What is myeloblastic leukemia and how does it develop?
The pathology occurs in the bone marrow, the tissue of which produces blood cells, platelets, leukocytes and red blood cells, which allow our body to function normally. Acute myeloblastic leukemia, AML, as the disease is called for short, originates from myeloblasts, immature stem cells, the further activity of which is already programmed: after maturation, they will have to perform the functions of granulocytes, granular leukocytes.
Defective damage to these progenitor cells leads to their mutation, resulting in the following:
- The maturation of leukocytes stops at the initial level and they, instead of turning into full-fledged blood cells, acquire a tendency to active and uncontrolled division.
- The appearance of numerous clones contributes to the rapid increase in the so-called tumor structure of the blood, which leads to inhibition and displacement of healthy blood cells.
- Mutated leukocytes fill the bloodstream and are transported through the bloodstream to the most distant parts of the body, forming numerous secondary foci.
Oncology of this type, which is sometimes called blood cancer, which is partly incorrect (the fluid environment of the body is affected by cancer, and not epithelial tissue, as occurs with the development of cancerous tumors) disrupts the functioning of the immune system and causes serious disruptions in the functioning of the entire body.
Diagnosis of acute leukemia
Often, acute leukemia is detected by the results of a blood test when a patient visits for another reason - the leukocyte formula reveals a so-called blast crisis, or leukocyte failure (lack of intermediate forms of cells). Changes are also observed in the peripheral blood: in most cases, patients with acute leukemia develop anemia with a sharp decrease in red blood cells and hemoglobin. There is a drop in platelet levels.
As for leukocytes, two options can be observed here: both leukopenia (decrease in the level of leukocytes in the peripheral blood) and leukocytosis (increase in the level of these cells). As a rule, pathological immature cells are also found in the blood, but they may be absent; their absence cannot be a reason to exclude the diagnosis of acute leukemia. Leukemia in which a large number of blast cells are found in the blood is called leukemic, and leukemia with the absence of blast cells is called aleukemic.
Red bone marrow examination is the most important and accurate method for diagnosing acute leukemia. The disease is characterized by a specific picture - an increase in the level of blast cells and inhibition of the formation of red blood cells.
Unlike other diseases, acute and chronic are different types of leukemia and do not transform into one another (i.e., chronic leukemia is not a continuation of acute, but a separate type of disease).
Another important diagnostic method is bone biopsy. Bone sections are sent for a biopsy, which reveals blastic hyperplasia of the red bone marrow and thus confirms the disease.
Acute myeloblastic leukemia in children
For a small child, the acute type of this type of disease is not typical, but still, in the clinical practice of hemato-oncologists, there is information about acute childhood myeloblastic leukemia. The incidence of this type of cancer of the hematopoietic system in young patients is only 15% of all malignant blood pathologies.
Acute myeloblastic leukemia is very dangerous for children, because mutated cells do not stay in the bloodstream, but affect the entire body of the child, which leads to a number of negative, often irreversible phenomena:
- there is a significant decrease in immunity;
- there are malfunctions in the functioning of internal organs;
- diseases develop that can cause premature death.
Important! Any mother has a chance to prevent the development of acute leukemia in her baby. To achieve your goal, you need to be more attentive to your health during the period of bearing a child, regularly undergo scheduled medical examinations, say goodbye to bad habits and start leading a healthy lifestyle.
Reasons for development
The exact reasons for the formation of ML are unknown. Scientists were able to find out the factors leading to the active development of the disease. These can be called:
- Preleukemic pathologies of the hematopoietic system such as myelodysplastic or myeloproliferative syndromes. The risk may increase or decrease depending on the form of the syndrome.
- Patient's history of chemotherapy. The risk increases if chemotherapy was given less than 5 years ago.
- Ionizing radiation.
- Genetic mutations of the fetus, for example, Down syndrome and the like.
- Impact of biological mutagens on the mother's body during pregnancy.
Predisposition to myeloblastic leukemia is also of great importance. If any of your relatives have a family history of the disease, it is highly likely to appear in future generations.
Classification of the disease
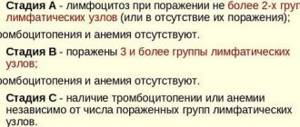
In order to completely cure acute leukemia caused by a mutation of myeloblasts, or to achieve a state of long-term stable remission, it is necessary to most accurately identify the form of the disease that affects a person. In clinical practice, hemato-oncologists use a unified classification, the purpose of which is more effective practical application. It takes into account the main signs of the disease that have prognostic value. According to this classification, AML is divided into 7 types, identified based on the nature of the course. But usually in everyday clinical practice a simplified version is used.
According to it, myeloblastic leukemia, which occurs in an acute form, is divided into 5 main subtypes:
- myeloid monocytic;
- megakaryocytic;
- monocytic;
- myeloid;
- erythroid.
Acute myeloblastic leukemia of any of these subtypes develops outside the age category, but has one feature - the older the person, the greater his chances of developing such a cancer.
Is it possible to be cured?
Despite the complexity and transience of this disease, there is still a chance for a complete recovery, albeit not great.
For example, the chronic form of myeloblastic leukemia was the first type of blood cancer for which comprehensive targeted treatment was developed. Thanks to new technologies, it is possible to achieve a complete cure much more often.
As for acute myeloid leukemia, the main methods of treatment still remain:
- chemotherapy,
- drug therapy,
- stem cell transplantation.
Attention! The problem with the last most effective method is finding a suitable donor, high cost and long queues. Since with myeloid leukemia the count is not months, but days, many patients do not even have time to wait for their turn.
In addition, the search for a donor is carried out by the patient’s family, and not by the medical institution. With all this, if the transplantation itself is paid for by the state, then paying for the transportation of the material is the task of the patient and his family.
In Russia, the bone marrow bank is very scarce, so it is often necessary to bring material from Europe, the USA and other countries, which can cost an amount that is unaffordable for ordinary families.
In other words, bone marrow transplantation increases the chances of a full recovery, but the ability to quickly find a donor and funds for transplantation (transportation, rehabilitation), especially without a waiting list, is practically absent.
Reference! The probability of a complete cure in clinical settings without bone marrow transplantation reaches 20-45%, provided that leukemia was detected at stages I or II.
Relapses most often occur directly during treatment or recovery (within 100 days after the course of therapy). With remission lasting 5 years, relapses are very rare.
Reasons that provoke the development of myeloblastic leukemia
No one can say exactly what exactly can trigger the pathological process of deformation in the DNA structure of bone marrow stem cells, as a result of which acute myeloblastic leukemia can begin to develop. This fact, despite numerous studies, remains unknown to science today. But scientists studying hematological and oncological diseases have accurately identified several risk factors, under the influence of which acute leukemia has a high chance of inception and rapid progression.
The main reasons contributing to the launch of the pathological process lie in the following:
- Long-term exposure to radiation or electromagnetic radiation. Under the influence of high-frequency rays, gene and chromosomal disturbances occur in cellular structures, which provokes the onset of mutation in cells and their further malignancy.
- A number of viruses that cause the development of certain diseases. Most often, the negative role of herpes, Epstein-Barr, and influenza viruses is noted. In total, more than a hundred pathogenic microorganisms are blastomogenic. They penetrate the blast hematopoietic cell and cause a mutation in it, as a result of which a person begins to develop acute leukemia of one type or another.
- Exposure to certain groups of drugs. Most often, the provocateurs of blood diseases are cytostatics, which have increased toxicity, or certain groups of antibiotics when used uncontrolled.
But the main reasons, according to most scientists, lie in hereditary factors and genetic predisposition. Those people with a family history of blood cancer have a higher risk of experiencing the painful symptoms of acute myeloid leukemia.
Important! Oncologists strongly recommend that everyone who has anything to do with the listed risk groups be more attentive to their well-being, regularly, for preventive purposes, visit a hematologist and donate blood. It is this analysis that will help to timely detect the onset of the process of malignancy in hematopoietic structures.
Causes
The cause of impaired hematopoiesis is currently considered to be a change in the composition and structure of human chromosomes. It can occur in children and adults under the influence of mutagenic factors:
- radiation emission;
- distribution of chemical agents, especially benzene, in the paint and varnish industry, during leather dressing;
- treatment with cytostatic drugs and immunosuppressants;
- hereditary instability of myelocytes.
Clinical manifestations, symptoms and course depend on the form of the disease.
Symptoms and manifestations of myeloblastic leukemia
The danger posed by acute leukemia, which occurs due to deformation of the DNA of myeloblast stem cells, lies in the blurred, asymptomatic initial stage of development. Most patients for a long time are not bothered by symptoms of mild malaise, which indirectly indicate the development of myeloblastic leukemia. Sometimes a person feels signs of ill health, but they are so nonspecific and similar to a common cold that they do not cause alarm. The patient does not strive to visit a doctor, but tries to relieve cold symptoms on his own, and acute myeloblastic leukemia is actively progressing at this time.
The transition of the disease to an advanced stage, treatment for which is quite complex, and the chances of survival are significantly reduced, is accompanied by more severe symptoms.
The main symptoms of an actively progressing disease are manifested by five main syndromes for blood oncology:
- Hyperplastic. It is associated with the penetration of blast cells, immature precursors of blood cells, into the parenchyma of the liver and spleen, as well as intraperitoneal lymph nodes, causing their enlargement. Also during this period of disease development, specific symptoms of obstructive jaundice appear.
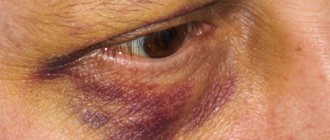
- Hemorrhagic. The manifestations of this syndrome are varied. Their variability ranges from the appearance of single small subcutaneous spots to extensive rashes and bruises that suddenly appear without mechanical impact. Extensive internal and nasal bleeding occurs very often.
- Anemic. Pale skin, lethargy.
- Intoxicating. Increased temperature, loss of appetite, nausea, sometimes turning into vomiting, diarrhea.
- Infectious. They are characterized by an increase in the occurrence of fungal and bacterial infections. Purulent processes, stomatitis, pneumonia, and bronchitis become constant companions of cancer patients. The development of sepsis is noted.
If such symptoms appear, an emergency visit to the doctor is required. Only timely medical care will help save a person’s life.
Treatment
Basic treatment measures consist of chemotherapy. Chemotherapy can be combined with basic therapeutic methods, including diet, physical therapy and hardware blood purification.
Chemotherapy is divided into 2 stages: induction and consolidation. The first stage is designed to obtain stable remission, and the second is carried out with the aim of destroying residual pathological cells.
Induction therapy includes cytarabine and an anthracycline antibiotic such as daunrubicin. Statistics show that this method can cure slightly less than 70% of patients.
Induction therapy may also include regimens such as:
- FLAG;
- ADE;
- DAT;
- high-dose cytarabine monotherapy;
- new drugs being researched;
Upon achieving stable remission after induction therapy, doctors begin consolidating therapy.
The second stage is mandatory in most cases, since without it there is a high probability of relapse of the disease.
Consolidation therapy may consist of 2-5 courses of additional chemotherapy, allogeneic stem cell transplantation, and others.
Laboratory and instrumental diagnostic methods that help identify the disease
To make a diagnosis of myeloblastic leukemia, an acute type of course, it is necessary to carry out specific diagnostic measures.
Diagnosis of leukemia is as follows:
- blood tests that detect the presence of damaged leukocytes, red blood cells, platelets;
- histological examination, biopsy of tissue taken through fine-needle puncture from the pelvic bones.
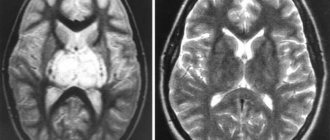
- radiography, ultrasound, CT, MRI of internal organs.
Diagnosis of this disease aims not only to clarify the nature of the course of myeloid leukemia, but also to exclude other diseases that have similar symptoms. Making a correct diagnosis is usually easy, especially if most of the healthy blood cells have already been destroyed.
Prognosis for myeloid leukemia
Currently, thanks to the use of modern drugs, the life prognosis for chronic myeloid leukemia has improved. With the use of new drugs, life expectancy for chronic myeloid leukemia in 90% of patients is at least 5 years. Most of them remain in normal health 10 years after completion of therapy.
But in general, both the life prognosis for acute myeloid leukemia and the prognosis for chronic myeloid leukemia depend on the stage of the disease. Life expectancy directly depends on the timeliness of the treatment started, as well as the correctness of its tactics.
Treatment methods for myeloblastic leukemia: medications, radiation, surgery
All treatment methods for myeloblastic leukemia are aimed at achieving long-term remission. They are selected for each patient individually, but the main place in them is occupied by chemotherapy. Drug antitumor therapy is carried out in 2 stages: induction, aimed at maximum destruction of mutated myeloblastic type cells, and prophylactic. In the majority of patients, induction therapy, which uses strong cytostatics Cytarabine, Doxorubicin and Daunorubicin, allows restoration of normal hematopoietic function and relief of cancer symptoms within several weeks. This allows specialists to say that myeloid leukemia has achieved conditional clinical remission.
Many patients, based on medical indications, are prescribed a bone marrow cell transplant. This operation is considered the most effective therapeutic method, but the final decision on its implementation is made solely by the patient and his relatives. Radiation is rarely used due to the large number of negative consequences of this procedure caused by the effects of radiation on the bone marrow. Alternative treatment should also be approached with caution. It is permissible only as an additional therapy to relieve negative symptoms.
Treatment of acute leukemia
Treatment of acute leukemia depends on several criteria: the patient’s age, his condition, and the stage of the disease. The treatment plan is drawn up for each patient individually.
The disease is mainly treated with chemotherapy. If it is ineffective, they resort to bone marrow transplantation.
Chemotherapy consists of two sequential steps:
- stage of induction of remission - they achieve a decrease in blast cells in the blood;
- consolidation stage – necessary to destroy remaining cancer cells.
This may be followed by a reinduction of the first step.
The average duration of treatment for acute leukemia is two years.
A bone marrow transplant provides the patient with healthy stem cells. Transplantation consists of several stages.
- Search for a compatible donor, bone marrow collection.
- Patient preparation. During preparation, immunosuppressive therapy is administered. Its goal is to destroy leukemia cells and suppress the body’s defenses so that the risk of transplant rejection is minimal.
- The actual transplant. The procedure is similar to a blood transfusion.
- Bone marrow engraftment.
It takes about a year for the transplanted bone marrow to fully take root and begin to perform all its functions.
According to statistics, disease-free survival after bone marrow transplantation ranges from 29 to 67%, depending on the type of leukemia and some other factors.
Prognosis for recovery
For acute myeloid leukemia, long-term survival prognosis is unclear. Life expectancy after treatment depends on certain factors, the main of which is the patient’s age. The best prognosis is observed in children. Adequately administered therapy allows 70% of babies to count on five-year survival while maintaining quality of life.
Adult patients have a poorer prognosis for achieving stable remission:
- elderly patients over 65 years of age reach the five-year mark only in 15-25% of cases;
- middle age (40-45 years) gives a chance for long-term remission to 50% of cancer patients;
- The most unfavorable prognosis for myeloid leukemia is observed in AML with chromosomal mutations occurring in chromosomes 3, 5 and 7. This pathological condition in 85% of cases leads to relapse of the disease and subsequent death in the first 2-3 years after treatment.
Worth knowing! No statistics can tell how myeloblastic leukemia, which has an acute type of course, will end for the patient. Even if cancer patients have a favorable prognosis for recovery, this does not mean anything. In clinical practice, a large number of cases have been recorded where a minor error in the therapeutic course led a person to premature death. Therefore, during antitumor therapy, it is necessary to unquestioningly follow all the specialist’s instructions. Only strict implementation of the treatment measures prescribed by the doctor will help increase survival and prolong life as much as possible.
Prognosis for myeloma
Multiple myeloma is also a disease called blood cancer. It develops from plasma cells, which are a type of white blood cell that helps the body fight infection. In multiple myeloma, cancer cells grow in the red bone marrow. They produce abnormal proteins that damage the kidneys. Multiple myeloma affects multiple areas of the body.
Of course, most patients do not seek medical attention until signs of the disease develop. In 90% of patients, pain and bone brittleness initially appear. 95% of people pay attention to the increased frequency of infectious diseases and attacks of fever. 100% of people who seek medical help experience thirst and frequent urination. Weight loss, nausea and constipation affect 98% of myeloma patients.
Treatment of the disease includes chemotherapy, radiation treatment and plasmaphoresis. The chance of cure for 70% of patients is bone marrow or stem cell transplantation. Despite the successes of oncological hematology, as well as transplantation, the prognosis for this form of blood cancer is unfavorable.
There are 14 known variants of myeloma, but in 90% of cases leukemia and lymphoma are registered. The survival prognosis depends on many factors, however, we should not forget that the prognosis is based only on statistical data. The earlier the diagnosis is made and treatment started, the better the prognosis.
There are 4 stages of multiple myeloma. At an early stage of the disease, in 100% of patients it is not possible to detect any pathognomonic symptoms. Damage to bone tissue is not detected either. At the first stage, a small number of myeloma cells are found, and in 97% of patients, minor damage to bone tissue is found.
The appearance of a moderate number of myeloma cells is interpreted as stage 2 of the disease. At the third stage of development of myeloma, in 100% of cases a large number of atypical cells and numerous damage to bone tissue are found. The prognosis for survival for a type of blood cancer such as myeloma is determined by the age of the patient. Young people are 2 times more responsive to treatment than older patients.
In 10% of cases, multiple myeloma is asymptomatic and progresses slowly. The prognosis worsens in 100% of persons with impaired renal function. However, the prognosis for recovery is 30% better in those patients who respond to therapy in the initial stage of the disease.
After treatment, 100% of patients require regular monitoring and examination. These people are advised to drink plenty of fluids to improve kidney function. Due to weakened immunity, they are forced to more carefully protect themselves from infectious diseases.
What is the life expectancy and predicted survival rate of patients suffering from myeloma? The studies provide an analysis of the survival rate of patients with myeloma compared with their peers who do not have the disease.
Table No. 2. Average life expectancy of patients with myeloma according to ACS (American Cancer Society).
Average life expectancy (in months)
source