Author's rating
Author of the article
Green Elena Stanislavovna
Otolaryngologist of the second category
Articles written
665
about the author
Sinusitis refers to ENT diseases in which there is an accumulation of purulent contents in the maxillary sinuses. To overcome the disease, it is necessary to take antibacterial agents. Nowadays, there are modern drugs of a new generation that cause a minimum of adverse reactions and effectively cope with the disease in a few days. Patients are often prescribed Cefotaxime for sinusitis.
Pharmacological action[ | ]
The drug is effective against many gram-positive bacteria and has high activity against gram-negative bacteria. It has a bactericidal effect on strains of bacteria resistant to penicillin, aminoglycosides, and sulfonamides. The mechanism of the antimicrobial action of Cefotaxime is associated with inhibition of the activity of the transpeptidase enzyme by blockade of peptidoglycan, disruption of the formation of mucopeptide in the cell wall of microorganisms. The drug is resistant to four of the five beta-lactamases of gram-negative bacteria and penicillinase of staphylococci. Active against Staphylococcus aureus
, including penicillinase-producing
Staphylococcus epidermidis
, some strains of
Enterococcus
spp.,
Streptococcus pneumoniae
(especially
Diplococcus pneumoniae
),
Streptococcus pyogenes
(group A beta-hemolytic streptococci),
Streptococcus agalactiae
(group B streptococci),
Bacillus subtilis
,
Bacillus myroides
,
Corinebacterium diphtheriae
,
Erysipelothrix insidiosa
,
Eubacterium
,
Enterobacter aerogenes
,
Enterobacter cloacae
,
Escherichia coli
,
Acinetobacter
spp.,
Haemophilus influenzae
, including ampicillin-resistant strains,
Haemophilus parainfluenzae
,
Klebsiella oxytoca
,
Klebsiella pneumoniae
,
Morganellamorganii
,
Neisseria meningitidis
,
Neisseria gonorrhoeae
, including strains that produce penicillinase,
Propionibacterium
,
Proteus mirabilis
,
Proteus vulgaris
,
Proteus inconstans
,
Serratia
spp.,
Viellonella
,
Yersinia
,
Bordetella pertussis
,
Moraxella
,
Aeromonas hydrophilia
,
Fusobacterium
,
Bacteroides
spp.,
Clostrridium species
,
Peptosteptococcus species
,
Pepto cocus
spp.
Has inconsistent effects on some strains of Pseudomonas aeruginosa
,
Acinetobactery
,
Helicobacter pylori
,
Bacteroidesfragtlis
,
Clostridiun diffcile
. It can act on multi-resistant strains that are resistant to penicillinase, first-generation cephalosporins, and aminoglycosides. The drug is less active against gram-negative cocci than first and second generation cephalosporins.
Cefotaxime
- pharmachologic effect
- Indications for use
- Mode of application
- Side effects
- Contraindications
- Pregnancy
- Interaction with other drugs
- Overdose
- Release form
- Storage conditions
- Compound
Cefotaximum
pharmachologic effect
Cefotaxime is a semisynthetic antibiotic of the third generation cephalosporin group, with a broad spectrum of action, for parenteral administration. The drug is effective against many gram-positive bacteria and has high activity against gram-negative bacteria. It has a bactericidal effect on strains of bacteria resistant to penicillin, aminoglycosides, and sulfonamides. The mechanism of the antimicrobial action of Cefotaxime is associated with inhibition of the activity of the transpeptidase enzyme by blockade of peptidoglycan, disruption of the formation of mucopeptide in the cell wall of microorganisms. The drug is resistant to four of the five beta-lactamases of gram-negative bacteria and penicillinase of staphylococci. Active against Staphylococcus aureus, including those producing penicillinase, Staphylococcus epidermidis, some strains of Enterococcus spp., Streptococcus pneumoniae (especially Diplococcus pneumoniae), Streptococcus pyogenes (beta-hemolytic streptococci of group A), Streptococcus agalactiae (streptococci of group B) , Bacillus subtilis, Bacillus myroides, Corinebacterium diphtheriae, Erysipelo-thrix insidiosa, Eubacterium, Enterobacter aerogenes, Enterobacter cloacae, Escherichia coli, Acinetobacter spp., Haemophilus influenzae, including ampicillin-resistant strains, Haemophilus parainfluenzae, Klebsiella oxytoca, Klebsiella pneumonia e, Morganellamorganii, Neisseria meningitidis, Neisseria gonorrhoeae, including strains that produce penicillinase, Propionibacterium, Proteus mirabilis, Proteus vulgaris, Proteus inconstans, Serratia spp., Viellonella, Yersitia, Bordetella pertussis, Moraxella, Aeromonas hydrophilia, Fusobacterium, Bacteroides spp., Clostrridium species , Peptosteptococcus species, Peptococcus spp. Inconsistently affects some strains of Pseudomonas aeruginosa, Acinetobactery, Helicobacter pylori, Bacteroidesfragtlis, Clostridiun diffcile. It can act on multi-resistant strains that are resistant to penicillinase, first-generation cephalosporins, and aminoglycosides. The drug is less active against gram-negative cocci than first and second generation cephalosporins.
Pharmacokinetics
The maximum concentration in the blood (11 and 21 mcg/ml) after intramuscular administration in doses of 0.5 g and 1 g, respectively, is observed 30 minutes after injection. 5 minutes after intravenous administration of 0.5 g, 1 or 2 g, the maximum concentration in the blood is 24, 39, 100 mcg/ml, respectively. In the blood, the drug is 25-40% bound to proteins. The bactericidal concentration in the blood remains for more than 12 hours. The drug penetrates well into tissues (creates an effective concentration in the myocardium, bone tissue, gall bladder, skin, soft tissues), body fluids (determined in effective concentrations in the spinal, pericardial, pleural, peritoneal, synovial fluids), passes through the placenta, penetrates into breast milk. Cefotaxime-BCPZ is excreted in significant amounts in the urine (90%) (in unchanged form about 60-70% and in the form of active metabolites about 20-30%, of which 15-20% are the main metabolite - desacetylcefotaxime, which has antimicrobial activity) . The half-life for intravenous administration is 1 hour, for intramuscular administration it is 1-1.5 hours. With repeated intravenous administrations at a dose of 1 g every 6 hours for 14 days, no accumulation is observed. In newborns, the half-life is 0.75-1.5 hours, in premature infants - up to 6.4 hours, in patients over 80 years old - 2.5 hours, in case of renal failure, the half-life does not exceed 2.5 hours. The drug is partially excreted in bile and breast milk.
Indications for use
Cefotaxime is prescribed for infections caused by microorganisms sensitive to it: infections of the lower respiratory tract (bronchitis, pneumonia, pleurisy, abscesses) and urinary tract; kidney; infections of the ear, nose, throat (sore throat, otitis, with the exception of enterococcal); with septicemia; endocarditis; infections of bones and soft tissues, abdominal cavity; for gynecological infectious diseases (uncomplicated gonorrhea, chlamydia); bacterial meningitis (except listeria); Lyme disease, as well as for the prevention of post-operative infections and complications.
Mode of application
Cefotaxime is prescribed intramuscularly and intravenously, by stream and drip. For intramuscular injections, dissolve 0.5 g (1 g) of Cefotaxime in 2-3 ml (4-5 ml) of sterile water for injection and inject deeply into the gluteal muscle.
For intravenous administration, first dissolve 0.5 g (1 g) of Cefotaxime in 2 ml (4 ml) of sterile water for injection, adjust the solvent to 10 ml and administer slowly over 3-5 minutes. For drip administration into a vein (over 50-60 minutes), dissolve 2 g of the drug in 100 ml of isotonic sodium chloride solution or 5% glucose solution. A single dose of Cefotaxime for adults is 1 g, every 12 hours; in severe cases, the dose is increased to 2.0 g, every 12 hours, or the number of injections is increased to 3-4 times a day, bringing the total daily dose to a maximum of 12 g In case of renal failure, the dose is reduced by 2 times.
For acute gonorrhea, the drug is administered once, intramuscularly, in a dose of 0.5-1 g. To prevent infectious complications, 0.5-1 g is administered before or during induction of anesthesia; if necessary, the injection is repeated after 6-12 hours.
Side effects
After the administration of Cefotaxime, allergic reactions may appear (rashes, hyperemia, exudative erythema multiforme, fever, eosinophilia, anaphylactic reactions, in rare cases - anaphylactic shock), nausea, vomiting, diarrhea, abdominal pain, dysbacteriosis, superinfection, rarely - pseudomembranous colitis. Indicators, including biochemical ones, of peripheral blood change (neutropenia, transient leukopenia, thrombocytopenia, hemolytic anemia, arrhythmia (with rapid jet injection), headache, reversible encephalopathy, pain at the injection site, tissue inflammation, phlebitis.
Contraindications
Hypersensitivity to any cephalosporin antibiotic and to penicillin; bleeding; history of enterocolitis; pregnancy. Caution must be exercised when prescribing the drug to patients with impaired renal and liver function.
Pregnancy
During pregnancy and breastfeeding, use only according to strict indications.
Interaction with other drugs
With the simultaneous use of Cefotaxime and aminoglycosides, “loop” diuretics, an increase in nephrotoxicity is observed. When administered simultaneously with antiplatelet agents, including non-steroidal anti-inflammatory drugs, the risk of bleeding increases. Probenecid slows excretion, increases plasma concentrations and half-life. Cefotaxime should not be administered in the same syringe with other drugs due to the possibility of interaction.
Overdose
An overdose can cause allergic reactions, dysbacteriosis, and encephalopathy.
Treatment: desensitizing drugs, symptomatic drugs.
Release form
Powder for the preparation of solution for injection in bottles of 0.5, 1.0 or 2.0 g.
Storage conditions
Store in a dry place, protected from light and out of reach of children, at a temperature not exceeding 25 °C. Shelf life: 2 years.
Dispensing conditions from pharmacies are by prescription.
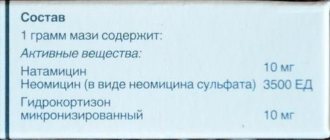
Compound
Cefotaxime;
sodium (6R,7R)-3-[(acetyloxy)methyl]-7-[[(Z)-2-(2-aminothiazol-4-yl)-2-(methoxyimino) acetyl]amino]-8-oxo- 5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylate;
The powder is white or white with a slightly yellowish tint, hygroscopic.
1 bottle contains sterile cefotaxime sodium salt in terms of cefotaxime 0.5, 1.0 or 2.0 g.
Additionally:
Cefotaxime should be prescribed with caution to patients with allergies, including to medications. When treating during lactation, it is necessary to stop feeding. Concomitant use of Cefotaxime with nephrotoxic drugs requires monitoring of renal function; When using the drug for more than 10 days, monitoring of peripheral blood is necessary. Elderly and debilitated patients should be prescribed vitamin K preparations (prevention of hypocoagulation). If a symptom of pseudomembranous colitis is established, Cefotaxime should be discontinued. For children under 2.5 years of age, the drug is administered intravenously. The dose of Cefotaxime for infants and young children is 50-100 mg/kg body weight per day, divided into separate doses, at intervals of 12 to 6 hours. For premature infants, the daily dose should not exceed 50 mg/kg body weight.
Attention
Before using Cefotaxime you should consult your doctor. This instruction is given in free translation and is intended for informational purposes only. For more complete information, please refer to the manufacturer's instructions.
Pharmacokinetics[ | ]
The maximum concentration in the blood (11 and 21 mcg/ml) after intramuscular administration in doses of 0.5 g and 1 g, respectively, is observed 30 minutes after injection. 5 minutes after intravenous administration of 0.5 g, 1 or 2 g, the maximum concentration in the blood is 24, 39, 100 mcg/ml, respectively. In the blood, the drug is 25-40% bound to proteins. The bactericidal concentration in the blood remains for more than 12 hours. The drug penetrates well into tissues (creates an effective concentration in the myocardium, bone tissue, gall bladder, skin, soft tissues), body fluids (determined in effective concentrations in the spinal, pericardial, pleural, peritoneal, synovial fluids), passes through the placenta, penetrates into breast milk. Cefotaxime is excreted in significant quantities in the urine (90%) (in unchanged form about 60-70% and in the form of active metabolites about 20-30%, of which 15-20% are the main metabolite - desacetylcefotaxime, which has antimicrobial activity). The half-life of intravenous administration is 1 hour, and intramuscular administration is 1-1.5 hours. With repeated intravenous administrations at a dose of 1 g every 6 hours for 14 days, no accumulation is observed. In newborns, the half-life is 0.75-1.5 hours, in premature infants - up to 6.4 hours, in patients over 80 years old - 2.5 hours, in case of renal failure, the half-life does not exceed 2.5 hours. The drug is partially excreted in bile and breast milk.
Effect of injections of the antibiotic Cefotaxime
The drug belongs to the group of third generation antibacterial agents. The active ingredient is cefotaxime in the form of sodium salt. Available in powder form for making a solution. The finished injection is administered intramuscularly or intravenously. The medicine has a slight yellowish tint. Sold in glass bottles, each containing one gram of the active ingredient.
Cefotaxime is used for sinusitis in children over two years of age and adults. It exhibits a bactericidal effect. Due to this, the active substance blocks the synthesis of the bacterial cell wall.
The drug shows high effectiveness when infected with Escherichia coli, Citrobacter, Proteus, and Klebsiella. Resistant to many beta-lactamases, which have the ability to weaken the effect of antibacterial agents.
One of the main questions that interests patients: “How many days should I inject Cefotaxime for sinusitis?” Only a doctor can determine the dosage and frequency of administration after a thorough examination. The average therapeutic course is from 5 to 10 days. In severe cases, treatment may be extended.
Injections for sinusitis usually occur in a hospital setting when the patient is hospitalized. This process is explained by the fact that the drug is one of the most powerful antibiotics. After administration of the medicine, the active component enters the sputum, which makes it possible to quickly overcome the infection.
Indications for use[ | ]
Cefotaxime is prescribed for infections caused by microorganisms sensitive to it: infections of the lower respiratory tract (bronchitis, pneumonia, pleurisy, abscesses) and urinary tract; kidney; infections of the ear, nose, throat (sore throat, otitis, with the exception of enterococcal); with septicemia; endocarditis; infections of bones and soft tissues, abdominal cavity; for gynecological infectious diseases (uncomplicated gonorrhea, chlamydia); bacterial meningitis (except listeria); Lyme disease, as well as for the prevention of post-operative infections and complications.
Directions for use[ | ]
Cefotaxime is prescribed intramuscularly and intravenously, by stream and drip. For intramuscular injections, dissolve 0.5 g (1 g) of Cefotaxime in a lidocaine solution and inject deep into the gluteal muscle.
For intravenous administration, first dissolve 0.5 g (1 g) of Cefotaxime in 2 ml (4 ml) of sterile water for injection, adjust the solvent to 10 ml and administer slowly over 3-5 minutes. For drip administration into a vein (over 50-60 minutes), dissolve 2 g of the drug in 100 ml of isotonic sodium chloride solution or 5% glucose solution. A single dose of Cefotaxime for adults is 1 g, every 12 hours; in severe cases, the dose is increased to 2.0 g, every 12 hours, or the number of injections is increased to 3-4 times a day, bringing the total daily dose to a maximum of 4 g In case of renal failure, the dose is reduced by 2 times. For acute gonorrhea, the drug is administered once, intramuscularly, in a dose of 0.5-1 g. To prevent infectious complications, 0.5-1 g is administered before or during induction of anesthesia; if necessary, the injection is repeated after 6-12 hours.
Contraindications
Hypersensitivity to cephalosporin antibiotics and other β-lactam antibiotics.
Contraindications for the use of solutions containing lidocaine:
- hypersensitivity to lidocaine or other amide-type local anesthetic;
- atrioventricular block without an established pacemaker;
- severe heart failure;
- intravenous administration;
- children under 1 year of age (intramuscular administration).
Interaction with other drugs and other types of interactions.
Uricosuric drugs
Probenecid blocks the tubular secretion of cefotaxime.
This approximately doubles cefotaxime exposure and reduces renal clearance by approximately 50% at therapeutic doses. Due to the wide therapeutic range of cefotaxime, no dosage adjustment is necessary in patients with normal renal function. Patients with impaired renal function may require dose adjustment.
Aminoglycoside antibiotics and diuretics
Like other cephalosporins, cefotaxime may enhance the nephrotoxic effects of nephrotoxic drugs such as aminoglycosides and strong diuretics (such as furosemide). In these patients, renal function should be monitored.
Cefotaxime should not be combined with bacteriostatic antibiotics (eg tetracycline, erythromycin and chloramphenicol) as an antagonistic effect may occur.
The following solutions can be used for infusions: water for injection, 0.9% sodium chloride solution, 5% dextrose, Ringer's solution.
Side effects[ | ]
After the administration of Cefotaxime, allergic reactions may appear (rashes, hyperemia, exudative erythema multiforme, fever, eosinophilia, anaphylactic reactions, in rare cases - anaphylactic shock), nausea, vomiting, diarrhea, abdominal pain, dysbacteriosis, superinfection, rarely - pseudomembranous colitis. Indicators, including biochemical ones, of peripheral blood change (neutropenia, transient leukopenia, thrombocytopenia, hemolytic anemia, arrhythmia (with rapid jet injection), headache, reversible encephalopathy, pain at the injection site, tissue inflammation, phlebitis.
special instructions
In the first weeks of treatment, pseudomembranous colitis may occur, manifested by severe, prolonged diarrhea. In this case, stop taking the drug and prescribe adequate therapy, including vancomycin or metronidazole. Patients with a history of allergic reactions to penicillins may have increased sensitivity to cephalosporin antibiotics. When treating with the drug for more than 10 days, monitoring of the peripheral blood picture is necessary. During treatment with cefotaxime, it is possible to obtain a false-positive Coombs test and a false-positive urine test for glucose. During treatment, you should not drink alcohol, since effects similar to those of disulfiram are possible (facial hyperemia, spasms in the abdomen and stomach, nausea, vomiting, headache, decreased blood pressure, tachycardia, shortness of breath).
Additionally[ | ]
Cefotaxime should be prescribed with caution to patients with allergies, including to medications. When treating during lactation, it is necessary to stop feeding. Concomitant use of Cefotaxime with nephrotoxic drugs requires monitoring of renal function; When using the drug for more than 10 days, monitoring of peripheral blood is necessary. Elderly and debilitated patients should be prescribed vitamin K preparations (prevention of hypocoagulation). If a symptom of pseudomembranous colitis is established, Cefotaxime should be discontinued. For children under 2.5 years of age, the drug is administered intravenously. The dose of Cefotaxime for infants and young children is 50-100 mg/kg body weight per day, divided into separate doses, at intervals of 12 to 6 hours. For premature infants, the daily dose should not exceed 50 mg/kg body weight.