| Measles | |
| Measles virus under an electron microscope | |
| ICD-10 | 05. |
| ICD-9 | 055055 |
| DiseasesDB | 7890 |
| MedlinePlus | 001569 |
| eMedicine | derm/259 |
| MeSH | D008457 and D008457 |
Measles
(lat. Morbilli) is an acute infectious viral disease with a high level of susceptibility (the contagiousness index approaches 100%), which is characterized by high fever (up to 40.5 ° C), inflammation of the mucous membranes of the oral cavity and upper respiratory tract, conjunctivitis and characteristic maculopapular rash of the skin, general intoxication.
The World Health Organization estimates that 158,000 people worldwide died from measles in 2011, most of them children under the age of five. In 10% of children with malnutrition and lack of proper medical care, the disease is fatal[1]. In Russia, the incidence of measles for 2020 is 3.2 cases per 100,000 people[2].
Content
- 1 Etiology
- 2 Distribution
- 3 Pathogenesis and pathological anatomy
- 4 Clinical picture of typical measles
- 5 Complications
- 6 Atypical (weakened) measles
- 7 Measles in adults
- 8 Measles in immunocompromised patients
- 9 Measles and allergies
- 10 Laboratory data
- 11 Differential diagnosis (DD)
- 12 Treatment
- 13 Prevention 13.1 Safety
- 13.2 Dosage form
- 17.1 In English
First signs of measles
During the catarrhal period of the disease, the first symptoms of measles in adults are observed: a sharp deterioration in the patient’s well-being, weakness, photophobia, headache, and loss of appetite. The initial phase of the development of infection is characterized by a sharp and strong increase in body temperature (up to 40°C), runny nose, wheezing, vomiting, convulsions, and loss of consciousness. Measles often causes symptoms of bronchitis, tracheitis, pneumonia, swelling and pallor of the face. The period of first signs of the disease in adults lasts 5-7 days.
Etiology
The causative agent of measles is an RNA virus of the genus Morbillivirus, a family of paramyxoviruses, which has a spherical shape and a diameter of 120-230 nm. The virus consists of a nucleocapsid - a minus strand of RNA, three proteins and an outer shell formed by two types of matrix proteins (surface glycoproteins) - one of them is hemagglutinin, the other is a “dumbbell-shaped” protein.
The virus is not stable in the external environment and quickly dies outside the human body from exposure to various chemical and physical factors (irradiation, boiling, treatment with disinfectants).
There is a hypothesis about the origin of the measles virus from the rinderpest virus during the emergence of animal husbandry[3].
Despite its instability to the external environment, there are known cases of the virus spreading over significant distances with air flow through the ventilation system - during the cold season in one single building. Weakened strains of measles virus are used to produce live measles vaccine.
Spreading
The route of transmission of infection is airborne; the virus is released into the external environment in large quantities by a sick person with mucus during coughing, sneezing, etc.
The source of infection is a patient with measles in any form, who is contagious to others from the last days of the incubation period (last 2 days) until the 4th day of rash. From the 5th day of the rash, the patient is considered non-infectious.
Measles affects mainly children aged 2-5 years and much less often adults who did not have this disease in childhood. Newborn children have colostral immunity, passed on to them from their mothers if they have previously had measles. This immunity lasts for the first 3 months of life. There are cases of congenital measles due to transplacental infection of the fetus with the virus from a sick mother.
After an illness, stable immunity develops; re-infection with measles in humans, without concomitant pathology of the immune system, is doubtful, although such cases have been described. Most cases of measles are observed in the winter-spring (December-May) period, with an increase in incidence every 2-4 years.
Currently, in countries that conduct total measles vaccination, the disease occurs in the form of isolated cases or mini-epidemics (for example, in 2013 in the Netherlands[4]).
In 2020, Rospotrebnadzor reported an ongoing epidemic rise in measles incidence in Europe. Cases of the disease have been identified in 14 European countries, and the total number of victims is more than 4,000 people.[5]
On August 20, 2020, WHO reported a record level of incidence in the European region: the number of people infected in the first six months of 2020 amounted to more than 41 thousand people, with 37 deaths. It is noted that this is the highest incidence rate since 2010. More than 1,000 cases of infection have been recorded in Georgia, Greece, Italy, the Russian Federation, Serbia, Ukraine and France[6].
Prevention of infectious disease
To avoid contracting measles, you should follow some preventive measures:
- Get vaccinated. Measles vaccinations are administered almost all over the world. The activities are absolutely safe and can be performed by both adults and children. Before the procedure, it is advisable to consult with your doctor. Pregnancy, AIDS, tuberculosis and leukemia are considered contraindications. In childhood, it is necessary to vaccinate twice - at 1 and 6 years.
- Vaccination with immunoglobulin is done if there has been contact with a patient.
- During the epidemic, try to avoid places where large numbers of people gather.
Like many other infectious diseases, measles requires immediate treatment. In no case should you let the disease take its course, as this is fraught with serious consequences.
attuale.ru
Pathogenesis and pathological anatomy
The virus enters the human body through the mucous membrane of the upper respiratory tract and then through the bloodstream (primary viremia) the virus enters the reticuloendothelial system (lymph nodes) and affects all types of white blood cells. From the 3rd day of the incubation period, typical giant multinucleated Warthin-Finkeldey cells with inclusions in the cytoplasm can be found in the lymph nodes, tonsils, and spleen. After multiplying in the lymph nodes, the virus enters the blood again, and repeated (secondary) viremia develops, which is associated with the onset of clinical manifestations of the disease. The measles virus suppresses the activity of the immune system (direct damage to T-lymphocytes is possible), a decrease in immunity occurs and, as a result, the development of severe secondary bacterial complications with a predominant localization of processes in the respiratory organs. The virus may also cause temporary vitamin A hypovitaminosis.
Microscopic picture: the mucous membrane of the respiratory tract - edema, vascular congestion, foci of necrosis, areas of epithelial metaplasia, focal lymphohistiocytic infiltration in the submucosal layer. Reticuloendothelial system - Warthin-Finkeldey cells. Skin - changes in the papillary layer of the dermis in the form of edema, congestion of blood vessels, hemorrhages with perivascular lymphohistiocytic infiltration, foci of necrosis in the epidermis.
What is measles in adults
An infectious disease caused by a specific RNA virus from the morbillivirus group is called measles. As a rule, the pathogen enters the body through airborne droplets. The disease is much more severe in adults than in children. There are three degrees of measles:
- Easy. Body temperature remains within subfebrile values (37-38°C), the rash does not completely cover the body, patients note rare bouts of mild cough.
- Average. The patient has a temperature above 39 °C, the urge to vomit, and a severe cough. An infected person's face swells and a bright red rash appears on the body.
- Heavy. Characterized by high body temperature (more than 39 °C), convulsions, vomiting, symptoms of respiratory failure (shortness of breath, pale skin, bluish lips).
Measles symptoms do not appear immediately after infection. The classic clinical course of measles is divided into several periods:
- Incubation. The time from the entry of the virus into the body to the first symptoms of the disease. In most cases, it ranges from 7 to 21 days, but can vary depending on the state of the person’s immune system and concomitant diseases.
- Catarrhal. During the catarrhal stage, the first symptoms of measles appear: body temperature rises, cough, runny nose.
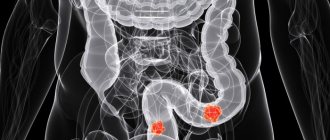
- Stage of rash. On the fifth or sixth day from the onset of the disease, characteristic rashes (Koplik-Filatov spots) begin to appear on the skin, which spread from top to bottom: first on the face, behind the ears, then on the torso, arms, legs.
- Pigmentation period. Characterized by a decline in symptoms. The rash takes on a dark brown-bluish tint. The stage lasts about a week.
- The period of recovery (reconvalescence). During this period, the disease regresses and the person begins to recover. Body temperature gradually decreases, the rash peels off. The convalescence stage can last up to two weeks.
Clinical picture of typical measles
Belsky-Filatov-Koplik spots on the inner surface of the cheek
Incubation period
8-14 days (rarely up to 17 days). Acute onset - a rise in temperature to 38-40 ° C, dry cough, runny nose, photophobia, sneezing, hoarseness, headache, swelling of the eyelids and redness of the conjunctiva, hyperemia of the pharynx and measles enanthema - red spots on the hard and soft palate. On the 2nd day of illness, small whitish spots appear on the mucous membrane of the cheeks in the area of the molars, surrounded by a narrow red border - Belsky-Filatov-Koplik spots - pathognomonic for measles. A measles rash (exanthema) appears on the 4-5th day of illness, first on the face, neck, behind the ears, the next day on the torso and on the 3rd day the rash covers the extensor surfaces of the arms and legs, including the fingers. The rash consists of small papules surrounded by a spot and prone to merging (this is its characteristic difference from rubella, the rash in which does not merge).
The reverse development of the elements of the rash begins on the 4th day of the rash: the temperature returns to normal, the rash darkens, turns brown, becomes pigmented, and peels off (in the same sequence as the rash). Pigmentation lasts 1-1.5 weeks.
Diagnosis of measles in children
Diagnosing a child with measles is not difficult. The main stages of diagnosis are:
- careful history taking - contact with sick children, cases of measles outbreaks in kindergarten or in the environment;
- complaints from parents and children;
- the appearance of characteristic rashes;
- the presence of Belsky-Filatov-Koplik spots on the mucous membranes of the mouth, palate and gums in the area of the molars.
Sometimes measles in children occurs atypically, without pronounced characteristic clinical symptoms. In this case, to make a diagnosis, additional laboratory tests are required - a virological blood test, a serological test, a chest x-ray if complications of measles are suspected.
Treatment
No drugs have been developed for the specific treatment of measles.
Symptomatic treatment includes expectorants, mucolytics, and anti-inflammatory aerosols to relieve inflammatory processes in the respiratory tract.
To reduce fever and pain, you can use ibuprofen or paracetamol. Children with measles are not recommended to take aspirin because some studies have suggested that aspirin may cause Reye's syndrome.[14] Other researchers have questioned the connection between the development of Reye's syndrome and the use of aspirin in the treatment of measles[15]. However, most doctors recommend against using aspirin to treat measles and other febrile illnesses in children under 16 years of age[16].
To relieve itching on the skin, daily rinsing of the body and washing with a solution containing Delaskin powder (synthetic tannin) are recommended [17].
To wash your eyes during illness, you can use a solution of baking soda or strong tea. For conjunctivitis, drops with antibiotics are recommended (levomycytin 0.25%, albucid 20%).
The oral cavity can be rinsed using chamomile infusion and chlorhexidine solution.
In case of pneumonia or other bacterial complications of measles, antibiotics are indicated; in severe cases of croup, corticosteroids are used.
Ribavirin showed [ source not specified 891 days
] its effectiveness
in vitro
. One of the side effects is dose-dependent hemolytic anemia, which in its advanced form causes the death of the patient (and therefore requires total monitoring of blood counts during treatment)
The World Health Organization recommends the use of vitamin A in the treatment of measles to reduce the risk of mortality[18][19][20][21].
Symptoms
With measles in adults, the clinical picture is the same as in children, but the symptoms are more pronounced. The main manifestations are:
- increase in body temperature (fever) up to 38-40 °C;
- weakness;
- headache;
- decreased appetite;
- hard breathing;
- conjunctivitis;
- inflammation of the upper respiratory tract;
- hacking dry cough;
- hoarseness of voice;
- large red or pink spots on the roof of the mouth (measles enanthema);
- rash and pigmentation on the entire skin;
- disturbance of consciousness (delirium, fainting, etc.);
- peeling, skin pigmentation;
- bruising;
- intestinal dysfunction.
Prevention
Accelerated immunization efforts have had a significant impact on reducing measles deaths. Global deaths from measles fell by 73%, from 548,000 deaths in 2000 to 145,700 deaths in 2013. Two doses of the vaccine are recommended to provide immunity and prevent outbreaks, as approximately 15% of vaccinated children do not develop immunity after the first dose[22].
In accordance with the Russian national vaccination calendar, which was approved by order of the Ministry of Health of the Russian Federation No. 125n dated March 21, 2014[23], vaccination against measles is carried out with a combined live vaccine against measles, rubella and mumps simultaneously at the age of 12 months, revaccination - at 6 years .
In accordance with the same order, vaccination against measles and revaccination against measles are indicated for all children and adults aged 1 to 35 years if they have not been sick, are not vaccinated, have been vaccinated once against measles, or do not have information about vaccinations against measles . In the age category of 36-55 years, under the same conditions, measles vaccination is indicated for representatives of certain professions.
The measles vaccine is very effective[24]. After one dose, 85% of nine-month-old children and 95% of twelve-month-old children are immune[25]. Almost everyone who does not develop immunity after the first dose becomes immune after the second dose.[24]
Once vaccination coverage in an area is greater than 93%, measles outbreaks typically no longer occur, but they may recur if coverage declines.[24].
The protective effect of the vaccine lasts for many years[24]. It remains unclear whether it becomes less effective over time[24]. In addition, the vaccine may protect against disease when administered within a few days of infection[24].
Safety
The vaccine is generally safe, including for patients with HIV infection[24]. Side effects are usually mild and disappear quickly[24]. These include pain at the injection site or mild fever[24]. One case of anaphylaxis has been reported in approximately one hundred thousand vaccinations[24]. There was no increase in the incidence of Guillain-Barré syndrome, autism, or inflammatory bowel disease[24].
Dosage form
The vaccine is used alone or in combination with other vaccines, including rubella vaccine, mumps vaccine, and varicella vaccine (in the combination MMR and MMRV vaccines)[24]. The vaccine works equally well in all dosage forms[24]. The World Health Organization recommends vaccination for children at nine months of age in areas where the disease is common, and at twelve months of age in areas where the disease is rare[24]. This is a live vaccine[24]. The vaccine is produced in the form of a powder, which must be mixed immediately before administration subcutaneously or intramuscularly[24]. The effectiveness of the vaccine is checked using a blood test[24].
In case of illness, all unvaccinated contact persons over 1 year of age are given emergency vaccine prophylaxis; if there are contraindications, immunoglobulin is administered.
In order to create active immunity, routine vaccination with live measles vaccine (LMV) is carried out in accordance with the vaccination calendar, as well as for children and adults in the absence of measles antibodies. The complex of anti-epidemic measures in the outbreak of infection includes identifying the source of infection, contacts who had the fact of unconditional or probable communication with the patient, to establish the boundaries of the outbreak.
The source of infection is isolated for the entire infectious period (until the 4th day of the rash). Children who were in contact with him and adults working with children (with the exception of persons who have previously had measles, who have been vaccinated, who are seropositive with a titer of anti-measles antibodies of 1:5 or higher) are subject to separation from other children for 17 days (with the introduction of immunoglobulin - 21 days ).
Emergency prophylaxis with normal human immunoglobulin is carried out in the first 5 days after exposure to children from 3 to 12 months. and pregnant women.
A differentiated serological examination is desirable to identify seronegative individuals followed by vaccination with LCV or other measles vaccines.
Treatment and vaccination against measles
To date, no drug has been obtained that would specifically target the virus of the disease. Treatment of measles is usually carried out symptomatically. Both medications and traditional medicine are allowed.
Under no circumstances prescribe any medications for yourself - medications may not be compatible.
Complex treatment includes drugs from the following groups:
- antiviral - they are prescribed when the disease has a slow rate of increase, with their help you can ease the symptoms;
- antipyretics - it is better to use those medications that can lower the temperature and stop inflammation. It is advisable to avoid Aspirin: it affects blood clotting, which can cause internal bleeding;
- antihistamines - with their help they get rid of itching and swelling. It is recommended to use 1st and 2nd generation drugs, which additionally have sedative properties;
- mucolytic - prescribed to suppress cough.
If you have a sore throat, take lozenges or a spray. Stinging in the eyes can be relieved with anti-inflammatory eye drops, sometimes containing an antibiotic.
If treatment occurs in a hospital setting, measles immunoglobulin may be prescribed.
Adults receive a free measles vaccination only up to the age of 35; in all other cases, this service is paid. Depending on the vaccine, its cost ranges from 450 to 1.5 thousand rubles.
There are several types of vaccines:
- monovalent;
- two- or three-component.
Adults should be vaccinated in the following cases:
- You will be traveling to a country with a high risk of contracting measles.
- A woman is planning a pregnancy, but she has not had measles before.
- Returning from the epidemic zone.
- Previous contact with the patient.
WHO plan for global measles elimination
Measures to combat measles undertaken by WHO (mass vaccination) led to a decrease in global measles mortality from 2000 to 2014 by 79%, that is, almost five times. By 2020, it was planned to reduce mortality from measles by 95% (20 times) compared to 2000, and by 2020 to completely eliminate measles (as well as rubella) in at least five WHO regions[26].
WHO experts note that the reason for the current situation was a sharp decline in measles vaccination rates, especially in marginalized groups in several European countries.[27]
Diagnosis of the disease
Measles is diagnosed based on the symptoms characteristic of this disease and the results of laboratory tests, including ELISA - enzyme-linked immunosorbent test and general blood test. Sometimes virological diagnostic methods (immunofluorescence reaction, virus microscopy) are used to determine the causative agent of this disease in the human body.
A general blood test for measles is characterized by a low content of leukocytes (the number of fractions of lymphocytes, monocytes, neutrocils decreases), a high ESR, and when a secondary bacterial infection is added, leukocytosis appears with an increased content of the neutrophil fraction.
When performing ELISA, the disease can be determined in the initial period. This test can detect antibodies to the measles virus (immunoglobulins IgM, IgG), which are produced when the causative agent of this disease enters the human body. On days 1-2 after infection, the concentration of IgM in the patient’s blood begins to increase, and from the 10th day of illness, the IgG level increases.
- Recipe for a delicious assortment of cucumbers and tomatoes for the winter
- How to find your phone if it is turned off and lost
- Vinegar against nail fungus
Some symptoms in the catarrhal period of this disease are similar to a number of other infectious diseases (rubella, influenza, whooping cough, rhinovirus or adenovirus infection). Measles is distinguished from other viral infections by the following characteristics: the presence of conjunctivitis, the appearance of Belsky-Filatov-Koplik spots on the 2-3rd day of the catarrhal period, general intoxication against the background of increased symptoms.
Notes
- World Health Organization: Measles. Newsletter No. 286, February 2013
- The incidence of measles in Russia in 2020 decreased by almost six times
- Mark Reimers.
Recent evolutionary changes in the human genome. Retrieved January 8, 2020. - The cause of the measles epidemic in the Netherlands was religious fundamentalists, Lenta.ru (September 12, 2013). Retrieved January 28, 2014.
- https://www.rospotrebnadzor.ru/about/info/news/news_details.php?ELEMENT_ID=8196
- The European Region has seen a record high number of measles cases (Russian). www.euro.who.int (20 August 2018). Retrieved August 22, 2020.
- RKI (Robert Koch Institut), Sentinel der Arbeitsgemeinschaft Masern (AGM) - aktuelle Ergebnisse, Epidemiologisches Bulletin, 37, 2000, 297
- Measles and atopy in Guinea-Bissau. [Lancet. 1996] - PubMed - NCBI
- Frequency of allergic d... - PubMed - NCBI
- Allergic disease and atopic sensitization in children... [Pediatrics. 2009] - PubMed - NCBI
- Early atopic disease and early childhood immunization… [Allergy. 2008] - PubMed - NCBI
- Acute infections, infection pressure, and a… - PubMed - NCBI
- Age at childhood infections and risk of atopy
- Starko KM, Ray CG, Dominguez LB, Stromberg WL, Woodall DF
Reye's syndrome and salicylate use. (English) // Pediatrics. - 1980. - Vol. 66, no. 6. - P. 859-864. - PMID 7454476. - Casteels-Van Daele M., Van Geet C., Wouters C., Eggermont E.
Reye syndrome revisited: a descriptive term covering a group of heterogeneous disorders. (English) // European journal of pediatrics. - 2000. - Vol. 159, no. 9. - P. 641-648. — DOI:10.1007/PL00008399. - PMID 11014461. - Schrör K.
Aspirin and Reye syndrome: a review of the evidence. (English) // Paediatric drugs. - 2007. - Vol. 9, no. 3. - P. 195-204. — DOI:10.2165/00148581-200709030-00008. - PMID 17523700. - Fölster-Holst R., Latussek E.
Synthetic tannins in dermatology—a therapeutic option in a variety of pediatric dermatoses. (English) // Pediatric dermatology. - 2007. - Vol. 24, no. 3. - P. 296-301. — DOI:10.1111/j.1525-1470.2007.00406.x. - PMID 17542884. - Strategies for reducing global meat mortality. (French) // Releve epidemiologique hebdomadaire / Section d'hygiene du Secretariat de la Societe des Nations = Weekly epidemiological record / Health Section of the Secretariat of the League of Nations. - 2000. - Vol. 75, no 50. - P. 411-416. - PMID 11189704.
- Huiming Y., Chaomin W., Meng M.
Vitamin A for treating meats in children. (English) // The Cochrane database of systematic reviews. - 2005. - No. 4. - P. 001479. - DOI:10.1002/14651858.CD001479.pub3. - PMID 16235283. - Measles vaccines: WHO position paper. (French) // Releve epidemiologique hebdomadaire / Section d'hygiene du Secretariat de la Societe des Nations = Weekly epidemiological record / Health Section of the Secretariat of the League of Nations. - 2009. - Vol. 84, no. 35. - P. 349-360. - PMID 19714924.
- Moss WJ, Griffin DE
Measles. (English) // Lancet. - 2012. - Vol. 379, no. 9811. - P. 153-164. — DOI:10.1016/S0140-6736(10)62352-5. - PMID 21855993. - Measles Fact sheet N°286. who.int
(November 2014). Retrieved February 4, 2020. - Order of the Ministry of Health No. 125n dated March 21, 2014 “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications.” With changes and additions until June 16, 2020 (Russian). garant.ru. Retrieved December 7, 2020.
- ↑ 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17
(28 August 2009) “Measles vaccines: WHO position paper.”.
Weekly epidemiological record 84
(35): 349–60. PMID 19714924. - Control, Centers for Disease.
CDC health information for international travel 2014 the yellow book / Centers for Disease Control, Prevention. - 2014. - P. 250. - ISBN 9780199948505. - Measles.. Newsletter N°286 (Russian). WHO (March 2016). Retrieved May 2, 2020.
- https://www.remedium.ru/news/detail.php?ID=74843
Links
| measles in Wiktionary |
| Measles on Wikimedia Commons |
In English
- https://www.nlm.nih.gov/medlineplus/measles.html
- https://www.kidshealth.org/parent/infections/lung/measles.html
- https://www.nlm.nih.gov/medlineplus/ency/article/001569.htm
- https://web.archive.org/web/20150805090051/https://www.cdc.gov/ncidod/diseases/submenus/sub_measles.htm
- https://www.netdoctor.co.uk/diseases/facts/measles.htm
- Center for Disease Control and Prevention
In Russian
- Manual for laboratory diagnosis of measles and rubella (Russian) (pdf). WHO. Retrieved April 14, 2020.
- Measles, educational film
Literature
- Measles // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907.
- Dobrokhotova A.I.
Measles and the fight against it. - M.: Medgiz, 1959. - 160, [20] p. — 20,000 copies. (in translation) - Handbook of infectious diseases in children. Edited by Professor L. A. Trishkova, Associate Professor S. A. Bogatyreva. Kyiv
- Pathological anatomy of diseases of the fetus and child. A. A. Birkun, V. V. Vlasyuk, P. S. Gurevich, B. S. Gusman and others; Ed. T. E. Ivanovskaya, L. V. Leonova. Moscow Medicine.
- Handbook of differential diagnosis of infectious diseases. Edited by Professor A.F. Frolov, Professor B.L. Ugryumov, Dr. med. Sciences E.K. Trinus. Kyiv
- Harrison's Principles of Internal Medicine 14th edition - Measles (Rubeola) - Anne Gershon.
- Pathologia AUTH. Medical School, Thessaloniki Greece. Edition — professor M. Papadimitriou
- Guide for the local pediatrician. S. Sh. Shamsiev, N. P. Shabalov, L. V. Erman