Any woman has seen yellow vaginal discharge. However, not everyone knows that in certain situations they are the norm. In most cases, representatives of the fairer sex begin to worry and look for ways out of the situation.
Using folk remedies for treatment, douching without a doctor’s prescription and taking medications, they only worsen their condition. Before treating yellow discharge, you should make sure that the cause of its origin is truly pathological.
When is yellow discharge not a deviation?
In the case when the discharge becomes yellow in color, but does not cause discomfort, and also has no odor, then most likely it should be considered normal. The fact is that the cause of this condition may be changes in hormonal levels, severe stress, or the use of contraceptives. However, after sexual contact, during which seminal secretions entered the vagina, the discharge may also become yellow.
Before menstruation, during ovulation, and also during pregnancy, almost all women experience an increase in the amount of discharge, and due to hormonal changes, they may become yellowish at this time.
So you have vaginitis - now what?
If you experience any of the symptoms listed above other than yellow vaginal discharge, you should contact your doctor immediately. She'll take a sample of your discharge to determine the cause of your vaginitis and even perform a Pap smear to rule out cervical cancer. Unless you are suffering from a yeast infection, your doctor will likely prescribe antibiotics to help restore the normal balance of vaginal flora, fight bacteria, and return your discharge to normal. Keep in mind that light yellow vaginal mucus can also be associated with early pregnancy. If you experience this during pregnancy (especially after the 37th week), then no treatment will be needed.
When does yellow discharge cause the development of pathology?
With the development of a particular disease, in addition to a change in color, the amount of vaginal secretion, as well as its consistency, may also change. Thus, the discharge may become foamy, cheesy or jelly-like.
Copious yellow discharge
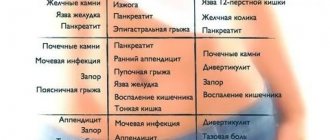
This condition often signals the development of an acute bacterial infection. It can cause the following diseases:
- Inflammatory process in the fallopian tubes (salpingitis). Develops due to hematogenous spread of pathogenic microflora from the uterine cavity or other nearby organs. In the acute form, the patient experiences copious yellow discharge, pain may appear when urinating, bloating is often noted, and after sexual intercourse, blood is found in the discharge.
- Adnexitis (inflammation of the uterine appendages). This disease occurs due to the penetration of infection through ascending or descending pathways. In the acute form, a woman develops profuse, purulent, yellow discharge, causing severe irritation of the external genitalia. Patients complain of a frequent urge to urinate, they experience pain during sexual intercourse, and menstruation is very painful.
- Bacterial vaginitis (inflammation of the vaginal mucosa). This is a disease of infectious etiology, accompanied by profuse yellowish discharge, swelling and itching of the external genitalia, as well as pain in the lower abdominal cavity and back.
- Urogenital infections (gonorrhea, trichomoniasis, chlamydia). With the development of sexually transmitted diseases, the discharge also becomes yellow in color, abundant impurities of pus appear in it, and a sharp unpleasant odor appears. The external genitals swell, severe itching and burning develop, intensifying after urination, and pain appears during sexual intercourse.
- Allergies also often cause yellow discharge. The pathological condition can be provoked by synthetic underwear, sanitary pads and tampons, as well as the use of condoms.
Scanty yellow discharge
Yellow vaginal secretion, released in a small volume, can occur with cervical erosion, chronic adnexitis and chronic salpingitis
Discharge with odor
Doctors consider an unpleasant odor as one of the signals about infection of the reproductive system. Often we are talking about STIs.
Trichomoniasis
The mucus coming out of the vagina has a yellow or green tint and a foamy consistency. Particular discomfort is caused by the smell of rotten fish and pain during sexual intercourse associated with hyperemia of the small lips.
Chlamydia
At the initial stage, the discharge is light in color; the progression of the pathology is indicated by its identity in appearance with the purulent contents and a pronounced shade. If the situation is aggravated by the spread of inflammation to the urinary tract, the burning sensation is a constant concern. It is possible to differentiate chlamydia and trichomoniasis thanks to a smear on the flora and bacterial culture.
Colpitis, oophoritis
The discharge takes on a yellow-green color due to the presence of pus in the mucus. With colpitis, the actively secreted secretion has a thick consistency, sometimes bloody inclusions can be seen with the naked eye.
The peculiarity of oophoritis is the involvement of the female reproductive glands in the inflammatory process and disruption of hormone production. The consequence of negative mechanisms is a disruption of the menstrual cycle, prolongation of menstruation with a simultaneous increase or decrease in the volume of discharged masses.
Gonorrhea
The infection can be determined by the appearance of greenish mucus or yellowish-white secretion. Difficulties with diagnosis are due to the similarity of the clinical picture with candidiasis. The main treatment regimen involves taking antibacterial drugs.
Mucus with a pronounced odor is also a symptom of vaginitis and cervicitis, which affects the vaginal cavity and cervix, respectively. In the latter case, erosion forms, on the surface of which purulent discharge collects.
Discharge after abortion
Normally, a woman may experience brownish discharge for ten days after an abortion. This is due to the fact that blood oozes lightly from the internal genital organs, which, reaching the external genitalia, manages to coagulate. At the same time, yellowish-brown discharge that occurs after an artificial termination of pregnancy can signal the presence of polyps in the uterine cavity. Such benign neoplasms do not pose any particular danger, but, nevertheless, they can cause pain in the lower abdomen, especially after sexual intercourse.
Also, the occurrence of this kind of discharge may signal the development of an inflammatory process of an infectious nature, provoked by staphylococcus, streptococcus, Proteus and E. coli. This condition occurs due to decreased immunity and activation of potentially pathogenic microorganisms.
Characteristics of normal vaginal discharge
1.Consistency.
2. Smell.
3. Volume.
https://www.youtube.com/watch?v=gkpWnHxC8aQ
4. Structure.
Brown, odorless discharge is a general concept. This way you can describe dark yellow, brown, light and dark brown, as well as black mucus.
Its main components are the secretion produced by the glands of the reproductive system and fluid from the cervical canal. Leucorrhoea acquires an uncharacteristic color when oxidized and coagulated blood gets into it. In this case, discharge of a light or dark brown hue may not smell at all, and unpleasant sensations may not appear.
Such changes are observed during pregnancy and in different phases of the cycle. Women do not perceive them as signs of illness. There is a misconception that pathology should always be accompanied by unpleasant sensations. In fact, everything is somewhat different. There may be a hidden threat in the body that is only indicated by an uncharacteristic secretion.
Yellow discharge during pregnancy
During the period of bearing a child, the discharge may have a different character. In the first three months, when progesterone has the greatest influence on the female body, thick discharge with a yellowish tint and practically no odor often occurs.
However, in the second trimester of pregnancy, discharge normally becomes more abundant and transparent, and therefore, if it begins to acquire a yellow color and is accompanied by an unpleasant odor, this may signal the possible development of a pathological process.
Bright yellow discharge during pregnancy is often a symptom of inflammation of the fallopian tubes or ovaries, which develops due to a bacterial infection. Sometimes a change in the color of vaginal secretions occurs due to the use of intimate hygiene products that are unsuitable for a woman or when wearing synthetic underwear. In this case, when the irritant is eliminated, all unpleasant symptoms go away on their own.
Natural secretion
Healthy vaginal flora contains bacteria that are beneficial to the female body. They protect the reproductive organs from harmful microorganisms. In addition to them, a small amount of fungal bacteria is also present in the reproductive system. Normal microflora is an unfavorable environment for their growth and reproduction.
The body's protective reaction is manifested in the appearance of mucus from the vagina. Most often they have a homogeneous mass of transparent color. And only under the influence of oxygen, having oxidized, a yellowish discharge appears without odor and itching. Moreover, color saturation changes during the menstrual cycle.
Natural secretions cannot cause itching or irritation of the skin of the external genital organs, and they should not have an unpleasant odor. Typically, yellow discharge in women, which has many causes, is not a cause for concern .
What to do if you are worried about yellow vaginal discharge?
If the occurrence of yellow discharge is not accompanied by any negative symptoms, then most likely there is no cause for concern. You just need to monitor your intimate hygiene as carefully as possible, wear underwear only made from natural fabrics, use only proven and high-quality cosmetics and hygiene products, as well as barrier contraceptive methods.
In the case where yellow discharge causes some concern, causes burning and itching, makes it difficult to urinate, and is also accompanied by an unpleasant odor, urgent consultation with a specialist is required, who, after a thorough physical examination and passing all the necessary tests, will be able to determine the true cause of this condition, as well as , if necessary, will prescribe treatment.
Light yellow vaginal discharge: when is it normal?
In short, light yellow discharge is normal only if there is no odor, itching, redness or tenderness of the vulva (genital area). Many women have light yellow vaginal discharge instead of whitish or clear discharge, while some experience it early in pregnancy or just before their period begins. In the latter case (before menstruation), light yellow, odorless discharge may be accompanied by itching and soreness of the vulva, which disappear after the onset of menstruation.
The sequence of your discharge depends on the timing of your menstrual cycle. After the end of the cycle, you will notice that the discharge is thick and white. By the middle of the menstrual cycle, vaginal mucus will become clear and thin with a consistency very similar to the white of a raw egg. As your period approaches, your discharge will again become white, thick, and even slightly yellow.
Cervicitis
Cervicitis is a disease characterized by inflammation of the cervix. This inflammatory process is characterized by gray cloudy discharge (possibly purulent), urination problems, pain in the lower abdomen, and painful sexual intercourse. Advanced cervicitis can lead to the development of cervical erosion. Occurs when opportunistic microflora enters the cervix: staphylococci, streptococci, E. coli, fungi, trichomonas, chlamydia, gonococci, parasitic infections. Sexual transmission is also possible.
Cervicitis often develops together with other diseases of the genital organs, such as vaginitis, entropion, vulvitis, pseudo-erosion of the cervix, etc. It is quite rare in women during menopause; this disease is mainly typical for women of reproductive age. To diagnose cervicitis it is necessary:
- conducting a gynecological examination;
- laboratory examination of smear and bacterial culture;
- performing colcoscopy.
Treatment of cystitis depends on the causative agent of the disease. They mainly use antibacterial and antiviral agents, douching with a solution of dimethyl sulfoxide, chlorophyllipt, and silver nitrate. In some cases, it is necessary to use vitamins, immunostimulants, interferons, and cytostatics.
Gardnerellosis, or bacterial vaginosis
Gray discharge in women can be a sign of bacterial vaginosis. This is a non-inflammatory disease associated with changes in the vaginal microflora. Almost every woman experiences this disease at least once in her life. For the carrier of the disease, gardnerellosis is not dangerous, but it can cause miscarriages, complications of childbirth, and fetal infections.
Bacterial vaginosis appears as a result of disruption of the vaginal microflora and colonization of it by pathogenic bacteria that enter there either sexually or from the skin of the perineum.
Opportunistic bacteria that cause gardnerellosis are mycoplasmas, atopobium, bactericides, peptococci, peptostreptococci, gardnerella, megaspheres.
Signs of bacterial vaginosis:
- gray mucous discharge;
- unpleasant fishy smell;
- the volume of discharge is small;
- discharge does not change depending on the menstrual cycle.
The appearance of pain in the lower abdomen, pain, burning indicates that some kind of infection is associated with bacterial vaginosis. Treatment is carried out with antibacterial agents, mainly penicillins or cephalosporins. Douching with chlorhexidine solution is also prescribed. After the main course of treatment, medications are prescribed to restore the vaginal microflora. Under no circumstances should this disease be treated on its own.
Gray discharge in women can be observed for a number of other reasons:
- intimate hygiene with the use of unsuitable detergents leads to disruption of the vaginal microflora, washing away beneficial bacteria and creating a favorable environment for the development of pathogenic microorganisms;
- damage to the mucous membranes of the vagina due to frequent sexual intercourse;
- helminths (roundworms or pinworms) often cause gray discharge;
- sexually transmitted diseases (venereal infections): chlamydia, trichomoniasis, gonorrhea in the initial stages of the disease manifest themselves in the form of gray discharge with a foul odor;
- various types of inflammation (vagina, appendages, cervix);
- diseases of the endocrine system, vascular diseases;
- taking contraceptives without a specialist's prescription;
- hormonal imbalance due to thyroid disease, tuberculosis, or the presence of any infection;
- atrophic vaginitis;
- various allergic reactions;
- thermal burn of the mucous membranes of the vagina.
Cervical erosion
Cervical erosion is a disorder of the mucous membranes of the cervix. Translated as "destruction".
Symptoms of cervical erosion are as follows:
- burning and itching when urinating;
- discomfort during sexual intercourse;
- gray-yellow discharge, possibly bloody.
Erosion can be divided into 2 groups: true erosion and pseudo-erosion (ectopia).
True erosion is also divided into subgroups:
- leukoplakia – hardening of the epithelium in any area of the cervical mucosa;
- ectropion – forward displacement of cervical tissue, occurring as a result of abortion or difficult childbirth;
- endometriosis – vertical displacement of the mucous surfaces of the cervix;
- polyps of the cervix and cervical canal.
Ectopia, or pseudo-erosion, is not a disease; in the absence of inflammatory processes it is not dangerous. Most often, this pathology is congenital.
To diagnose erosion, it is necessary to examine a gynecologist using speculum, smear examination, biopsy, cytological analysis, colposcopy, tests for the presence or absence of infection, and a blood test.
Treatment of erosion is carried out using surgical methods:
- cryotherapy;
- chemical coagulation;
- laser therapy;
- diathermocoagulation;
- radio wave influence.
At the moment, the best treatment for cervical erosion is radio wave surgery. It allows you to completely get rid of pathology, while the process itself is completely painless. Unfortunately, not all clinics have the equipment to perform these operations.