The natural and most favorable position of the fetus before childbirth is the head-down position. If the buttocks are facing the exit of the uterus, doctors diagnose breech presentation. This situation makes the birth process difficult for both mother and child. Before the doctor makes a decision about delivery, it is necessary to evaluate possible claims and conduct a more detailed diagnosis.
Now let's look at this in more detail.
What is “breech presentation”?
Breech presentation is the longitudinal position of the fetus in the uterus, in which the buttocks face the exit. In approximately 5% of pregnant women, the baby is breech before birth. During natural childbirth, this requires a special approach and highly qualified assistance. Since the baby’s buttocks and legs pass through the birth canal first, the likelihood of rupture and injury to the mother’s mucosa increases.
Despite the fact that natural childbirth with a breech presentation is possible, this position of the child is considered pathological due to the fact that the likelihood of injury and death is increased. Childbirth is easier and safer when the baby moves forward with the widest part of the body - the head, after which the torso and limbs slide well through the birth canal.
What is the best way to give birth with TPP?
It is impossible to answer this question unequivocally. Most women strive for natural childbirth, which is quite justified. Despite the fact that the vast majority of women in labor with TPP undergo CS, spontaneous childbirth is still possible, especially if:
- fetal weight ranges from 1.8 to 3.5 kg;
- there is one fetus, in a breech position;
- pelvic dimensions correspond to the norm;
- the cervix is mature;
- childbirth occurs no earlier than 36 weeks.
During childbirth at 7-8 months, a caesarean section is indicated.
Surgical intervention minimizes the risk of fetal trauma, development of congenital disease, and even death. At least a third of women in labor who insist on the natural method experience an urgent need for surgery during childbirth. Indications for this include: prolapse of the umbilical cord, early breaking of water, weak labor, throwing back of the baby’s arms, which complicates the exit of the head.
What does a breech presentation of a fetus look like with a photo?
Breech presentation has several varieties:
- Gluteal. The baby’s buttocks are adjacent to the exit from the uterus, while the legs are bent at the hip joints. The baby's head and arms are pressed to the chest in this position.
- Foot. The exit from the uterus does not touch the baby’s buttocks, but the feet or knees.
Examples of breech presentation are shown in the photo:
Pure breech presentation occurs in 60% of cases. The position of the fetus begins to be preliminarily determined from the 32nd week of pregnancy. However, the likelihood of a baby turning from a breech presentation to a cephalic presentation remains until birth.
General characteristics and types of Chamber of Commerce and Industry
About 4-5 women in labor out of 100 are faced with the problem of TPP. Carrying out such a pregnancy should be accompanied by more frequent and thorough diagnostics, performing certain exercises, and undergoing drug therapy. How difficult the birth will be depends on the experience and qualifications of the doctor.
With a breech presentation of the fetus, there are 2 positions:
- Foot. It is diagnosed when the legs go first through the birth canal. If the necessary measures are not taken in time, childbirth is fraught with severe pain and injury to the mother, as well as trauma to the baby. In such a situation, the obstetrician must forcibly delay the birth of the child, giving him the opportunity to change position. The leg form of TPP can be knee (knees forward), complete (two legs) and incomplete (one of the legs).
- Gluteal. A safer position, which is observed in 80-85% of all cases of TPP. Most often, only the buttocks are adjacent to the exit, while the legs are located along the body. Another type involves bent knees, which causes the buttocks and legs to move out at the same time. Often, specialists insist on performing a cesarean section to avoid large ruptures and other dangerous consequences.
The baby's head is the largest and densest part; it is the one that contributes to the natural opening of the cervix during a typical birth with a cephalic presentation. In the case of the pelvic version, the head comes out last, preventing the uterus from taking its normal position. This key factor causes complicated childbirth.
Symptoms of breech presentation of the fetus
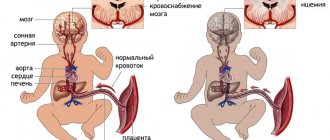
Starting from the 33rd week, with a breech presentation, there is not enough space for the baby’s head to fully develop. Because of this, delayed maturation of brain structures occurs and tissue swelling occurs. Quite often after birth, children were diagnosed with a decrease in adaptive properties and depletion of the adrenal cortex.
There may be disturbances in the development of the genital organs due to improper hemodynamics of the fetus. With breech presentation, the likelihood of malfunction of the cardiovascular system, gastrointestinal tract and musculoskeletal system also increases.
Uteroplacental blood flow is difficult during breech presentation, which leads to fetal hypoxia and a decrease in its motor activity. Squeezing of placental vessels and hypoxia can dramatically worsen the child’s health and lead to a critical situation.
Possible complications of TPP
Abnormal presentation inevitably affects the condition of the baby, placenta and internal genital organs of the pregnant woman. The most common complications:
- threat of spontaneous termination of pregnancy;
- gestosis, accompanied by increased blood pressure, swelling, convulsions, loss of protein in the urine;
- fetoplacental insufficiency is a change in the structure of the placenta and its basic functions due to impaired blood circulation.
As a result, all systems of the fragile body suffer. At the 8th month, problems begin with the maturation of the structures of the posterior part of the brain, dysfunction of the adrenal cortex occurs, and protective reactions worsen. During the examination, doctors can diagnose a rapid heartbeat and decreased activity. There is also a high probability of weak labor.
Causes and prevention of breech presentation of the fetus
Due to the ovoid shape of the uterus and the similar shape of the fetus, the baby naturally takes a cephalic presentation. A change in the normal position can occur for several reasons:
- Mother has problems. These may be abnormalities in the development of the uterus, a narrow pelvis, the presence of tumors, a history of multiple curettages, inflammatory processes in the vagina and uterus. Overwork, stress, and neurocirculatory dystonia can lead to a change in the tone of the myometrium, which will prevent the child from taking the correct position.
- Fetal pathologies. This includes prematurity, abnormalities of the central nervous system, heart defects and others.
- Placental disorders - placenta previa, short umbilical cord, change in the volume of amniotic fluid.
Some medical sources provide evidence that a predisposition to breech birth can be inherited.
Methods for preventing breech presentation are still unknown. It is believed that the correct lifestyle of a pregnant woman and the absence of stress will contribute to the normal course of pregnancy and the natural position of the baby with its head down. Physical exercises that lead to the correct position of the head are quite effective. Their essence lies in the use of gravity, thanks to which the head, as the heaviest part of the child, descends into the mother’s pelvis.
Antecedent factors
During pregnancy, the reproductive organ takes on an ovoid shape (the upper part is slightly wider than the lower). During the process of growth, the fetus adapts to the prevailing “circumstances”, so the pelvic part is placed at the top, and the head is pressed against the exit of the uterus. If any obstacles appear, the child’s position may change. The causes of breech presentation of the fetus can be:
- benign and malignant tumors of the genital organs;
- abnormal development of the pelvis and uterus;
- numerous pregnancies, artificial births, curettage;
- scars on the uterus, stress conditions;
- pathological location of the placenta, covering the internal os;
- polyhydramnios, causing excessive mobility;
- prematurity, hydrocephalus, asphyxia, other pathologies.
The hereditary factor plays a special role. The vast majority of women born with TPP experience the same complication during pregnancy. After the birth of the first child with breech presentation, the risk of developing a similar situation in the future is about 25%.
Diagnostics
The likelihood of the baby turning over remains until birth. However, we can talk about the stable position of the fetus starting from the 35th week of pregnancy. Breech presentation can be detected by external obstetric examination, vaginal examination, and also by ultrasound.
In a breech presentation, the baby does not descend into the pelvic cavity as much as he does with his head down. Because of this, the pathology is characterized by a higher standing of the uterine fundus at a time when this should not be observed.
In the womb area, the gynecologist probes the soft and inactive part of the fetal body, making the assumption that it is not the head, but the buttocks. In this case, near the bottom of the uterus, on the contrary, there is a large, round and hard part.
It is important to distinguish breech presentation from frontal and facial presentation, so the woman is always prescribed an additional ultrasound examination.
Tactics for pregnancy management with breech presentation
When identifying a breech presentation, the gynecologist must carefully influence the position of the fetus and try to change it naturally. This can be done starting from week 32, strictly following the recommendations of your doctor. The main attention is paid to a set of gymnastic exercises, which affects the tone of the muscles of the anterior abdominal wall and uterus, causing the fetus to turn over.
If the pregnancy is normal and the fetus is breech, the woman is hospitalized for observation at 38-39 weeks. In case of a complicated pregnancy (narrow pelvis, large fetus, concomitant pathologies), the woman is hospitalized at 37 weeks.
One way to change the child’s position is to externally roll over. The technique is considered quite safe and effective, so it is often used in the third trimester for breech presentation. If the manipulation is successful, the probability of a reverse coup is only 4%. It is recommended to do this at 34-35 weeks. The manipulation is performed by a gynecologist.
In most cases, with breech presentation, preference is still given to cesarean section. This is due to the high incidence of complications and adverse outcomes.
When choosing delivery tactics, the gestational age, fetal weight, head position, pelvic size, cervical maturity and other factors are taken into account.
Natural childbirth is usually allowed with a purely breech position, a small fetus and normal maternal pelvic dimensions. During the period of contractions during breech presentation, it is recommended not to walk, but to lie down with the foot end of the bed raised. After the water breaks, the doctor checks to see if the placenta or baby's legs have fallen out. If everything goes well, the first stage of labor is carried out under careful monitoring of CTG and uterine contractility. In the second period, oxytocin may be administered to prevent labor weakness. When the buttocks erupt, an episiotomy is usually performed and manual assistance is provided.
Pregnancy management
Fetal presentation is formed by 32 weeks. Breech presentation detected before the third ultrasound screening does not require treatment. Turning of the fetus onto its head occurs spontaneously in most pregnant women.
The final diagnosis is made at 36 weeks. But even in this case, 8% of women experience spontaneous rotation of the fetus before the natural birth date. To clarify the location of the baby in the uterine cavity, you need to repeat the ultrasound at 40-41 weeks or earlier when labor starts.
If breech presentation is detected at 36 weeks, it is recommended:
- Assessment of risk factors. Other possible contraindications for natural childbirth are identified. A woman should be informed about the high risk of complications during vaginal birth.
- Physiotherapy. Prescribed at 28-30 weeks, practiced up to 36 weeks.
- External obstetric rotation of the fetus. It is carried out at 36 weeks only in a hospital setting with the possibility of performing an emergency caesarean section.
Physiotherapy
Therapeutic gymnastics exercises are performed independently or under the guidance of an instructor. Primiparous women are recommended to study in groups.
The Dikan method is practiced from 28 weeks of gestation. Lying on a hard bed or couch, a pregnant woman turns alternately on each side and remains in this position for 10 minutes. The procedure is repeated 3-5 times three times a day before meals.
The Fomicheva method is prescribed from 32 weeks. First, a warm-up is carried out (walking on your toes and heels, raising your knees high). Next, the pregnant woman needs to take the starting position - feet shoulder-width apart, arms down. From this position the following exercises are done:
- tilt to the side - left and right alternately;
- make a slight bend back, bend at the lower back;
- spread your arms to the sides as you inhale, turn your torso, bring your arms together as you exhale;
- raise the leg bent at the hip and knee joint, touching the hand.
Once the fetal head is positioned at the entrance to the pelvis, it is recommended to wear a bandage until the date of natural birth. Wearing a brace keeps the child in the desired position and prevents relapse.
A large number of different techniques have been proposed for turning the fetus onto its head, but their effectiveness has not been proven. The likelihood of spontaneous fetal revolution is low. But there will be no harm from therapeutic exercises. The proposed exercises give strength to the muscles, improve the general condition of the woman and serve as good preparation for the upcoming birth.
External obstetric turn
Indications:
- pregnancy period from 36 weeks;
- singleton pregnancy;
- mobility of the fetal buttocks;
- bent position of the fetal head;
- normal amount of amniotic fluid;
- satisfactory condition of the fetus according to ultrasound and CTG.
Contraindications:
- multiple pregnancy;
- polyhydramnios or oligohydramnios;
- rupture of amniotic fluid;
- extension position of the fetal head;
- immobility of the fetal buttocks;
- abnormalities of the uterus;
- fetal malformations;
- chronic fetal hypoxia;
- presence of indications for caesarean section.
Preparation:
- Introduction of tocolytics - drugs that relax the muscle layer of the uterus.
- Breech presentation, the location of the placenta and umbilical cord are confirmed again by ultrasound. An ultrasound examination is performed no later than one day before the procedure.
- CTG to assess the condition of the fetus.
- Woman emptying her bladder.
External rotation is performed by a doctor. The doctor places one hand on the fetus’s buttocks, the other on the head, and pushes it into the desired position. If the first attempt fails, you can repeat the manipulations. After completion of the procedure, a control ultrasound and CTG are performed. The woman remains under observation in the hospital for 24 hours, after which she is discharged home.
Rotation of the fetus is accompanied by some discomfort for the woman. The severity of unpleasant sensations depends on the individual threshold of sensitivity. The total duration of the procedure is no more than 5 minutes.
External rotation is carried out under constant monitoring of the fetal heartbeat. If bradycardia develops (heart rate less than 120 beats per minute), manipulations are stopped.
Complications:
- fetal bradycardia as a result of clamping or twisting of the umbilical cord;
- placental abruption;
- premature rupture of amniotic fluid;
- launch of labor.
The efficiency of external rotation is 60-70%. The longer the pregnancy, the higher the failure rate.
Complications of childbirth with breech presentation
The birth itself with breech presentation often occurs with complications:
- Premature rupture of water. Umbilical cord prolapse and early breaking of water are common in breech presentation. Since the buttocks do not fill the mother’s pelvic area tightly enough compared to the head.
- Hypoxia. Compression of the umbilical cord by the fetal pelvis leads to poor circulation and lack of oxygen in the child. This condition requires emergency measures due to the high probability of brain damage to the child and even death.
- Weakness of labor. Due to weak contractions, labor becomes protracted, and the fetus suffers from a lack of oxygen.
- Difficult birth of the head. This can happen for various reasons (discrepancy between the sizes of the mother’s head and pelvis, hyperextension).
After childbirth, the following complications are possible due to incorrect fetal position:
- intracranial injuries;
- hip dysplasia;
- encephalopathy;
- fetal hypoxia;
- damage to the birth canal (women often experience ruptures of the vagina, cervix and perineum);
- damage to the pelvic bones.
Management of childbirth
The tactics of labor management during T. p.p. depend on the woman’s age, obstetric history, the readiness of the mother’s body for childbirth, the size of the pelvis, the state of the amniotic sac, the functional state and size of the fetus, the type of breech presentation and other points. To resolve the issue of choosing a method of delivery (via the natural birth canal or by cesarean section), a prognostic index proposed in 1967 by GI Zatuchni and GJ Andros is used. This takes into account the outcomes of past pregnancies, the duration of the current pregnancy, the estimated weight (mass) of the fetus, a history of breech presentation, cervical dilatation, and the location of the presenting part of the fetus.
If the pregnant woman and fetus are in good condition, the pelvis is normal and the fetus is of average size, childbirth should be carried out through the natural birth canal. The first stage of labor (dilation period) with T. p.p. differs from that with cephalic presentation in that the head comes last. As a result, the birth canal does not dilate sufficiently and remains ill-prepared for childbirth, which can lead to a number of complications: throwing back of the arms, head retention with subsequent fetal hypoxia, compression of the umbilical cord, formation of a posterior view and retention of the head by the chin above the pubic symphysis and asphyxia of the newborn (see Fetal asphyxia and newborn). It should be noted the high frequency of untimely amniotic fluid from lithium (see Premature rupture of water), prolapse of small parts of the fetus and umbilical cord loops, fetal hypoxia, protracted labor, and fetal infection.
In order to prevent early opening of the membranes, the woman in labor must observe bed rest. Childbirth with T. p. p. should be carried out with monitor observation (see) of the fetal heartbeat. When regular labor is established and the cervix is opened by 3-4 cm, in order to anesthetize labor and regulate labor, intramuscular administration of analgesics (promedol) and antispasmodics (no-spa, aprofen) is indicated, as well as the use of electroanalgesia with pulsed currents (see Anesthesia childbirth).
To prevent fetal hypoxia, the Nikolaev method is used (see Childbirth), and 2 ml of 1% sigetin solution, 0.05 g of cocarboxylase are administered intravenously, and 0.5 g of galascorbine is given orally. After the amniotic fluid is released, a vaginal examination is immediately performed to clarify the diagnosis and exclude prolapse of small parts of the fetus and umbilical cord loops. In cases of labor disturbances, more often than in cases of cephalic presentation of the fetus, delivery by cesarean section is indicated (see).
In the second stage of labor (expulsion period), oxytocin is administered intravenously for prophylactic purposes, and by the end of the second period, antispasmodics (no-spa, papaverine hydrochloride) are administered to prevent cervical spasm. When the buttocks erupt, pudendal anesthesia is performed, then perineo- or episiotomy is performed (see Perineotomy). During the expulsion period with breech presentation, a noticeable acceleration of the fetal heartbeat is often observed.
When an umbilical ring appears in the genital slit, an extremely dangerous moment occurs for the fetus, because the head, entering the pelvis, inevitably compresses the umbilical cord, and the fetus faces asphyxia. The danger increases at the moment of birth of the head. The umbilical cord can be pressed for no more than 3-5 minutes. If the umbilical cord is compressed for more than 10 minutes. the fetus usually dies. At this time, premature placental abruption may also occur (see).
If the fetus is in good condition, they usually provide manual assistance according to Tsovyanov (see below), and, if necessary, classic manual assistance or extraction of the fetus by the pelvic end. With classic manual assistance, the birth of the shoulder girdle and head is promoted. When extracting the fetus by the pelvic end, all moments of labor during breech presentation are artificially reproduced, and the fetus is removed after the presenting part appears from the genital slit.
Manual manual according to Tsovyanov. With a purely breech presentation, the essence of the aid is to maintain the normal position of the fetal legs (flexion at the hip joints and extension at the knee joints).
After the birth of the buttock facing anteriorly, the obstetrician wraps his thumbs around the fetal hips (the remaining fingers are in the sacrum area). As the fetal body is born, the doctor carefully presses the fetal legs to its abdominal wall, gradually moving his hands towards the mother’s genital slit, which prevents the fetal legs from falling out, as well as the arms being thrown back behind the head, pressed to the chest by the feet of the legs extended along the body. The fetus is gradually born up to the umbilical ring, and then to the lower angle of the shoulder blades. In addition to the translational one, the fetus makes a rotational movement, and the shoulders transform into the direct size of the pelvic outlet. The anterior shoulder is the first to fit under the pubic arch. To facilitate the birth of the anterior handle from under the pubic arch, it is recommended to direct the buttocks somewhat posteriorly (downwards), to the corresponding thigh of the woman in labor (in the first position - to the left). To birth the posterior arm, the fetus is lifted upward (anteriorly). Removing the subsequent head is usually not difficult; To do this, it is enough to direct the fetal buttocks anteriorly (upward). Usually, after the birth of the shoulder girdle, the chin appears from the genital slit, and the head is born on its own. If the birth of the head does not occur, it is usually removed manually (abroad - according to the Bracht method, in our country - according to the Morisot-Levret-Lachapelle method - see below).
Rice. 3. Schematic representation of Tsovyanov’s manual aid for leg presentation of the fetus: the obstetrician’s palm, pressed to the genital slit, covered with a sterile diaper, counteracts the premature birth of the legs.
In case of foot presentation, manual assistance according to Tsovyanov comes down to preventing the birth of the fetal legs until the uterine os is fully dilated. To do this, by covering the genital slit of the woman in labor with a sterile diaper, the palmar surface of the right hand, applied to the genital slit, prevents the premature birth of the legs (Fig. 3). During each attempt, the fetus seems to “squat down” inside the birth canal. In this regard, the buttocks put pressure on the cervical canal and promote its opening. In this case, a mixed breech presentation is formed. Counteraction to the birthing legs should be provided until the uterine os is fully dilated. After the uterine os is fully opened, there is no longer any resistance to the legs, and the buttocks and torso of the fetus, which are born after the legs, do not encounter difficulties due to the good preparedness of the birth canal. After birth, manual assistance is provided to the lower corners of the shoulder blades, as with a breech presentation. When carrying out this method, you should carefully monitor the fetal heartbeat, the height of the contraction ring, and the condition of the lower segment of the uterus. In case of prolapse of the legs and incomplete opening of the uterine pharynx, they also begin to provide manual assistance according to Tsovyanov.
Rice. 4. Schematic representation of the position of the obstetrician’s hands during classical manual assistance during breech presentation of the fetus: a - grasping the fetus in the hip area (first stage); b — position of the obstetrician’s hands when turning the fetus 180° (second stage); c — position of the obstetrician’s hands when releasing the back handle (second stage); d - release of the head using the Morisot-Levret-Lachapelle method (third stage).
The classic manual manual is a set of measures aimed at the birth of the shoulder girdle and head. The fetus is born independently up to the umbilical ring. After the birth of the fetus, the umbilical cord should be examined up to the navel (pulsation, tension). Strong tension should be released; if this fails, it is necessary to cut the umbilical cord and hasten the end of labor. By the time the fetus is born, everything should be prepared to provide manual assistance up to the navel. If you start releasing the arms earlier, it may be difficult for the doctor to reach the fetal arms with his fingers; if you pull too hard on the pelvic end, the arms may tip over the head. There are three stages in the provision of classic manual assistance. The first stage is from the navel to the lower corner of the scapula. The fetus is grabbed with both hands in the hip area (Fig. 4, a), and the body is transferred to the direct size of the outlet from the pelvis and reduced until the lower angle of the scapula appears in the genital slit.
The second stage - releasing the handles - is carried out according to the following rules: the obstetrician releases each handle with the same hand (the right handle - with the right hand, the left - with the left), the back handle is always released first (more space in the sacral cavity), the second front handle should first be transferred to the back , for which the body is rotated 180°, without doing traction, so that the back passes under the pubic symphysis (Fig. 4, b).
To release the rear handle, take the fetal legs at the ankle joint with one hand and lift them forward and to the side opposite the fetal back (Fig. 4, c). Two fingers (index and middle) of the corresponding hand are inserted into the vagina (along the back of the fetus, closer to the sacral cavity) and, sliding along the back, and then along the shoulder of the fetus, they reach the elbow bend. Then the obstetrician moves the handle with his fingers so that it slides over the face and chest of the fetus, i.e., makes a “washing” movement; First, the elbow appears from the vagina, and then the forearm and hand.
Then the front handle is brought out, having previously transferred it to the rear. There are other ways to release the handles. So, according to Muller, hands should be born on their own. In this case, it is recommended to pull the fetal body down until the anterior shoulder appears from under the pubic arch and then the corresponding handle fits under the pubic symphysis and comes out. After this, the torso is vigorously lifted upward until the rear shoulder emerges from under the perineum and the rear arm is born.
The third stage is the release of the head, the edges must pass through the birth canal in a state of flexion (small oblique size), which is achieved using various techniques. The best of them is the Morisot-Levret-Lachapelle method (Fig. 4, d), in which the hand that released the second handle is inserted into the genital tract. The fetal body is placed on the forearm. The nail phalanx of the index finger of the hand is inserted into the fetal mouth, on which the fetus is located. A finger inserted into the mouth does not act as a driving force, but only supports the flexion of the head. With the other (outer) hand, grab the fetal shoulder with the index and middle fingers bent in a hook-like manner. The inner hand supports the head in a state of flexion, which promotes correct rotation and transition of the head from the transverse size of the entrance to the pelvis to the oblique size of the pelvic cavity, and then to the direct size of the exit from the pelvis. Traction is applied with the outer hand. The direction of traction should coincide with the wire axis of the pelvis; when the head is at the entrance to the pelvis, the direction of traction goes backward (on the obstetrician’s socks), in the pelvic cavity - downwards (on the knees of the sitting obstetrician). When the suboccipital fossa approaches the lower edge of the pubic symphysis, the head is rotated around the fixation point anteriorly, and the chin, forehead and back of the head appear from the genital slit. When removing the head, the assistant applies gentle pressure from above through the abdominal wall.
Rice. 5. Schematic representation of some stages of extraction (extraction) of the fetus in various types of breech presentation: a - traction of the fetus by the leg in mixed breech presentation; b — traction of the fetus after eruption of the buttocks with a mixed breech presentation; c — extraction of the fetus by the inguinal fold in a purely breech presentation.
Removal (extraction) of the fetus by the pelvic end is usually performed using manual techniques. There are ways to extract the fetus by the pedicle(s) and by the inguinal fold. Indications for removing the fetus by the pelvic end are severe illnesses of the woman in labor requiring urgent termination of labor (heart defects, eclampsia, etc.), the onset of fetal hypoxia and the condition after the classic rotation on the leg (see Obstetric rotation). In the crust, the fetus is removed by the pelvic end either when the fetus is dead or in the absence of conditions for cesarean section. Extraction is performed under anesthesia provided that the cervix is fully dilated, the size of the fetal head and pelvis of the woman in labor corresponds, and the amniotic sac is opened. Removing the fetus in a mixed breech presentation consists of four steps: removing the fetus to the level of the navel, removing the fetus to the lower angle of the shoulder blades, releasing the arms, releasing the subsequent head. The leg lying in front is grabbed by hand. Traction is applied by the leg downward (posteriorly) and the leg is turned with the flexion side forward (Fig. 5, a), while the fetus is turned with its back anterior. When erupting the buttocks, the index finger of the same hand is inserted into the groin fold. The forward-facing ilium of the fetus represents the point of fixation. The obstetrician grabs the fetal anterior thigh with both hands, vigorously lifts it anteriorly, and the posterior gluteal region gradually rolls out over the perineum. There is no need to free the second (back) leg - it falls out on its own. After eruption of the buttocks, the obstetrician places the thumbs of both hands along the fetal sacrum (Fig. 5, b), covering his hips with the remaining fingers. Traction is done more horizontally (downwards), and the fetus is removed up to the navel. The fetus is removed to the lower angle of the shoulder blades, the arms and head are released, as when providing manual assistance.
Removing the fetus in a purely breech presentation presents significant difficulties, especially when driving the buttocks into the pelvis, which occurs when labor is weak or due to a discrepancy between the sizes of the fetus and the mother's pelvis. Therefore, if labor is weak, the fetus is large, or the fetus is not progressing, a caesarean section should be performed. When the buttocks are driven into the pelvis, an extremely unfavorable situation is created, since delivery through the birth canal becomes difficult and traumatic for the mother and fetus, and the time for delivery by cesarean section is lost. Extracting a fetus with the buttocks stuck in the pelvis is one of the most difficult operations in obstetrics. With a high standing and mobility of the buttocks, a purely breech presentation is transferred to an incomplete breech presentation by lowering the leg, and then the fetus begins to be removed.
The first step of the operation - removing the fetus from the inguinal fold to the umbilical ring - is performed with the index finger, which is inserted into the inguinal fold (Fig. 5, c). Traction is performed posteriorly with a hook-shaped curved finger during pushing. To enhance traction, it is recommended to clasp the hand performing the operation with the other hand in the wrist area. The anterior buttock is removed to the lower edge of the pubic symphysis, and the fetal ilium becomes the point of fixation. Then the finger of the second hand is inserted into the posterior inguinal fold and the posterior buttock is removed.
The obstetrician then places both thumbs along the fetal sacrum, wrapping the remaining fingers around the fetal hips, and removes the fetus up to the umbilical ring. The next three stages of extraction are carried out in the same way as with manual assistance. In case of fetal death in a purely breech presentation, extraction can be done at the inguinal fold using tools (hook, loop). The use of obstetric forceps to extract the fetus by the pelvic end is undesirable due to the high rate of complications.
How to help your baby roll over
While there are several weeks left before the birth, you can try to influence the situation and change the breech presentation to the cephalic one. Before following the recommendations given below, you should consult your doctor.
- Lie on your back so that your pelvis is elevated above your head. Lie in this position for 5-10 minutes twice a day. The exercise can be performed from 32 weeks of pregnancy until the baby turns over.
- Take the knee-elbow position and stand there for 15 minutes several times a day. Thanks to gravity, the fetal head should turn into the correct position.
- Talk to your baby and ask him to roll over. Many mothers note that this approach is very effective and really helps to achieve results. You can enhance the effect with the help of visualization - mentally imagine that the child has already turned over.
After 34 weeks, the obstetrician-gynecologist may suggest performing a manual inversion. The procedure is carried out under hardware supervision and is considered quite safe.