We will present treatment and photos of genital warts in women (or condylomatosis) in this publication. After all, there are many diseases in nature, the names of which people only learn when they come face to face with the disease. One of the little-known but very common diseases is candilomatosis. This disease affects the human reproductive system, and in modern society people are ashamed to talk about such things openly. Externally, the disease manifests itself in the form of genital warts in women and men. Condylomatosis is caused by the human papillomavirus; today it is found in the body of almost 75% of the entire earth's population. Most people do not even suspect that they are hidden carriers of the disease, although the consequences of not treating the virus can have a disastrous outcome.
What are genital warts
Anogenital warts grow on the epithelium and mucous membranes, present as soft growths, they can mainly be seen on the genitals and around the anal area. They look similar to cauliflower.
The causative agent is nothing other than the human papillomavirus. Anogenital warts are infectious diseases of the human urinary and reproductive system.
Photos for men:
Photos for women:
Pathology in men
It is important to note that this type of neoplasm almost never occurs in people with strong immunity. The presence of bad habits, chronic diseases and other decisive factors has a strong influence on the course of condylomatosis . Let's look at the main reasons for the activation of the virus.
The cause of genital warts is human papillomavirus (abbreviated as “HPV”)
Decreased immunity
A decrease in the quality of the immune system is not always associated with chronic diseases. The body's protective functions can be reduced by lack of sleep or increased physical activity. In order to get rid of growths, the cause of which is associated with disruptions in the immune system, it will be necessary to direct treatment to restore the immune system.
Stress
Often such formations form in men exposed to stress and other prolonged psycho-emotional stress. You should remember this.
Other factors
Lack of hygiene, addiction to alcohol and tobacco, poor diet, lack of adequate sleep can also act as reasons contributing to the appearance of condylomas.
Genital warts in men, photos of which are presented below, in most cases appear six months after infection. Medical practice has described cases where a person was a carrier of the virus, but did not have genital warts on his body. Research on this issue suggests that the development of growths is strongly influenced by various internal factors.
The formation of warts begins with the virus entering the cells of the mucous membranes. The introduction of viral DNA leads to changes in cells and keratinization of the mucosal surface. The division of viral cells leads to the formation of a small spot on the affected tissues. Subsequently, growths themselves appear in place of the spot.
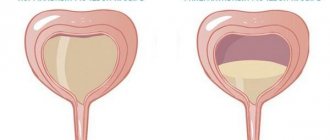
Condylomas most often form on the edges of the head of the penis, close to the urethra. The growth of tumors can lead to the creation of a kind of barrier to the outflow of urine. Detecting the development of tumors is quite simple. On the affected areas of the genital organs, keratinized areas are observed. Small lumps with a hard structure can be felt under the mucous membrane. They are the root of the tumor.
Types of genital warts
There are several main types of warts.
Namely such as:
- Typical condylomas.
- Hyperkeratotic condylomas.
- Papular.
- Flat.
Flat Hyperkeratotic
Typical
Papular
hyperkeratotic warts differ from typical warts in that they are covered with horny scales. Papular genital warts are distinguished by the fact that they are without horny layers and have a smooth surface. Flat condylomas look like spots; they do not rise above the surface of the skin.
Genital warts are detected 1-3 months after a person becomes infected with the virus.
Why do genital warts need to be treated?
Genital warts, or genital warts, are neoplasms of the skin and mucous membranes of the genital organs caused by the human papillomavirus.
Most people learn about condylomas with the onset of active sexual life. Infection most often occurs between the ages of 20 and 24, and the more sexual partners you have, the higher the risk. Moreover, condylomas do not appear immediately, but 90 or more days after sexual contact with an infected person.
Genital condylomas are not just a cosmetic defect, but also a risk factor for malignant tumors. Therefore, it is important to know what types of condylomas are, what they look like, where they are located and how to get rid of them.
Genital warts are easy to recognize by description. The first characteristic sign is the appearance of tumors several weeks or months after contact with an infected partner.
Initially, single nodules 1-2 mm in size appear. Their color varies from pink to gray-red. After some time, where there were individual defects, multiple growths appear in the form of papillae, which can merge with each other and grow like a cockscomb, raspberry or cauliflower. They are often injured, bleed, macerate (get wet), and become covered with ulcers.
The structure of genital warts is lobulated, which is easy to check with a spatula or probe. The lobules are soft, not fused to the underlying tissues, the skin around them is usually unchanged, although with constant mechanical irritation and poor hygiene, redness, itching and burning around such papillae are possible.
If a non-specialist still has doubts about the nature of such skin neoplasms, a dermatologist-venereologist can often make a preliminary diagnosis already at the first examination.
The varieties and types of condylomas vary depending on the strain of the virus. Some lesions are diagnosed visually (such as typical genital warts), while others require an acetic acid test and other studies.
There are the following types of condylomas:
- Typical condylomas, including genital warts. These are formations that are shaped like cauliflower.
- Hyperkeratotic - localized on the epithelium capable of keratinization: the labia majora, the outer layer of the foreskin, the body of the penis, the scrotum. Such formations are layered on top of each other with scales.
- Papular - have a smooth surface without horny layers.
- Flat - formations inside the epithelium, which may not have external signs, since they do not rise above the surface of the skin. Even colposcopy does not always reveal this form of condylomatosis. But if you treat the surface of the epithelium with a 3% solution of acetic acid, the areas affected by the virus will appear in the form of grayish-white spots. Such condylomas are dangerous because they are prone to germinating inwards and becoming malignant.
Symptoms of genital warts may vary depending on their type and location. In the early stages of the disease, there may be no signs.
But as the pathological process progresses, nodules appear in the affected area and associated discomfort, a feeling of a foreign body, and moisture. You may also experience pain during sexual intercourse, an unpleasant odor in the area of the rash, painful urination (if condylomas affect the urethra), and blood in the stool if the anus is affected.
There are signs of intoxication, chills, fever, weakness, headache.
Localization
- Firstly, the risk of infecting a sexual partner is very high,
- Secondly, they extremely rarely disappear on their own,
- Thirdly, without treatment, these tumors sometimes grow to significant sizes,
- Fourthly, they increase the risk of developing infection in their localization areas.
Reasons for appearance
Human papillomavirus (HPV) is the main cause of this disease. favorable conditions under which this disease manifests itself :
- pregnancy;
- the presence of secretions from the foreskin;
- various vaginal discharges;
- discharge from the urethra;
- discharge from the rectum.
The virus is transmitted through direct contact - sexual intercourse. Those at risk are those who are sexually active, mainly young people under the age of 26.
Many factors predispose to the development of the disease:
- decreased immunity;
- basic lack of hygiene;
- lack of vitamins;
- frequent stress;
- vaginal dysbiosis;
- wearing tight underwear.
Risk factors:
- early onset of sexual activity;
- unprotected sexual intercourse;
- the presence of other diseases that are sexually transmitted.
Video
Traditional methods
Self-cure of venereal warts is possible, but this happens very rarely. There are a considerable number of ways in which you can cope with condylomas. Removing growths from the skin or mucous membrane is one of the important stages on the path to recovery. Therefore, the interest of those suffering from this disease is drawn to home treatment methods. Eradicating the human papillomavirus from the body is a rather difficult task that cannot be accomplished without taking immunostimulants and antiviral agents. It follows from this that traditional methods are effective only in conjunction with the latter. You should also review your diet, eliminate alcohol, and take vitamins to boost your immunity.
Let's look at the products that are used at home to combat growths:
It is necessary to get rid of condylomas with all seriousness, otherwise even the most powerful methods may turn out to be completely ineffective.
Signs and symptoms
The incubation period lasts from several weeks to six months. According to some statistical data, it is known that the disease occurs in the same way in both men and women. The average age of people affected by this disease is 21-25 years. The genitals and perianal fold are the main location of condylomas
Among women
In women, anogenital warts are most often located on the labia majora and minora, on the posterior commissure of the lips, and very rarely on the vaginal wall and on the cervix. During oral sex, the mouth and throat are affected. During anal sex - the anal area.
Genital warts located in the vagina and cervix can only be detected during a gynecological examination. Symptoms may appear in different ways.
In men
In men, genital warts are very often located on the penis, glans, urethra, scrotum, perianal, anal and rectal area.
Localization of condylomas in the urethra causes unpleasant and painful sensations, urination becomes difficult, and the stream of urine may splash.
Symptoms of the disease
Condyloma virus in men, photos of the manifestations of which are available in this article, has a long incubation period. The average duration of the latent course of the disease is about five months. However, in medical practice there are descriptions of cases where genital warts appeared many years after infection. If pronounced symptoms of the disease appear, you should not blame your partner. Most likely, the infection occurred long before the first sexual intercourse. It is precisely because of the length of the incubation period that it is quite difficult to identify the exact moment of infection.
In women, symptoms characteristic of condylomatosis appear in various parts of the genital organs. As usual, condylomas develop in the area of the labia, vaginal walls, on the surface of the cervix and near the anus. In more complex cases, growths can form in the urethra, leading to various complications. Depending on the characteristic differences of the organism, neoplasms can be either single or located in entire groups.
In most cases, the growths fully correspond to their name and have a pointed tip. Less commonly, the apex of genital warts has a flat or rounded end. In approximately seventy percent of cases, the growths are flesh-colored. In other situations, the color of condylomas can be significantly darker or lighter than the skin tone. In addition, there are cases when genital neoplasms are so small that it is impossible to diagnose the disease yourself.
The development of condylomatosis is rarely accompanied by a feeling of discomfort. However, any injury that violates the integrity of intimate warts can lead to bleeding and irritation of the affected tissue.
Through direct contact with condylomas, virus transmission is diagnosed in 70% of cases
Treatment of genital warts in women and men
To reduce the risk of developing anogenital warts, it is necessary to use contraception, namely condoms. It is very difficult and almost impossible to completely get rid of the human papillomavirus; it can remain in the body in an inactive state for a long time. Therefore, only genital warts can be removed in order to reduce the risk of illness for the partner and alleviate the patient’s condition. To increase immunity, you need to consult an immunologist who will prescribe immunostimulants for you.
The important thing is that treatment must be carried out on both partners at the same time.
Surgery
One of the methods for removing genital warts is laser coagulation . During laser coagulation, the tissue of the condyloma acuminatum evaporates and a scab, that is, a dry crust, is formed. It is an expensive procedure. Read more about laser removal here.
Using radio waves, a radio knife also perfectly removes condylomas. The advantage of this method is that the procedure is painless. The disadvantage is that the procedure is expensive.
Cryodestruction is one of the most popular methods for removing genital warts today. The affected area is treated with liquid nitrogen using a cotton swab.
The procedure is repeated after a week and a half, and is carried out until all condylomas are removed.
This method leaves scars. This method is considered expensive and also causes pain.
Drug treatment
Condilin is 0.5% solution in a bottle. The composition contains podophyllotoxin, which, when applied topically, can lead to necrosis and destruction of genital warts.
The drug must be applied carefully so that the solution does not get on healthy areas of the body.
The drug is applied 2 times a day for 3 days , and then you need to take a four-day break. You can use this drug for no more than five weeks. Solcoderm is a mixture of nitric, acetic, lactic and oxalic acid. It also contains copper nitrate. Read more about this drug here.
The drug is applied by medical personnel; healthy areas of the body must be avoided.
Interferon
can be used . It must be injected directly into genital warts.
This procedure is quite painful, and the treatment must be repeated. Trichloroacetic acid is applied directly to genital warts. The course of treatment is one week.
If genital warts still remain, it means that this method is ineffective and you need to change to another drug.
Treatment
No doctor can guarantee that the result of the treatment will be complete recovery, since in modern medicine there is still no remedy that would eradicate condylomas. Therefore, the main method of treating venereal warts is local removal of condylomas, as well as a course of immunostimulants.
Let's consider several of these methods:
Complications of genital warts
There are many complications of genital warts. If condylomas are not treated for a very long time, they can fester.
- If the condyloma is located in places where there is contact with linen, then it may fall off, and in its place there will be ulcers that bleed.
- If genital warts are not treated promptly, their number may increase.
- Prolonged development of the virus in the human body can lead to decreased immunity.
- This infection can cause cancer of the skin and mucous membranes.
- In women, papillomavirus can lead to uterine cancer.
- In men, one of the most terrible complications is penile cancer.
How does infection occur?
Treatment of condylomas in women and men depends on the nature of the severity of the pathology. But before we talk about ways to get rid of it, let's look at the ways the virus spreads.
The papilloma virus is capable of life only in the human body. This means that the main route of transmission of the virus is contact of the carrier with a healthy person. Most often, the infection is transmitted during sexual intercourse, while the form of sexual contact itself is not critical. Even the use of condoms does not always guarantee 100% protection, since both partners are touching their bodies.
In most cases, the infection is transmitted to people with weakened immune system functions. Such complications are often observed due to lack of rest and proper sleep. Symptoms characteristic of this disease can also appear in infancy, if the virus was active in the mother’s body during the last months of pregnancy. In this situation, infection occurs at the time of birth, when the baby comes into contact with infected areas of the mucosal surface. It should be noted that this virus poses a much greater danger to infants than to adults.
Condylomatosis during pregnancy
During pregnancy, a woman's immunity decreases, so condylomas can easily recur and increase in size. During pregnancy, condylomas must be treated because they are a direct source of infection. It is recommended to begin treating genital warts during pregnancy in the third trimester.
Contraindications include treatment with cryodestruction, laser, and cytostatics. If anogenital warts have been treated, pregnancy should not be planned immediately after treatment. You can become pregnant only 2-3 months after treatment.
There is only one danger to the fetus. When a child passes through the birth canal during childbirth, he may inhale prematurely, and if there are condylomas in the vagina, the child may become infected with this virus.
As a result, the child will develop a disease such as laryngeal condylomatosis.
If condylomas during pregnancy are not located in the vagina, then there is absolutely no risk of infection.
What are the symptoms
Anogenital warts can manifest as:
- genital warts;
- warts in the form of nodules (papules);
- in the form of spots;
- neoplasia;
- Bowenoid papulosis and Bowen's disease;
- giant Buschke-Levenstein condyloma.
If the virus has become more active and condylomas have formed, it is unlikely to go unnoticed.
How do genital warts manifest themselves?
- They are easy to feel
- Itching is felt in the area where they are located,
- Makes anal hygiene difficult
- May be felt when walking and may cause injury or damage to surrounding tissues,
- They ulcerate and bleed,
- Cause psychological discomfort.
The course of the disease depends on the characteristics of the body, on how the immune system works in a particular case.
Symptoms depend on the shape of the genital wart. There are 4 main types:
- directly pointed;
- flat;
- keratinized;
- papular.
Variants of the course of the disease are as follows. Firstly, the condyloma can gradually develop (its size increases, new growths appear), and then it becomes injured. Secondly, changes may be absent for a long time. Thirdly, under the influence of immune mechanisms, the disease is stopped by the human body.
Genital warts can cause a number of complications. If they grow too much, they can be injured by clothing and then bleed.
This increases the risk of secondary infection. In addition, a person can catch other infections through microcracks.
Women may have difficulties during childbirth if condylomas have formed on the mucous membrane of the genital and urinary organs. In addition, such growths are often an obstacle to normal sexual life.
Because of this, a person’s self-esteem deteriorates and psychological discomfort appears.
Most often, growths form not one at a time, but in groups. In this case, the disease is called condylomatosis.
The growths themselves are soft and do not have a cavity inside. They are located on a wide base or on a thin stalk, which is why they rise above the level of healthy skin.
By the way, the appearance of warts depends on their location. If they form on the genitals, they have a dense shape in the form of papules, on which there are keratinized areas.
In the groin they have an uneven surface. If they have formed on the vulva, they are distinguished by either a brown or whitish tint.
When neoplasms appear on the mucous membranes, they are distinguished by a pinkish or reddish tint.
By the way, condylomas themselves most often appear in those areas where there is increased trauma during sexual intercourse. The incubation period can take from a couple of weeks to several years. Then flesh-colored or pink growths appear. They can range in size from 1 mm to 4 cm. Often the growths merge. Because of this, condylomas resemble cauliflower.
Diagnostics
Diagnosis consists of clinical examination, colonoscopy, urethroscopy, cytological studies, histological studies, and immunological studies.
Visual examination can determine the presence of genital warts.
But if genital warts are suspected, it is necessary to exclude other diseases, such as molluscum contagiosum and condylomas lata, which are found in syphilis.
Colposcopy is performed if there is a suspicion of the presence of genital warts in the vaginal part of the cervix.
If the presence of condylomas in the urethra is suspected, urethroscopy is prescribed. A smear is taken from the cervical canal and examined. The goal is to search for atypical cells in order to exclude cervical dysplasia. With the help of immunological studies, antibodies to the human papillomavirus are searched for.
Complications
Condyloma injury is especially dangerous. In such cases, the inflammatory process starts, suppuration begins, and the mucous membrane becomes covered with ulcers. You should not try to remove the condyloma yourself by tearing it off. Firstly, this can lead to infection, and secondly, at the site of the removed condyloma, a new one, and sometimes even several, always grows.
HPV can lead to erosion and cervical dysplasia. In addition, the risk of developing cancer increases.
Prevention
Prevention of human papillomavirus should be aimed at preventing infection with this virus. It is necessary to use condoms, which act as a barrier to the entry of the virus.
It is necessary to observe basic rules of hygiene of the skin and mucous membranes.
It is also necessary to increase immunity, consume more vitamins, avoid hypothermia, eliminate smoking, alcohol, and avoid stress and overwork.
Little girls are vaccinated against cervical cancer starting from the age of 11, this manipulation is carried out three times.
If you already have the virus, then this vaccine will not help. It is very important to have regular check-ups with your doctor.
Preventive actions
In order to reduce the risk of infection with the HPV virus, it is necessary to use condoms during sexual intercourse with a new partner. If one of the partners has an acute form of the disease, you should abstain from sexual activity during the course of treatment.
In the treatment of condylomas, various methods are used, including medications and hardware methods for removing growths. In order to minimize the risk of infection, it is recommended to pay increased attention to your health and hygiene.
Diagnosis of condylomas
When diagnosing a disease, all affected areas of the body are examined
When visiting a doctor, a physical examination of all areas where the presence of condylomas is suspected is performed. If warts are not visually detected, then the doctor can treat the skin with a weak acid solution, which will lighten it a little and help make them more noticeable.
If a woman has condylomas located deep inside the vagina or in the uterus, an examination of the pelvic organs may be required using a special microscope - a colcoscope.
Colposcopy can be especially useful in identifying flat lesions that are not visible to the naked eye. It is a thorough diagnosis that will help to carry out high-quality treatment and removal of condylomas.
During diagnostic procedures, the gynecologist may also take smears from the vagina and samples of cervical cells (biopsy). The data obtained is then tested in a laboratory for the presence of HPV. Some types of viruses may show abnormalities in the results and indicate precancerous conditions.
If these anomalies are detected, emergency complex treatment of genital warts may be required with further regular monitoring for possible changes. If there is concern about contracting a form of HPV that can cause cervical cancer, a DNA test may be ordered to determine the strain of the virus.
When collecting information to make a diagnosis, the doctor conducts a survey about the general health of the patient, about his sexual contacts, especially those during which unprotected sex took place, including oral sex.
Prevention of condylomas
Is it possible to prevent genital warts?
In the Russian Federation, two types of vaccines can be purchased: bivalent (HPV types 16 and 18), and trivalent (HPV types 6,11,16,18). Vaccination is recommended before the start of active sexual life. Also, HPV vaccine prevention is more relevant for females, due to the frequent association of this infection with cervical cancer.
If you find signs of genital warts, do not self-medicate and seek help from a dermatovenerologist. I strongly recommend that you consult a doctor at the first signs of the disease, due to the fact that at the initial stage of development, condylomas are much more amenable to therapy, and in the absence of therapy they progress quickly.
Nonspecific measures for the prevention of genital warts are available to adults. This is a healthy lifestyle, food rich in vitamins and microelements. Factors that suppress the immune system should be avoided - smoking, excessive amounts of alcohol, heavy psychophysical stress. It is also worth being selective in sexual intercourse and using barrier methods of contraception.
A vaccine has now been developed against some strains of HPV. Scientists have high hopes for it, since human papillomavirus infection is a risk factor for the formation of cervical cancer and other cancers.
To prevent cervical cancer, vaccination is carried out for girls aged 9 to 26 years using the drug Cervarix. The Gardasil vaccine is also effective. Mostly girls are vaccinated, since the potential risks of HPV infection are greater for them than for boys.
Prevention consists of avoiding casual sexual intercourse, using condoms, chemical solutions (Miramistin, chlorhexidine), and suppositories (Hexicon) after them.
Diagnosis and treatment
All patients with clinical manifestations of genital warts require consultation with a dermatovenerologist and treatment.
A positive HPV test is not an absolute indication for treatment.
If symptoms of genital warts are detected, it is necessary to examine sexual partners
Treatment goals:
- removal of genital warts;
- improving the patient's quality of life.
The main method of treating condylomas is the removal of formations on the skin and mucous membranes. It should be borne in mind that after removal of condylomas, relapses are possible in up to 30% of cases. The likelihood of development is much higher if the removal was performed by the patient independently, and not by a qualified specialist.
In most cases, treatment is carried out on an outpatient basis; only in rare cases of extensive damage requiring surgical treatment, hospitalization in a hospital is possible.
Cytotoxic and chemical agents for removing condylomas
- cream or raster podophyllotoxin
- zinc chloropropionate solution in 50% 2-chloropropionic acid, solution (externally only!)
- a combined preparation containing nitric, acetic, oxalic, lactic acid and copper nitrate trihydrate (solution for external use only)
Local immune preparations for condylomas
- Keravort or Aldara cream
- Administration of α-interferon to the area of condylomas.
Physical methods
- electrocoagulation
- laser removal
- radiosurgical removal (for example, with the Surgitron device)
- cryodestruction (removal of condylomas with liquid nitrogen)
All physical removal methods are carried out under local anesthesia, and therefore the patient feels comfortable during the procedure.
Surgical removal of condylomas is used in patients with multiple lesions of the skin and mucous membranes, for example, with giant Buschke-Levenstein condyloma.
How to treat genital warts during pregnancy?
During pregnancy, progression of the disease and the appearance of new condylomas are quite possible.
The optimal period of treatment for pregnant women is considered to be up to 36 weeks of pregnancy using the following methods: cryodestruction, laser destruction, electrocoagulation, with the mandatory involvement of obstetricians and gynecologists in the treatment process.
If a pregnant woman has a large number of genital warts, a cesarean section is recommended in order to avoid infection of the newborn and the development of, for example, laryngeal condylomatosis.
Treatment of genital warts in children
Treatment of condylomas in children is preferably carried out using physical methods of destruction (removal), which will not cause toxic complications
What should be the results of treatment?
No manifestations on the skin and mucous membranes.
Tactics in the absence of treatment effect
For frequent relapses, it is recommended to re-remove condylomas and prescribe antiviral drugs:
- inosine pranobex
- gamma interferon
Therapy must be comprehensive. It is aimed at strengthening the immune system and eliminating the condyloma itself.
Strengthening the immune system is required so that the body can independently fight the virus. It will not be possible to completely eliminate the virus from the human body; such drugs have not been developed.
The same applies to vaccines - they are at the development stage. Therefore, it is very important to maintain the body’s strength so that the immune system can fight the viral infection and suppress its activity.
To do this, the doctor will prescribe vitamin-mineral complexes and immunomodulators if necessary. In addition, you need to reconsider your diet - every day you need to eat more fruits, berries, herbs and vegetables.
Genital warts must be removed.
In 70% of cases, radical therapy gives a positive result, but in 30% of cases a relapse can occur. Several methods have now been developed for the removal of genital warts. The doctor chooses the most optimal one among them, depending on the location of the tumor, its nature, shape and quantity.
The appearance of warts in an intimate place indicates a viral infection of the body, which requires competent therapy.
In rare cases, the infectious disease may go away on its own.
If you have the first warts on your private parts, treatment at home can help you get rid of them quickly.
It is possible to cure genital warts in women at home only if the warts are localized on the skin of the perineum. Removing genital warts from the cervix using traditional methods is dangerous due to numerous complications.
We list the effective folk methods of getting rid of condylomas:
- Pieces of garlic are applied to the condyloma overnight under a bandage. The procedure is repeated until the growth disappears.
- You can buy celandine juice at a pharmacy or use fresh stems of the plant. It is necessary to lubricate the nodules several times a day until healing.
- The juices of sour apples, aloe, pineapple, and grapevine are also used to remove warts. You need to rub the condylomas with the juices of these plants for 10 days.
- Vinegar is mixed with wheat flour, the resulting dough is carefully applied to the condyloma. You should try not to burn healthy skin during the procedure. The dough is left until completely dry. The procedure is repeated until the nodule disappears.
- Propolis is soaked in saliva and applied to the growths under a bandage for several days (up to 3 days).
Diagnostic methods
Men can consult a urologist, and women can consult a gynecologist. PCR diagnostics allows you to determine the presence of papillomavirus in epithelial cells taken from the affected areas. The area around the anus, covered with condylomas, is examined under magnification. This method is called anoscopy. Certain areas of growths are studied using histological examination under a microscope. If necessary, the person is referred to a proctologist for consultation.
An experienced doctor is able to make a diagnosis during an external examination. But additional research methods are needed to identify the type of virus. Certain types of infectious agents can cause tumors, so a blood test using PCR is desirable. It is recommended to take it to your partner, even if he has no clinical manifestations. If the results are positive, it is necessary to carry out preventive measures to prevent the development of the disease.
Sometimes they resort to diagnostic methods with 5% acetic acid. Take a medical napkin, moisten it in the solution and apply it to the condylomas for 10 minutes. After this, the rashes become lighter. This test is effective when it is necessary to carry out differential diagnosis with other sexually transmitted diseases. Genital condylomas must be differentiated from lichen planus, folliculitis, and molluscum contagiosum.
Often, in addition to genital warts, a person is diagnosed with other sexually transmitted diseases. If the disease is mild, then with the permission of a doctor, condylomas can be treated at home.
Kinds
- Keratotic. Horn-shaped growths resembling cauliflower or seborrheic keratosis; usually located on dry skin (women's labia).
- Papular. Such condylomas have a characteristic dome-shaped shape, a diameter of 1 to 4 mm and a smooth surface (less horny than in the case of keratotic ones) of a reddish color. Location: keratinized skin.
- Giant Buschke-Levenshtein condylomas. These are large formations that develop in patients with a reduced level of cellular immunity, as well as in pregnant women.
Classification by localization
As for the localization of genital warts, condylomas are distinguished based on this feature:
- external anogenital (located in the area of the labia majora and minora);
- vaginal, which are located in the area of the vestibule of the vagina;
- endourethral (formed in the urethra);
- anal (located in the anus area);
- cervical tumors;
- oral cavity (localized on the lips, tongue, mucous membrane of the cheeks).
Dangerous consequences and prevention
Lack of timely and effective treatment can lead to serious complications. First of all, this is the appearance of more and more genital warts, which can fester and fall off due to constant contact with underwear, leaving behind painful and bleeding ulcers. The presence of numerous growths can lead to complications in the processes of urination and defecation, as well as to a narrowing of the foreskin - phimosis. But the main danger is the risk that benign formations can eventually become malignant, causing cancer.
Preventive measures are simple and effective:
- maintaining the level of the immune system;
- do not overcool the body;
- If possible, give up smoking and alcohol;
- Avoid chronic fatigue and stressful situations.
If the problem is low activity of the immune system, you can use immunostimulants, which include Cycloferon, Immunal and others. Their relevance is due to the reduction in the risk of the appearance of new formations, but in fairness it is worth noting that doctors still doubt the effectiveness of this method.
If genital warts appear regularly and treatment does not bring the desired effect, then it is worth undergoing a full course of examination to identify the cause of this phenomenon. A qualified doctor will not get rid of the virus, since it is classified as lifelong, but it will significantly alleviate the patient’s condition.
How to get rid of genital warts
It is not yet possible to completely eliminate the human papillomavirus from the body. But this does not mean that modern medicine does not have an answer to the question of how to deal with condylomas. Condylomatosis requires complex treatment, which includes immunocorrection and elimination of external manifestations of the disease - removal of condylomas.
Modern methods relieve patients of growths quickly, painlessly, with minimal risk of complications. Each of them is good in its own way and has its own indications.
Immunostimulating and antiviral drugs for oral administration
The main method of treatment is removal of condylomas. Immunostimulants and antiviral drugs are complementary to surgical methods. They do not get rid of existing growths, but prevent the appearance of new ones. Without drug therapy, tumors reappear in 30% of patients.
How to get rid of genital warts using the pharmacy arsenal? Antiviral drugs used for oral administration include Isoprinosine, Panavir, and Epigen. Immunal, Reaferon, Polyoxidonium, Likopid or other drugs are recommended as immunostimulating therapy.
You can try to remove the growths at home, but it is better to get rid of the growths under the supervision of a specialist. The most effective treatment against condylomas can only be prescribed by a doctor.
Local medications
The most inexpensive way to remove condylomas is chemical destruction. The neoplasm is treated with a preparation that contains a concentrated alkali or acid, for example, Lapis pencil, Supercelandine. Products of this kind require extremely careful handling, as they can damage healthy tissue.
In some cases, removal of condylomas is performed with local medications. First of all, these are drugs that cause necrosis of neoplasm tissue - Podophyllotoxin, Condyline, Condiline.
They are not acidic compounds, but act on the principle of cauterization, resulting in burning, hyperemia (redness of the skin), and discomfort during the procedure and after. Such drugs are contraindicated during pregnancy.
Before removing condylomas with these means, you should consult a specialist.
Another category of agents are local antiviral agents, in the form of injections or creams. In the first case, it is recommended to inject the growth site with a human interferon preparation.
The drug has a number of side effects, including fever, like a cold. Removing condyloma at home is possible using external agents such as Imiquimod.
The cream is applied to the lesions overnight and washed off in the morning with warm water and soap. The drug is effective only for small growths.
Hardware and surgical methods
Removal of condylomas can be carried out using hardware or surgical methods. Some of them are painless, others require anesthesia. Today, patients do not have to worry about whether it is painful to remove condylomas. If you experience discomfort, your doctor will administer anesthesia before removing the condylomas.
- The simplest and rarely practiced way to remove growths on the genitals is surgical excision. Removal of condyloma is carried out with a scalpel under local anesthesia, followed by a long recovery period, during which it is necessary to regularly treat the wound.
- As an inexpensive alternative method, you may be offered cryodestruction. During the procedure, the changed skin is frozen with liquid nitrogen, which causes the destruction of proteins and the death of the pathological formation. The papilloma disappears, and the wound heals within a few weeks. The method is relatively painless and does not require anesthesia.
- Electrocoagulation is the cauterization of tissue under the influence of high frequency current. This way you can cut off the growth and cauterize the wound. After the procedure, enhanced tissue regeneration is observed. Among the disadvantages, it should be noted that the method requires anesthesia and can leave scars.
- Radio wave therapy is an expensive but extremely effective method of removing tumors. The device for this procedure is called radioknife or Surgitron. It generates radio wave radiation that burns out the tumor. The instrument does not come into contact with the skin, which eliminates infection, reduces the risk of suppuration, and simplifies wound care. The operation is performed under local anesthesia and is practically painless.
- Laser therapy is the most effective way to eliminate genital tumors. Under the influence of a laser beam, the condyloma tissue evaporates. However, the method is rarely used for anogenital pointed growths due to the risk of burning the mucous membranes.
Treatment of condylomas with folk remedies
Traditional medicine, like official medicine, offers two approaches to the treatment of genital warts - general strengthening of the immune system and removal of genital warts using local treatment.
Genital warts (or condylomas) are benign growths that form on the genitals of men and women aged 18 to 35 years.
Neoplasms are not always harmless:
- often cause discomfort, itching, pain, especially during and after sexual intercourse;
- can be injured, and in some cases, degenerate into a malignant form.
That is why the treatment of genital warts is based on their removal.
Like other warts, growths on the genitals appear as a result of infection with the human papillomavirus.
In total, over 100 different types of HPV have been studied, which, based on their ability to cause malignant processes, are divided into groups:
- non-oncogenic;
- low risk;
- high risk.
The appearance of genital warts is caused by low-risk HPV (types 6, 11, 13) and high oncogenic risk (types 16 and 18).