Pancreatitis is inflammation of the pancreas, characterized by acute and chronic subtypes. The most important danger of the disease chronic pancreatitis is the independent digestion of the organ (self-destruction). During inflammation, pancreatic secretions are not distributed to the duodenum, but are activated in their own organ, and their independent digestion begins. Toxic substances and excess secretions are released into the body and damage the brain, lungs, liver, and kidneys.
The disease always occurs with pronounced symptoms, manifests itself in severe pain, and is characterized by a high probability of death.
Symptoms of chronic pancreatitis
Symptoms of chronic pancreatitis may vary depending on the stage (remission or exacerbation), course and physical condition of the patient. The main signs of the disease are as follows:
- acute pain without clear localization. Pain can be felt in the right hypochondrium, upper or middle abdomen and spread to the back. In many patients, pain occurs immediately after eating, especially if the diet contained fatty, smoked or spicy foods;
- frequent loose stools are one of the main signs of indigestion. Digestive problems in chronic pancreatitis are caused by a lack of enzymes;
- heaviness in the abdomen, nausea, which also indicate a lack of digestive enzymes;
- increasing feeling of hunger, muscle tremors, weakness, cold sweat;
- intoxication, manifested in fever, chronic fatigue, and a feeling of general malaise.
Classification of inflammatory processes
Doctors have a large number of ways to classify inflammation:
- The first classification was made in 1946: the development of chronic pancreatitis due to alcoholism.
- 1963 – pancreatitis, developing due to the peculiarities of morphological and etiological characteristics.
- New international systematization, 2007 - multiple risk factors M-ANNHEIM with a characteristic manifestation: acute recurrent, chronic, acute chronic.
Basically, the disease in the stage of chronic pancreatitis develops after an acute attack. The transformations from acute to chronic are conditional and appear more than six months after the onset of the disease.
Volume lesions (necrotic changes) of glandular tissue differ in the following types:
- edematous appearance – transformation of a single pancreatocyte without the appearance of necrotic areas;
- destructive – pancreatic necrosis multiple transformations;
- small focal - weak degree of pancreatic necrosis with focal damage to minimal areas;
- medium focal - average degree of damage;
- large focal lesion of the pancreas;
- total, subtotal pancreatic necrosis involving the entire territory of the pancreatic glandular space (head, body, process).
The degree of lethality varies:
- Early mortality due to the symptom of multiple organ failure is a severe nonspecific reaction of the body with a disorder of all microcirculations, metabolism, disruption of the functionality and structure of organs.
- Late mortality is due to long-term purulent septic lesions and complications of a destructive degree in purulent-necrotic parapancreatitis.
Causes of chronic pancreatitis
One of the most common causes of chronic pancreatitis is poor diet and unhealthy lifestyle. Constant overeating, abuse of fatty foods and alcohol cause blockage of the excretory ducts of the pancreas. Narrowed excretory ducts provoke the accumulation and premature activation of digestive enzymes. As a result, the pancreas actually begins to digest itself, and inflammation forms1.
In addition, the following factors can lead to chronic pancreatitis3:
- ulcer of the duodenum, stomach and enteritis. Chronic inflammation of the mucous membrane of the gastrointestinal tract makes it difficult to secrete pancreatic juice, which often causes chronic pancreatitis;
- cholelithiasis. After leaving the gallbladder, the stone causes blockage of the common duct and inflammation of the pancreas develops;
- genetic predisposition;
- toxic effects of drugs.
Causes and development of the disease
Most often, the causes of the disease are divided into two groups: internal and external.
READ Beneficial effects of chicory on pancreatitis
Exogenous or external causes of chronic pancreatitis:
- alcohol abuse;
- the presence in the diet of a large number of fried, salty and spicy foods;
- fast food and unhealthy snacks: chips, soda and crackers;
- poorly prepared dishes and products treated with chemicals;
- frequent smoking;
- long-term use of medications, in particular anti-inflammatory and diuretic drugs.
- staying in a room with a lot of chemicals.
Endogenous or internal causes of the disease:
- inflammatory diseases of the duodenum;
- injury or unsuccessful surgery;
- diseases of the connective tissue of the pancreas;
- genetic metabolic disorders.
The following reasons can lead to the appearance of obstructive pancreatitis:
- duodenitis;
- tumors in the pancreas area;
- stenosis or any inflammation of the major duodenal papilla - the main duct for transporting bile and pancreatic juice to the duodenum;
- a scar on an organ left after surgery or injury;
- pseudocyst in pancreatic tissue.
Video:
Toxic-metabolic pancreatitis can be provoked by the following reasons:
- chronic form of renal failure;
- too high calcium content in the body;
- hyperlipidemia – excessive levels of lipids or lipoproteins in the body;
- acid or alkali poisoning;
- alcohol poisoning.
The causes of idiopathic pancreatitis are not fully understood, but doctors identify some factors that can lead to the disease:
- hypercalcemia;
- violations of gene structure;
- dysfunction of the major duodenal papilla;
- small stones in the bile ducts;
- taking narcotic or toxic substances.
Chronic pancreatitis in children most often develops as a result of hereditary or autoimmune diseases.
Diagnosis of chronic pancreatitis
Identifying chronic pancreatitis can be difficult due to the nonspecific clinical picture. Nausea, abdominal pain, digestive problems - these symptoms are characteristic of many diseases, for example, stomach ulcers or chronic cholecystitis. Therefore, identifying the disease may require a whole range of studies. Diagnosis of chronic pancreatitis may include2,3:
- external examination of the patient. Chronic pancreatitis may be indicated by bluish areas of the skin on the front and side walls of the abdomen. In some patients, bright red patches of skin on the chest and back become noticeable. Palpation may reveal pain in the left hypochondrium and the upper third of the abdomen;
- a general and detailed blood test, which shows the presence of an inflammatory process, based on an increase in the concentration of leukocytes;
- laboratory blood test to identify markers of nutritional status;
- fecal elastase test;
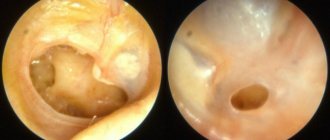
- ultrasonography. In some cases, ultrasound examination (ultrasound) can be performed through the walls of the stomach and duodenum, which significantly increases the accuracy of the examination. This method is called endoUS and combines the possibility of endoscopic and ultrasound diagnostics of the gastrointestinal tract (GIT);
- computed tomography: used to determine complications of pancreatitis associated with thickening of the pancreas tissue.
Diagnosis of the disease
Since in some cases the symptoms of pancreatitis and cholecystitis in women and men may coincide with signs of gastritis, in addition to analyzing the patient’s complaints, a diagnosis of chronic pancreatitis is carried out, including ultrasound and other numerous laboratory examinations.
Today, modern medicine includes more than 90 studies to establish and clarify the diagnosis of chronic pancreatitis.
Diagnosis of chronic pancreatitis and cholecystitis consists not only of ultrasound and a general blood test, but also of many other examinations that the patient must undergo before treating chronic pancreatitis.
Video:
Diagnostics mainly includes the following activities:
- a general blood test, through which you can find out about the presence of pancreatitis or cholecystitis in women and men. Signs of inflammatory changes are determined by changes in the number of leukocytes, an increase in the erythrocyte sedimentation rate, etc.;
- biochemical analysis allows you to determine the enzyme level of the pancreas in the blood;
- Urine and stool tests are performed to check for the presence of amylase and undigested food particles, respectively. If diabetes is suspected, the urine is also checked for the presence of glucose;
- Ultrasound is performed as the main examination for women, men and children. Ultrasound can detect damage to the pancreas and other organs of the digestive system;
- thanks to gastroscopy, the doctor can visually assess the depth and nature of inflammation from the inside;
- sometimes, if an ultrasound cannot be performed for some reason, then an X-ray of the gastrointestinal tract is performed;
- the ERCP procedure, like ultrasound, is indispensable for diagnosing pancreatitis;
- MRI is used to detect pathologies in muscles and organs;
- computed tomography is generally similar to ultrasound, but allows layer-by-layer scanning and evaluation of organs;
- regular functional tests.
Exacerbation of chronic pancreatitis
Chronic pancreatitis may hardly manifest itself until the period of exacerbation. Relapse of the disease is usually associated with two main reasons3:
- alcohol consumption. Even a small amount of alcohol consumed can provoke the transition of the disease into the acute phase;
- violation of the diet, overeating, a large number of fatty, fried, spicy dishes on the menu.
Other factors can also provoke exacerbation of chronic pancreatitis in adults, for example, chronic stress, physical fatigue, poisoning or the toxic effects of certain medications3.
Exacerbation of the disease is manifested by the following symptoms3:
- attack of acute or dull pain in the hypochondrium. Painful sensations spread to the subscapular region or the entire back;
- progressive diarrhea. In this case, the feces have a characteristic greasy shine. Undigested food remains are often observed in the stool;
- the occurrence of specific bitterness in the oral cavity, nausea and loss of appetite;
- whitish coating on the surface of the tongue;
- weight loss.
Exacerbation of chronic pancreatitis in adults can last for one to two weeks. You cannot fight the disease on your own during this period: the best solution is hospitalization and constant monitoring by specialists.
Causes of pathology
The pathogenesis of the disease has not yet been fully studied, but it has been precisely established that its key link is the replacement of the epithelial tissue of the pancreas with connective tissue. Untreated acute pancreatitis can become chronic, but most cases of the etiology of chronic pancreatitis are associated with alcohol abuse and cholelithiasis. From 30 to 60% of patients have alcoholic pancreatitis, mostly men. Inflammation due to gallbladder diseases occurs in 25-40% of cases.
Other predisposing factors of the disease:
- sphincter of Oddi insufficiency,
- cystic fibrosis,
- taking certain medications
- high concentration of calcium ions in the blood,
- hereditary and idiopathic pancreatitis.
Treatment of chronic pancreatitis
The answer to the question “how to cure chronic pancreatitis” remains open even for modern doctors. The treatment regimen is determined by the doctor for each individual case. The main thing is that therapy should be comprehensive, affecting the main cause of the disease.
Treatment of chronic pancreatitis includes2,3,4:
- immediate cessation of bad habits. Smoking and abuse of strong alcoholic beverages aggravate the inflammatory process and contribute to the subsequent development of the disease;
- strict adherence to the diet. The daily diet should contain high-calorie foods, without spicy foods, salt and pure sugar. You should eat food often, in small portions. In case of exacerbation of chronic pancreatitis, therapeutic fasting is prescribed, which will help stop pancreatic secretion and relieve pain. After 1-3 “hungry” days, the patient is transferred to a special diet;
- basic therapy. In this case, we are talking about taking the following type of drugs: antispasmodics and analgesics, antisecretory and detoxification drugs. Treatment is carried out under the supervision of a doctor with strict adherence to the instructions;
- taking enzyme preparations, the task of which is to compensate for the impaired functioning of the pancreas. The fact is that the pancreas does not recover (it is not the liver), and therefore will no longer be able to work at full capacity during chronic pancreatitis. That is why the first line of therapy is enzyme preparations, which should be taken for life. An example of an enzyme drug prescribed for chronic pancreatitis is Creon®;
- complex therapy. May include taking antispasmodics or analgesics, antisecretory and detoxification medications. Therapy is carried out under the supervision of a physician with strict adherence to the instructions;
- taking anti-inflammatory and painkillers that improve the patient’s well-being;
- herbal medicine, which can be prescribed during remission only as prescribed by a doctor.
What to do if an exacerbation of pancreatitis occurs suddenly, and the ambulance has not yet arrived? Before the doctors arrive, you need to lie down, try to relax your abdominal muscles as much as possible and apply a heating pad with cold water to the sore spot. You should not take painkillers or any other medications - this will interfere with correct diagnosis. And, of course, any food and drinks, even plain water, are strictly prohibited, because any food or liquid can cause increased pain3.
Treatment of the disease
To treat pancreatitis and cholecystitis at home, the doctor prescribes medications and also gives nutritional recommendations.
If you follow these recommendations, you can cure the disease, if not forever, then for quite a long time.
READ How does pancreatitis occur and how to treat it?
It is possible to completely restore damaged pancreatic tissue only in the initial stages of the disease.
Video:
Depending on how much time has passed since the onset of the disease in the absence of proper treatment, the chances of completely curing pancreatitis decrease.
Before using medications to cure the disease at home, ask your doctor for recommendations regarding hospitalization; perhaps in the later stages of pancreatitis or cholecystitis you should go to the hospital.
Drug treatment of chronic pancreatitis:
- painkillers are used to relieve acute pain in pancreatitis or cholecystitis, especially during exacerbation: Papaverine, No-Shpa, Atropine. Such drugs can only be used by adult men and women;
- proton pump blocker drugs can be used to reduce the activity of pancreatic enzymes: Omeprazole, Contrical and other drugs;
- drugs for the prevention of infectious diseases. Antibiotics such as Amoxicillin, Clarithromycin, Ampicillin are prescribed;
- enzyme preparations used in replacement therapy can restore the disturbed balance of enzymes and proteins. The following drugs are prescribed: Mezim, Creon, Festal, Digestal;
- to restore water and electrolyte balance, physiological and saline solutions are prescribed;
- To restore the level of vitamins and beneficial microelements in the body, especially after taking antibiotics, various multivitamin complexes are prescribed.
The drug Creon® 25000 for chronic pancreatitis
A decrease in pancreatic function inevitably leads to a lack of digestive enzymes in the body, the so-called enzyme deficiency. As a result, the quality of digestion suffers, and the body does not receive the necessary energy and nutrients for full functioning. Creon® is designed specifically to compensate for the lack of its own enzymes through their delivery from the outside and belongs to the group of enzyme preparations. The drug contains enzymes identical to those produced by the pancreas. The key feature is that the active ingredient Creon® is small particles - minimicrospheres, which are collected in a capsule. The fact is that science has been studying enzyme preparations for more than 100 years in order to increase their effectiveness. To date, scientific advances indicate that preparations with particles whose size does not exceed 2 mm4.5 can most accurately recreate the natural process of digestion. Moreover, it has been scientifically proven that the smaller the particles of the drug, the more effective it can be4,6.
Creon® is the only drug whose capsule contains hundreds of small particles - minimicrospheres7. Their size does not exceed 2 mm, which is recorded as recommended in world and Russian scientific works4,5,6.
Modern classification
There is no general classification system for the disease. There are many classifications of pancreatitis . The Marseille-Roman classification of chronic pancreatitis was used for a long time:
- Calcifying (chronic calculous pancreatitis).
- Obstructive.
- Parenchymatous-fibrous.
- Chronic cysts and pseudocysts.
There is an International Classification of Diseases. Chronic pancreatitis has a code according to ICD-10:
- Code K86.0 – alcoholic chronic pancreatitis.
- Code K86.1 – other types of chronic pancreatitis (infectious, recurrent, unidentified).
The main forms of CP according to Khazanov:
- Interstitial, or edematous . The form of the disease resembles acute pancreatitis, lasting longer than 6 months. Clinic: acute pain, nausea, vomiting.
- Parenchymatous, or recurrent . This form of chronic pancreatitis occurs most often - in half of the patients. Attacks of the disease occur several times a year, but the clinical manifestations are not as pronounced as with the edematous form.
- Fibrous-sclerotic, or indurative . Diagnosed in 15% of patients with CP. It is characterized by severe constant pain, but the overall level of amylase is not very high. The course of the disease is progressive, complications occur in half of the cases of this form of the disease.
- Cystic . It is characterized by great pain and intoxication during the period of exacerbation. Amylase levels are very high, both in the blood and urine. During an exacerbation, the pancreas can be easily palpated. Ultrasound and CT visualize small cysts of about 1.5 cm.
- Hyperplastic, or pseudotumor (pseudotumor) . Ultrasound and CT scans show an increase in the affected part of the organ, most often the head. Localization of pain in this case is in the epigastrium. About 5% of patients who went to the hospital suffer from the pseudotumor form of pancreatitis (chronic).
Depending on the course of the disease, chronic pancreatitis is distinguished:
- Easy . Exacerbations occur 1-2 times a year, the pain is well relieved with antispasmodics and analgesics. The functioning of the gland is practically not impaired, weight loss is not observed. The coprogram is normal.
- Average . Relapses occur 3-4 times a year and are characterized by persistent pain, with excessive fermentation. The internal and external secretion of the gland is slightly impaired.
- Heavy . Constant exacerbations with progressive pain. Dyspepsia syndromes are observed even without exacerbations. Pancreatic diarrhea and pancreatogenic diabetes are noted.
There is a clinical and morphological classification by Ivashkin and co-authors, which is used in domestic medicine. According to it, pancreatitis (chron.) is distinguished depending on:
1. morphological features:
- hydropic;
- chronic parenchymal pancreatitis;
- fibrous-sclerotic (with proliferation of connective tissue);
- pseudotumor;
- cystic.
2. clinical manifestations:
- painful form;
- hidden – without pain;
- hyposecretory – CP with exocrine insufficiency;
- hypochondriacal – CP with a predominance of psychoneurological symptoms;
- combined.
3. course of the disease:
- rarely repeated;
- often recurrent;
- persistent - constantly flowing.
4. etiology:
- drug;
- biliary;
- idiopathic – with complete loss of secretory functions;
- dysmetabolic – diabetes mellitus, hyperparathyroidism;
- alcoholic;
- infectious.
5. complications:
- disruption of the outflow of pancreatic, stomach, and liver juices;
- infectious – abscesses, cholangitis;
- disruptions in the endocrine system - hypoglycemia, diabetes;
- bleeding of the upper gastrointestinal tract, renal failure, enzymatic cholecystitis, erosive esophagitis.
The existing concept of “reactive pancreatitis” is not highlighted in the classification . This term summarizes the responses of the pancreas to provoking factors - food or drug poisoning, an infectious disease.
What else is important to know about enzyme preparations?
The minimum starting dosage is Creon® 25,000 units, which is stated in Russian recommendations for the treatment of chronic pancreatitis and exocrine pancreatic insufficiency2,5. The number indicates the amount of the enzyme lipase, which helps digest fats. If necessary, the doctor can increase the dosage; in European practice, the required dose per single dose can reach up to 80,000 units8. By comparison, the pancreas of a healthy person produces up to 720,000 of these units during each meal9.
Therapy should be taken seriously, since high-quality “nutrition” of the body is the key to its functioning. How long can a person live without energy from food? With chronic pancreatitis, the body must be supplied with enzymes at every meal, even with a snack. Thus, in accordance with the instructions for the drug Creon®, a full dose is required for a meal (for example, 25,000 units), and half for a snack. Creon® capsules are convenient to use: you can open them and add minimicrospheres to food, thereby selecting the desired dose10. More information about the admission rules can be found here.
- Maev I.V., Kazyulin A.N., Samsonov A.A., Kucheryavyi Yu.A. Chronic pancreatitis: (Algorithm for diagnosis and treatment tactics). A manual for general practitioners, therapists, gastroenterologists: A textbook. – M.: GOU VUNMTs MH and SR RF, 2006. – p. 104.
- Ivashkin V.T., Maev I.V., Okhlobystin A.V. et al. Recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of chronic pancreatitis // RZHGGK 2014, 4 – P.70-97.
- Maev I.V., Kucheryavyi Yu.A. Diseases of the pancreas: a practical guide. - M: GEOTAR-Media 2009; 736 pp.
- Löhr JM et al.; HaPanEU/UEG Working Group. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J. 2020 Mar;5(2):153-199.
- Ivashkin V.T., Maev I.V., Okhlobystin A.V. et al. Recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of EPI. REGGK, 2018; 28(2): 72-100.
- Löhr Johannes-Matthias, et. al. Properties of different pancreatin preparations used in pancreatic exocrine insufficiency. Eur J Gastroenterol Hepatol.2009;21(9):1024-31.
- According to the State Register of Medicines https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=cb656520-2b07-46f1-8370-16f5e075bb34&t=, accessed 03/04/2020
- Dominguez-Muñoz JE. Diagnosis and treatment of pancreatic exocrine insufciency. Curr Opin Gastroenterol. 2018;34(5):349-354
- Keller J., Layer P. Human pancreatic exocrine response. to nutrients in health and disease. Gut 2005;54(Suppl 6):vi1-28. 10.1136/gut.2005.065946.
- Instructions for medical use of the drug Creon® 10000, enteric capsules, dated 05/11/2018.
RUS237768-2 from 04/23/2020
Classification
There are several types of chronic pancreatitis.
According to the localization of the inflammatory process:
- limited,
- diffuse.
By origin (classification by M.I. Kuzin):
- primary (idiopathic, alcoholic, medicinal, but due to nutritional disorders),
- post-traumatic occurs due to injuries of the pancreas, after operations,
- secondary result of other diseases.
Find out the instructions for using the drug Propicil for the treatment and prevention of thyroid diseases.
Read about the causes of hypothyroidism in men, as well as the treatment features of the disease at this address.
By severity:
- easy,
- moderate severity,
- heavy.
According to symptoms:
- pain (recurrent, constant),
- latent,
- mixed.
Chronic pancreatitis in adults is characterized by cyclical stages of exacerbation, remission and unstable remission.
Possible complications
In clinical practice, the most common types of complications of pancreatitis are:
- Pancreatic abscess is an accumulation of pus in the tissues. Develops in the presence of necrotic phenomena and the addition of infection, most often in the second week of illness.
- Ascites is the result of pancreatic juice, rich in enzymes, entering the lesser omentum of the intestine and the abdominal cavity, where a large amount of exudate accumulates.
- Narrowing of the common bile duct is a consequence of swelling of the head of the pancreas, leading to the appearance of mechanical jaundice.
- Gastrointestinal bleeding – develops when pancreatic cysts rupture, as well as during exacerbation of diseases accompanying pancreatitis. Lead to the appearance of internal bleeding and require surgical intervention.
Other complications may occur, but the above list includes those most commonly encountered by practitioners.
Diagnostics
Diagnosis of inflammation of the pancreas is carried out on the basis of anamnesis and clinical picture, laboratory and instrumental studies. The purpose of examining the patient is not only to identify the fact of inflammation, but also to determine the level of its intensity, as well as differential diagnosis with diseases such as:
- cholecystitis;
- colitis;
- enteritis;
- ischemic syndrome;
- pancreas cancer.
Anamnesis collection and objective examination are carried out by a doctor immediately after hospitalization of the patient. At the same time, he manages to identify the symptoms of pancreatitis given above. Typically, the patient reports recent consumption of irritating foods or alcohol, complains of pain, and assumes a forced position (sitting, leaning forward).
Laboratory tests (general and biochemical blood tests) indicate an increase in ESR, leukocytosis and other signs of the inflammatory process. A study of the secretion of pancreatic enzymes confirms changes in this indicator down or up (perulein test, lund test). A stool examination within 3 days reveals polyfecal matter (the examination is not carried out for diarrhea).
Note: patients with chronic pancreatitis must undergo a blood sugar test. In this case, biomaterial is collected every 3 hours, throughout the day. A double-humped glycemic curve indicates endocrine insufficiency, characteristic of diabetes mellitus.
Diet for chronic and acute pancreatitis of the pancreas in adults
An important condition for the nutrition of patients with acute or chronic pancreatitis is that foods should not stimulate the secretion of gastric juice. In case of severe exacerbations and acute forms of the disease, patients are prescribed fasting for 3-5 days. During this time, parenteral nutrition methods can be used, but no food should be allowed into the stomach. Subsequently, the patient is allowed to eat normally.
Alcohol, spicy, sour, salty, fried, and stewed foods are strictly contraindicated for a patient with pancreatitis. It is not recommended to eat fats and foods rich in calcium. The patient's diet should include boiled meat, eggs, cereals and slimy soups, dried bread or dry biscuits. The total amount of protein, fat and carbohydrates should be 120:80:400 grams respectively.
Patients are fed in fractions: food is taken 5-6 times in small portions, accompanying each trip to the canteen with an enzymatic drug prescribed by the doctor. If the condition worsens after consuming a particular product, you should exclude it from the diet.
Treatment of pancreatitis in adults
Treatment of pancreatitis is carried out in a hospital setting.
In this case, therapy pursues the following goals:
- decreased pancreatic secretion;
- pain relief;
- prevention of complications;
- replacement therapy with enzymes.
Treatment consists of two important components: pharmacological correction of the condition and diet. It is permissible to use traditional medicine recipes as an auxiliary technique.
Drugs for treatment
The following medications are used for treatment:
| Pharmacological group | Name | Dosage and regimen | Expected pharmacological action |
| Histamine H2 receptor blockers | Ranitidine | 150 mg/2 times a day, course up to 4 weeks | Decreased secretion of hydrochloric acid in the stomach |
| Famotidine | 40 mg/2 times a day, course up to 4 weeks | ||
| Proteolysis inhibitors | Gordoks | 100,000 units/day 1 week | Suppression of pancreatic enzyme activity |
| Contrikal | 40,000 units/day 1 week | ||
| Nonsteroidal anti-inflammatory drugs | Analgin | 1 t/3 times a day, until severe pain disappears | Analgesic effect, reduced release of inflammatory mediators |
| Ketorol | 1 t/3 times a day, until severe pain disappears | ||
| Enzyme preparations | Lipase | 30,000 units after each meal. Lifelong course | Correction of steatorrhea, participation in the digestive process |
| Pancreatin | 4 capsules per day, 1 after each meal. Lifelong course. |
According to indications, the patient may be prescribed drugs from the group of antispasmodics (no-spa, papaverine), antiemetics (cerucal), hemostatic drugs (aminocaproic acid).
Folk remedies
To reduce pain, as well as to speed up recovery processes, the following traditional medicine recipes can be used:
- Potato and carrot juice: 3 potatoes and 2 carrots are washed, peeled and passed through a juicer. The resulting juice is drunk immediately; it cannot be stored. The product is taken in courses of one week. The total number of courses reaches 3, the break between them is a week. You should drink juice half an hour before meals.
- Barberry root tincture: 100 grams of root is poured with one and a half liters of vodka, infused in a dark place for a month. After preparation, the medicine is filtered through a fine sieve and taken a tablespoon before meals. The course of treatment is 2-4 weeks.
- Oat decoction: a glass of cereal is ground using a meat grinder or coffee grinder. After this, the raw material is poured with a liter of water. The mixture is boiled for 10 minutes, cooled and drunk half a glass before each meal. The course of treatment is until the symptoms of the disease disappear.
Do not forget that the basis of treatment for pancreatitis is drug therapy and diet prescribed by a doctor. The following recipes should only be used after consulting a doctor.