Gastroenterologists note the widespread prevalence of the disease; according to statistics, GERD confidently occupies a leading position among all diseases of the digestive system. In Russia alone, according to various sources, gastroesophageal reflux disease affects from 13 to 46% of the population of various regions. About 40% of people around the world experience heartburn, with an average of 10% experiencing this symptom every day. Only a quarter of patients with GERD consult a doctor; the rest prefer to take medications occasionally and use traditional methods to temporarily relieve symptoms.
What happens when GERD develops?
Inflammation and disruption of the integrity of the inner lining of the esophagus with the subsequent formation of various complications occurs under the influence of hydrochloric acid, which is part of the gastric juice (sometimes - pancreatic enzymes and bile acids released into the lumen of the duodenum during digestive processes and thrown from there into the esophagus). In order for these aggressive acids and enzymes to enter the esophagus and have a damaging effect on its internal lining, the following pathological factors must be present:
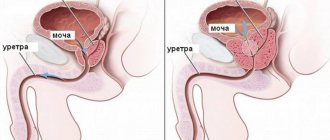
- insufficiency of the lower esophageal sphincter (a muscle that normally provides only one-way movement of the food bolus, preventing the return of food into the esophagus);
- increased intra-abdominal pressure;
- impaired cleansing of the esophagus from acids and enzymes due to decreased saliva synthesis and weakened esophageal peristalsis;
- hyperproduction of hydrochloric acid;
- decreased secretion of mucin (viscous mucus that protects the inner lining of the esophagus from the aggressive environment of gastric contents);
- slowing down the passage of gastric contents into the intestines.
As a result of increased production of hydrochloric acid and disruption of the natural defense mechanisms of the mucous membrane, permanent damage to the epithelium of the lower esophagus occurs.
Factors influencing the development of the disease
Causes that trigger the occurrence of GERD:
- smoking;
- consumption of alcoholic beverages in significant volumes and/or high strength;
- hiatal hernia;
- frequent intake of fatty, sweet, spicy, fried foods, large amounts of strong coffee, chocolate, fruit juices (packed ones, not freshly squeezed ones, are especially dangerous);
- frequent stressful situations;
- habitual overeating;
- pregnancy, especially in the third trimester;
- obesity, mainly abdominal;
- the use of certain medications (nitrates, calcium channel blockers and others);
- frequent inclined position of the body and wearing tight belts.
Stages of the pathological process
There is a Savary-Miller classification that distinguishes four stages:
- first: hyperemia and individual erosions running up the esophagus from the cardial part of the stomach or the esophageal opening of the diaphragm;
- second: merging erosions are detected that do not completely cover the surface of the inner lining of the esophagus;
- third: hyperemia and erosion during fusion completely cover the surface of the esophageal mucosa;
- fourth: complications are detected - esophageal strictures, ulcerative defects, Barrett's syndrome.
The Los Angeles classification does not consider the presence of complications, but is also actively used by gastroenterologists to formulate a diagnosis:
- stage A is characterized by the presence of one (or more) areas of inflammation of the mucous membrane measuring up to 5 mm, while the epithelium between the folds of the esophagus is intact;
- stage B is established if there is one (or more) area of inflammation of the mucous membrane with a length of more than 5 mm, while the epithelium between the folds of the esophagus is intact;
- stage C is characterized by the presence of one (or more) areas of inflamed mucous membrane, while the epithelium between the folds is also affected; approximately three quarters of the circumference of the esophagus is involved in the pathological process;
- Stage D is damage to the inner lining of the esophagus extending to more than three-quarters of the circumference of the esophagus.
Classification of the disease
According to the modern classification, gastroesophageal reflux disease is divided into three types.
- Non-erosive form. It occurs most often and is the mildest. Does not suggest the presence of erosive lesions on the walls of the esophageal mucosa. Like other forms of GERD, it is a chronic disease, but it is more treatable (but worse diagnosed). The chances of getting long-term remission are quite high. Non-erosive GERD predominantly affects men over 40 years of age. In fact, we are talking about stage 1 of the pathology, the lack of treatment of which inevitably leads to a worsening of the situation and more serious damage to the walls of the tubular organ.
- Gastroesophageal reflux with esophagitis is the 2nd form of the disease, involving pathological formations on the esophageal mucosa of the erosive type. Sometimes at this stage the situation is aggravated by the presence of ulcers.
- Barrett's esophagus is the third stage of the disease. It is considered a precancerous form. It is characterized by metaplasia of the squamous epithelium of the esophagus, resulting from esophagitis. Patients who ignore treatment for GERD at stage 1, and especially at stage 2, have a high chance of developing this serious complication.
In terms of the severity of damage to the esophageal mucosa as a result of reflux, a classification has been made according to the degrees of the disease:
- zero degree – no erosions (GERD without esophagitis);
- 1st degree – there are few erosions, they are in different places and do not merge with each other;
- 2nd degree - erosions merge in some places, but the area covered by them is still not significant;
- 3rd degree - the esophagus is seriously affected by erosions, they occupy the mucous membrane of the entire distal section;
- Grade 4 – Barrett's esophagus.
Clinical manifestations of GERD
The most common symptoms experienced by patients with GERD are:
- esophageal: heartburn, belching of air and sour, difficulty swallowing and pain when a bolus of food passes through the esophagus, pain behind the sternum of a burning nature without spreading to other areas and parts of the body;
- extraesophageal: hoarseness, sore throat, chronic cough, signs of chronic laryngitis, destruction of tooth enamel, stomatitis, unpleasant odor from the mouth, excessive formation of saliva at night.
Sometimes gastroesophageal reflux disease is asymptomatic. It is important to understand that the intensity of clinical manifestations does not always depend on the stage of development of GERD and vice versa.
Symptoms
The clinical picture of gastroesophageal reflux disease depends on the provoking factors and the degree of damage to the digestive system. The gastroenterologist, guided by the patient’s complaints, will prescribe the person the most informative examination in order to establish the correct diagnosis.
GERD (symptoms and treatment are determined by the doctor after a thorough examination of the patient) is accompanied by the following symptoms:
| Name | Symptoms |
| Esophageal signs |
|
| Extraesophageal manifestations |
|
In most cases, GERD symptoms worsen after eating, when the patient does not follow a specially formulated diet. Many people also complain of headaches, general weakness in the body, and sleep disturbances. Patients become weather dependent.
Complications characteristic of the course of the disease
Common complications of GERD are:
- Barrett's syndrome (replacement of the normal epithelium characteristic of the esophagus with an atypical one found in the stomach and intestines; is a kind of adaptive reaction of the body to frequent exposure to hydrochloric and bile acids, since the new cellular composition is more resistant to their influence, however, against the background of the course of this syndrome it is possible the occurrence of a dangerous oncological disease - adenocarcinoma of the esophagus);
- peptic ulcers of the esophagus (ulcerative defects occur due to damage caused by hydrochloric acid);
- bleeding from ulcerative defects (characterized by a long asymptomatic course, the main manifestation of which is posthemorrhagic anemia);
- esophageal strictures (narrowing of the lumen of the esophagus are formed due to the growth of connective (scar) tissue at the site of healed ulcers).
Complications
The most common (in 30-45% of cases) complication of GERD is the development of reflux esophagitis - inflammation of the mucous membrane of the lower esophagus, resulting from regular irritation of the walls by gastric contents. In the event of ulcerative-erosive damage to the mucosa and their subsequent healing, the remaining scars can lead to strictures - narrowing of the lumen of the esophagus. A decrease in the patency of the esophagus is manifested by developing dysphagia, combined with heartburn and belching.
Prolonged inflammation of the esophageal wall can lead to the formation of an ulcer, a defect that damages the wall down to the submucosal layers. An esophageal ulcer often causes bleeding. Long-term gastroesophageal reflux and chronic esophagitis lead to the replacement of the normal epithelium for the lower parts of the esophagus with gastric or intestinal epithelium. This degeneration is called Barrett's disease. This is a precancerous condition that develops into esophageal adenocarcinoma, a malignant epithelial tumor, in 2-5% of patients.
Diagnosis of GERD
The main methods to help the doctor establish a diagnosis are:
- Fibrogastroduodenoscopy. Signs of esophagitis, Barrett's syndrome, erosion and ulcers, strictures and other pathological changes characteristic of GERD are identified.
In approximately half of the patients suffering from heartburn, fibrogastroduodenoscopy does not reveal pathological changes in the inner lining of the esophagus.
- Histological examination. The method makes it possible to detect in a biopsy specimen both inflammatory changes (characteristic of GERD) and precancerous transformation of cells of the esophageal mucosa and malignant neoplasms.
- Manometry. Used to determine dysfunction of the lower esophageal sphincter and to identify disorders of esophageal motility.
- pH-metry. Used to assess the number and duration of reflux.
- pH-impedancemetry. A more modern method of detecting reflux is used to diagnose GERD that is insensitive to therapy, with an atypical course of the disease, to assess the effectiveness of antisecretory therapy without discontinuing the drug.
- Survey radiography of the chest and abdominal cavities. Detects esophageal strictures and signs of hiatal hernia.
- Endoscopic ultrasound examination of the esophagus. Used to detect esophageal tumors in controversial cases.
If necessary, the doctor prescribes further examination, for example, determining the level of pepsin in saliva, ultrasound examination of the abdominal organs, general blood test, biochemical blood test, electrocardiography and others.
Diagnostics
GERD (symptoms and treatment are recommended to be discussed with a gastroenterologist) requires a comprehensive diagnosis to establish the cause of the inflammatory process and the area of damage to the digestive organs.
Patients are prescribed the following examination methods:
| Name | Description |
| pH-metry of the stomach and esophagus | The results will help determine the duration and severity of gastroesophageal reflux. |
| pH-impedancemetry | Diagnostics allows you to identify acidic, slightly acidic or slightly alkaline refluxes, as well as differentiate their structure. |
| Endoscopy | The doctor examines the digestive organs, determines the degree and stage of the inflammatory process. |
| Radiography | A diagnostic method that is prescribed to patients to exclude the development of a hernia. |
| Ultrasound examination (ultrasound) | The specialist examines the internal organs, assesses their condition, functioning and identifies pathological processes. |
| Esophagogastro-duodenoscopy | During the examination, the doctor performs a biopsy. The taken material is examined in the laboratory. The results will help identify malignant processes. |
| Esophageal manometry | During the examination, the contractility of the esophagus and pressure in the area of the lower sphincter are assessed. |
To avoid damage or injury, many patients are prescribed proton pump inhibitors by gastroenterologists. The patient takes the medicine for a week and comes back for diagnostics. If the pathological symptoms have disappeared, the doctor assumes that the person has GERD. This diagnostic method helps if other tests have not revealed inflammation and damage to the gastric mucosa.
Questionnaire to determine the likelihood of a patient having GERD
By answering the questions of a specially designed questionnaire, the patient will be able to understand whether he has signs of GERD:
- How many days in the last week did you experience heartburn?
- How often did you burp?
- How often do you experience chest pain of a burning nature?
- How often have belching and heartburn kept you from sleeping at night?
- How many days in the last week did you have nausea?
- How often do you have to take additional medications (Maalox, Gastal, Rennie, Almagel and others, except those prescribed by your doctor) to relieve heartburn and belching?
After completing the survey, the patient can independently calculate the result:
- 0 days - 0 points;
- 1 day - 1 point;
- 2 - 3 days - 2 points;
- 4 - 7 days - 3 points.
Interpretation of the obtained score:
- 0 - 2 points - the likelihood of having GERD is low, the risk of developing erosions is 0%;
- 3 - 7 points - the likelihood of having GERD is low, the risk of developing erosions is 21.5%;
- 8 - 10 points - moderate or severe GERD, risk of developing erosions - 48.5%;
- 11 - 18 points - moderate or severe GERD, risk of developing erosions - 60.7%.
If the score is 8 or more, it is recommended to visit a doctor - a gastroenterologist or therapist!
Drug therapy
The basis of treatment for uncomplicated GERD is a course (and more often permanent) use of medications. The doctor selects treatment for the patient, which should:
- have a positive effect in relieving clinical manifestations;
- stop the damaging effect of hydrochloric and bile acids, as well as digestive enzymes on the gastric mucosa;
- prevent the progression of the disease and the formation of complications;
- promote rapid healing and restoration of the epithelial lining of the esophagus.
If there are symptoms of reflux esophagitis, if there are no signs of damage to the esophagus during FGDS, standard therapy aimed at treating GERD is prescribed.
The main drugs used as part of complex treatment or monotherapy:
- Alginates (Gaviscon). The drug dissolves quickly, forming a gel substance on the surface of the gastric contents. This substance serves as a kind of barrier to aggressive acids and enzymes, preventing them from having a negative effect on the mucous membrane of the esophagus.
- Antacids (Almagel, Relzer, Gastal, Gastratsid, Maalox, Rennie). Once in the stomach, these drugs actively neutralize hydrochloric acid and make the contents of the stomach safe for the esophagus.
A very effective remedy is flax seed, which can be purchased at any pharmacy. Use for GERD provides relief of inflammatory and pain syndromes, enveloping the esophagus and stomach due to the mucus contained in excess in each seed. Despite the availability of many modern treatment methods, many gastroenterologists advise supplementing the main therapy with a course of flax seed decoction to quickly and gently relieve the symptoms of GERD.
- Adsorbents, such as Smecta, Polysorb, Enterosgel, bind acids and enzymes in the lumen of the digestive tract.
- Proton pump inhibitors (Nolpaza, Losek, Parient, Nexium, Lancid) are the main medications prescribed to patients with GERD. Their safety and effectiveness make it possible to actively fight the disease by reducing the production of hydrochloric acid in the stomach. After completing the main course of treatment, it is almost always recommended to maintain long-term maintenance therapy to prevent relapse.
- H2 blockers - histamine receptors (Famotidine, Ranitidine). They reduce the formation of hydrochloric acid, but in the treatment of GERD they are significantly inferior to proton pump inhibitors in terms of effectiveness and frequency of use.
- Prokinetics (Cerucal, Motilium). They accelerate the slow evacuation of gastric contents and its further movement along the digestive tract, reduce the feeling of heaviness in the stomach and relieve nausea.
- Ursodeoxycholic acid preparations (Ursofalk, Ursosan) are recommended for use in case of regular reflux of bile acids from the duodenum into the esophagus.
A drug such as Omez D is a combination drug that includes a proton pump inhibitor (omeprazole) and a prokinetic agent (domperidone, which many patients are familiar with under the name “Motilium”). Omez D improves gastric motility and accelerates the passage of food, reduces the formation of hydrochloric acid, relieves nausea, heartburn and belching, which indicates its effectiveness in the fight against GERD.
Treatment of gastroesophageal reflux disease with alginates
Gastroesophageal reflux disease (GERD) is one of the most common diseases of the digestive tract, which is reflected in the postulate “The twentieth century is the century of peptic ulcer disease, and the twenty-first century is the century of GERD,” put forward at the VI Joint Gastroenterological Week (Birmingham, 1997). According to epidemiological studies, the prevalence of GERD in the adult population of Western Europe and North America reaches 10–20% [1], in Moscow - 23.6% [2].
GERD is considered a condition that develops when reflux of stomach contents causes symptoms that bother the patient and/or the development of complications. The most characteristic symptoms of the disease are heartburn and regurgitation, and the most common complication is reflux esophagitis. Regurgitation (sour belching, regurgitation) is the entry of stomach contents due to reflux into the oral cavity or lower part of the pharynx [3]. Heartburn is a burning sensation behind the sternum and/or “in the pit of the stomach”, spreading from bottom to top, individually occurring in a sitting, standing, lying position or when bending the body forward, sometimes accompanied by a feeling of acid and/or bitterness in the throat and mouth, often associated with a feeling of fullness in the epigastrium that occurs on an empty stomach or after consuming any type of solid or liquid food, alcoholic or non-alcoholic beverages, or the act of smoking [4].
The leading pathogenetic mechanism of the disease is pathological gastroesophageal reflux (GER) [5]. Because intra-abdominal pressure exceeds intrathoracic pressure, a pressure gradient acts to promote reflux of stomach contents into the esophagus, which is opposed by the lower esophageal sphincter (LES). The failure of the latter leads to the development of pathological GER, the result of which on the mucous membrane of the esophagus is determined by its composition (hydrochloric acid, pepsin, bile acids, etc.), the duration of exposure and the intrinsic resistance of the mucous membrane. In addition to the ineffectiveness of the LES, the occurrence of GER is facilitated by an increase in intra-abdominal (for example, with obesity, pregnancy, constipation) or intragastric pressure (with gastric or duodenal stasis of a functional or organic nature).
The mechanisms of the formation of the sensation of heartburn remain not fully understood. Most often, heartburn is a consequence of pathological GER (both acid and duodenal contents). In addition, the feeling of heartburn may be associated with impaired motility of the esophagus, increased sensitivity of its mucosa due to disorders of central and peripheral innervation, and changes in psychological status [6]. Taking into account and correct assessment of these mechanisms largely determines the success of therapy. Its main goals are relief of symptoms, improvement of well-being (quality of life), as well as treatment and prevention of complications, primarily reflux esophagitis. Based on the pathogenesis of the disease, this can be achieved by reducing the volume and modifying the composition of the refluxant, increasing the antireflux function of the LES, reducing the pressure gradient directed from the stomach to the esophagus, increasing the clearance of the esophagus, and protecting the esophageal mucosa from the damaging effects of the refluxant. In the presence of motor disorders, hypersensitivity of the esophagus and changes in psycho-emotional status, their correction is required.
The main directions of treatment for GERD include recommendations for changes in lifestyle and diet, pharmacotherapy (antisecretory drugs, prokinetics, alginates, antacids), if ineffective they resort to surgical treatment (laparoscopic fundoplication, etc.). Two pharmacotherapy strategies are considered as alternatives. The first of them, “gradually increasing,” involves lifestyle changes and the use of alginates or antacids at the initial stage of treatment. If they were ineffective, a transition was made to the second (histamine H2 receptor blockers and/or prokinetics) or immediately to the third stage (proton pump inhibitors (PPIs)). In the second strategy, “gradually tapering,” PPIs are prescribed, and only after achieving a clinical and endoscopic effect, patients are gradually transferred to maintenance doses of PPIs or on-demand therapy, including alginates or antacids [7].
The “gradually decreasing” strategy is recommended primarily for patients with reflux esophagitis, since it significantly reduces the healing time of erosions of the esophageal mucosa. To relieve the symptoms of uncomplicated (endoscopically negative) GERD, “gradually increasing” therapy is relevant, and already at the first step, the prescription of alginates [8]. Previous studies have demonstrated the safety and effectiveness of alginates in suppressing the symptoms of GERD and alleviating reflux esophagitis [9].
The source of alginic acid (from the Latin alga - sea grass, algae) is brown algae, mainly Laminaria hyperborea. Alginic acids are polysaccharides whose molecules are built from residues of D-mannuronic and L-guluronic acids. Blocks of mannuronic acid give alginate solutions viscosity. When guluronic acid blocks associate with the participation of calcium cations, gelation occurs.
Gaviscon is an oral suspension containing active substances: sodium alginate, sodium bicarbonate, calcium carbonate. When taken orally, Gaviscon reacts with acid in the gastric lumen, resulting in the formation of a non-absorbable alginate gel barrier. Due to carbon dioxide formed during the interaction of sodium bicarbonate with hydrochloric acid, the “alginate raft” floats on the surface of the stomach contents and mechanically prevents the occurrence of GER. If reflux nevertheless occurs, the alginate gel is the first to penetrate the esophagus and has a protective effect.
The purpose of our work was to evaluate the clinical effectiveness of Gaviscon suspension in patients with GERD.
Research objectives:
1. Assess the effectiveness of a 10-day intake of Gaviscon suspension in relieving the symptoms of GERD (heartburn, regurgitation, etc.).
2. Determine the dynamics of intraesophageal pH monitoring after taking Gaviscon suspension.
Material and research methods
We examined 30 patients (average age 46.2 ± 15.0 years, 50% women) with a non-erosive form of GERD who were hospitalized at the Central Research Institute of Gastroenterology. 46.7% of patients had a normal body mass index, and 53.3% had an excessive one. The duration of GERD symptoms ranged from 1 year to 30 years, on average 6.0 ± 8.7 years.
For 10 days, patients received Gaviscon suspension 20 ml 4 times a day 30–40 minutes after three main meals and before bedtime. GERD symptoms were rated daily using a 5-point Likert rating scale, where 1 is no symptoms at all and 5 is severe symptoms that significantly affect the patient's quality of life. Before prescribing the drug, esophagogastroduodenoscopy (EGD) and daily pH monitoring (Gastroscan-24) were performed. In 10 patients, an acute pharmacological test was performed under the control of pH monitoring with 1-fold or 4-fold doses of Gaviscon 20 ml. Before and after completion of Gaviscon treatment, well-being was assessed using a visual analogue scale (VAS). Taking into account the possible role of psycho-emotional disorders in the formation of complaints from patients with GERD, especially its endoscopically negative form, the psychological status was assessed using the SMOL questionnaire and the type of attitude towards the disease was determined using the LOBI questionnaire. The safety of the therapy was assessed based on the presence/absence of side effects.
Research results and discussion
The most common complaints were heartburn, sour belching, and air belching; dysphagia and odynophagia were less common (Table 1). A decrease in symptoms on the first day of therapy occurred in 26 (86.7%) patients. Two patients did not note the positive effect of Gaviscon and by 4-5 days they refused to continue taking the drug. One patient developed an allergic reaction in the form of urticaria on the 3rd day of treatment. Thus, 3 patients dropped out of the study, and their data were not taken into account when assessing the effectiveness of therapy. In the majority of the remaining patients, complete resolution of symptoms occurred within 1 to 7 days (
). It should be emphasized that inpatients are a more severe group of patients with GERD and the longest periods of symptom relief were in patients with excess body weight and changes in psycho-emotional status.
During therapy, an improvement in the well-being of patients was noted, which was reflected in an increase in the VAS score from 41.8 ± 15.3 before treatment to 60.2 ± 16.8 mm on the 10th day of taking Gaviscon.
An acute pharmacological test with Gaviscon carried out in 10 patients under the control of pH monitoring demonstrated its antireflux effect lasting from 1.5 to 3.5 hours. At the same time, the generalized De Meester indicator normalized or decreased significantly. The average pH in the stomach did not change in 3 patients, and in 7 patients a moderate antacid effect was observed due to the bicarbonates included in the drug.
The treatment was well tolerated in the vast majority of patients; 1 patient noted a short-term increase in burning sensation along the esophagus after taking the drug; 1 patient noted the appearance of flatulence. In 1 patient, on the 3rd day of treatment, an allergic reaction in the form of urticaria was noted. After stopping the drug, the allergy symptoms went away on their own.
Two patients stopped taking Gaviscon on days 4–5 of treatment, without noticing a clinical effect. The diagnosis in both patients was established based on the clinical manifestations of the disease: they were bothered by heartburn. At the same time, according to endoscopy, there were no changes in the esophageal mucosa; pH monitoring did not reveal pathological GER. A psychological examination (SMOL and LOBI questionnaires) revealed severe mental adaptation disorders in both patients. Probably, the mechanism for the formation of the sensation of heartburn in these patients was not pathological GER, but hypersensitivity of the esophagus against the background of changes in psychological status. An indirect confirmation of this is the ineffectiveness of Gaviscon, which relieves heartburn only in patients whose formation mechanism is pathological GER.
Conclusion
- Gaviscon suspension has an anti-reflux effect, preventing stomach contents, both acidic and mixed, from entering the esophagus by creating an “alginate raft”.
- The duration of the antireflux effect of a single dose of Gaviscon suspension ranged from 1.5 to 3.5 hours.
- The reason for the ineffectiveness of Gaviscon suspension may be non-reflux mechanisms of heartburn formation.
- Gaviscon suspension is an effective and safe drug for relieving the symptoms of GERD and can be recommended in the practice of gastroenterologists and therapists.
For questions regarding literature, please contact the editor.
Surgery
Surgical treatment is resorted to when conservative therapy is ineffective (which happens in approximately 5-10% of all cases). Most often, to achieve this goal, fundaplication is used - an operation to prevent the backflow of food into the esophagus (they suture a section of the stomach to the esophagus and “envelop” the final section of the esophageal tube with it), as well as endoscopic correction of the lower esophageal sphincter.
In the presence of complications, in most cases, various methods of surgical treatment are also used (ablation, resection, and so on).
Tips for changing your lifestyle
In addition to the listed treatment methods, modification of the patient’s lifestyle is of great importance, which includes the implementation of the following recommendations:
- eat food at least three hours before bedtime;
- sleep on a high pillow, mainly on the left side;
- do not lie down after eating;
- stop smoking;
- normalize body weight and maintain it;
- do not wear tight belts and belts;
- Take medications only as prescribed by your doctor; if any side effects occur, immediately inform your doctor.
Prevention
Simple recommendations from a doctor will help prevent gastroesophageal reflux or exacerbation of pathological processes:
- A person needs to eat right and give preference to healthy foods.
- Monitor your weight and prevent weight gain.
- Completely eliminate any provoking factors that cause stomach contents to reflux into the esophagus (physical activity, heavy lifting).
- To refuse from bad habits.
- Take medications only as prescribed by your doctor.
You should not try to treat diseases or disorders of the digestive system on your own. A gastroenterologist must make a diagnosis, as well as prescribe medications.
Dietary recommendations
Following a diet provides a noticeable reduction in the frequency and duration of reflux, helps reduce clinical manifestations, and is also a preventive method that prevents the development of complications of GERD. Basic recommendations for the patient’s nutrition:
- do not drink carbonated drinks, sweet packaged fruit juices, alcohol, strong coffee;
- reduce (ideally eliminate) the consumption of fried, smoked, fatty, salty, spicy, canned and pickled foods;
- Predominant steaming, stewing and boiling, baking without adding excessive amounts of oil is encouraged;
- avoid hot seasonings, salty, sour sauces, ketchup and mayonnaise;
- eat small meals 5-6 times a day;
- the intake of most dairy products should be limited (milk, low-fat cream, butter, kefir are allowed);
- It is not recommended to eat raw vegetables;
- bread should be consumed dried, it is advisable to exclude rye and butter products;
- All food and drinks should be consumed warm.
Monitoring a patient with GERD
Once a diagnosis is made and treatment is prescribed, the patient is advised to adhere to a regular monitoring plan:
- after the course of treatment, fibrogastroduodenoscopy should be performed to monitor therapy;
- if, when a patient undergoes fibrogastroduodenoscopy, no signs characteristic of GERD are detected, after successful treatment, a repeat endoscopic examination is not necessary;
- with each exacerbation of the disease and progression of clinical manifestations, it is necessary to undergo an examination prescribed by the doctor for the timely detection of dangerous complications;
- If there are no signs of Barrett's syndrome, fibrogastroduodenoscopy is recommended to be performed every 2 to 3 years.