When to give
Not all infectious diseases are treated with antibiotics. Thus, the irritant of diphtheria, fungal diseases, tetanus and botulism in children are toxins. The basis of sinusitis and inflammatory diseases of the bronchial mucosa are viruses. Inflammation of the paranasal sinuses, ears and throat, accompanied by fever, is more often caused by exposure to bacteria. Antibiotics affect only very simple microbes and are useless for viral diseases, such as influenza, hepatitis, chickenpox, herpes, rubella, measles.
Likewise, if a child just starts to have a runny nose, a sore throat, or a fever, there is no need to immediately use antibiotics. Moreover, after a course of one of the drugs of a particular series, the body slowly develops resistance (resistance) of pathogens to this drug and weak sensitivity to the entire series. Due to this, prescribing antibiotics for ARVI in children is reasonable only if bacterial flora has joined the infection, and this usually happens no earlier than on the 3-4th day of the disease.
Antibiotics and lactation
Are antibiotics dangerous for a baby if a nursing mother takes them? It all depends on the type of drug. Penicillins, macrolites and cephalosporins are considered compatible with breastfeeding.
If treatment is carried out with their help, lactation can be continued. But these medications can cause side effects for both mother and baby, including:
- allergy
- dysbacteriosis
- diarrhea
- constipation and so on
To prevent them, mothers should take probiotics (Bifidumbacterin, Linex), as well as fermented milk products. In consultation with the doctor, products with beneficial bacteria can be given to the child.
Aminoglycosides, tetracycline, chloramphenicol, lincomycin, metronidazole, some fluoroquinolones and other drugs are prohibited during breastfeeding.
During lactation, treatment of any disease, even simple ARVI, should be carried out under the supervision of a doctor, so as not to harm the baby.
Names
Each group of antibiotics has its own mechanisms of influence on microbes and affects a specific group of bacteria. Therefore, before prescribing drugs, you need to take smears (bacterial culture tests) from the throat and nose to determine the sensitivity of the microflora to specific groups of antibiotics.
However, doctors do not always have such an opportunity, since the results of smears can only be expected 3-7 days after the test, and the child’s condition is already critical at the moment; in this case, broad-spectrum antibiotics are prescribed.
Penicillin group
This is the main category of antibiotics that are prescribed to children for respiratory diseases. Penicillins interfere with the synthesis of key substances that are part of the cell membrane tissues of harmful bacteria, thus causing their death.
- Amoxicillin is prescribed for bacterial diseases of the upper respiratory tract, ENT organs (tonsillitis, pharyngitis, otitis, etc.), genitourinary system (cystitis), gastric (peritonitis, enterocolitis), infectious infections of the skin and soft tissues. Can be prescribed to children over 2 years of age.
- Flemoxin Solutab is similar to a new generation of amoxicillin, which can be prescribed to children from 1 year of age. It is used to suppress harmful bacteria (staphylococci, streptococci), cure pneumonia, etc.
- Augmentin is a drug with a wide spectrum of action, prescribed to children from the very beginning of life (as drops). It has bacteriolytic (destructive) qualities regarding aerobic, anaerobic gram-positive and gram-negative strains. As stated in the instructions, it is harmful to patients with severely impaired liver and kidney function.
- Amoxiclav is a combined antibiotic for the treatment of sinusitis, acute abscesses, otitis media, bronchitis, infections of the genitourinary system , skin, bones, joints, and for prevention after surgical interventions. It is prescribed to children from the very beginning of life as a suspension.
Normalization of balance
How to help a baby who has dysbiosis? Treatment includes taking sorbents and preparations containing beneficial bacteria. There are various probiotics available today. One of them is “Bifidumbacterin”.
“” is a drug that contains active bifidobacteria, as well as substances necessary to maintain their vital functions. The main indication for taking the drug is dysbacteriosis.
"Bifidumbacterin" is produced in different forms. Children are usually prescribed powder. The dosage regimen for newborns is 1 sachet 2-3 times a day, for babies up to 1 year old – 1 sachet 3-4 times a day. The product must be diluted in milk and given during feeding.
Treatment is carried out for 2-3 weeks. During this period, beneficial bacteria should populate the intestines, displacing opportunistic microorganisms.
If probiotics do not have an effect, and the dysbiosis that accompanies diarrhea, constipation and flatulence does not go away, the child may be prescribed bacteriophages. Their formula includes viruses that do not harm beneficial flora, but only work against pathogenic microbes.
It is advisable to take probiotics in parallel with antibiotics.
How to take it correctly
To prevent taking antibiotics from causing damage to the child’s developing body, parents need to know several important rules for taking these drugs:
- The course of treatment with an antibiotic is at least 5 days, maximum 14 (in severe cases). Even if the child feels much better even on the 3rd day of treatment, just do not end the treatment for at least another 48 hours. If medications are taken incorrectly (an unauthorized dose reduction, non-compliance with the dosage regimen, or an incomplete course of treatment), only the weakest microbes die, although a temporary improvement in the general condition of the body is noted. The remaining bacteria mutate, adapt to the previously taken medicine and do not react to it at all. It is necessary to look for a replacement, increase the dose, or try an antibiotic from a completely different series.
- The antibiotic should be taken at the same time every day. If you need to take the medicine 2 times during the day, then you should do it exactly every 12 hours.
- If the drug is provided to small children as a suspension or drops, then the contents of the bottle are carefully stirred until the liquid becomes homogeneous and all the sediment has dissolved.
- Almost all antibiotics should be taken during meals or immediately after them, washed down with a considerable amount of water (not tea, compote, milk, juice or mineral water).
- To maintain a normal level of intestinal microflora and avoid the formation of dysbiosis in a child, bifidobacteria or lactobacilli should be taken at the same time (prescribed by a doctor).
- For a certain period of time while taking antibiotics, it is best to keep the child on a diet: remove fatty, fried, smoked foods, and sour fruits. The use of antibiotics in itself greatly inhibits liver function, and heavy meals significantly increase the load.
- Any antibacterial drugs are prescribed only by a doctor. The dosage is calculated based on the severity of the disease, the properties of the body and the general condition of the child.
- If there is no improvement within 48-72 hours after starting antibiotics, you should immediately consult a doctor to adjust the cure. The same actions are taken by parents if the child is allergic or exhibits other undesirable effects.
- You should always write down when, what medications, what course were taken before, and whether the children had any allergies or other undesirable effects.
How often can you give
The less often antibiotics are used to treat children, the better. Over time, resistance to any antibacterial drug develops in pathogens, which can complicate the cure of diseases for the rest of life. Another argument “against” is a decent load on the child’s growing body.
Some recommendations for parents on taking antibiotics:
- if the disease is not very serious, it is necessary to avoid the use of antibacterial drugs;
- if the child has never been given antibiotics, then therapy should begin with the weakest medicine, but the choice of the drug and its dosage is primarily made by the doctor;
- after treatment is completed, for some time the child must be given probiotics to restore normal microflora and absorbent drugs (Enterosgel or Polysorb) to remove toxins and decay products of harmful bacteria from the liver and body;
- for the next serious illness, the doctor will prescribe a stronger drug for the child;
- Nowadays, a lot of local antibacterial drugs have appeared (for example, Bioparox throat spray, Isofra, Polydex nasal drops, Sofradex, Garazon ear drops, Fluimucil-antibiotic IT for inhalation, etc.) which have a less noticeable effect on the child’s body .
Indications for the use of antibiotics in children
The use of antibiotics in children is justified only in cases of bacterial disease. However, viruses very often cause symptoms similar to a bacterial infection, which significantly complicates the choice of treatment tactics. The only thing that helps is laboratory diagnostics, which are not cheap these days. However, in this case, the gamble is worth the candle: it is better to make sure that the antibiotics will solve the problem and not be taken in vain. Unreasonable use of antibiotics risks the fact that when they are really needed, the body may react to them.
Relying on past experience or the advice of loved ones (they say that it helped your friend’s child and will help mine), you risk not saving, but harming. Therefore, when it comes to choosing antibiotics for children, the issue of parental responsibility and a professional approach to the issue is especially acute. Going to see a pediatrician and going through all the necessary diagnostic procedures is the main task of a parent. And the doctor decides whether the child needs an antibiotic, if so, which one and in what dosage, how much to take, etc. You should not suspect the doctor of unprofessionalism if he quickly decided on the diagnosis and prescribed the drug. Some antibiotics have a wide spectrum of action and have indeed proven themselves in medical practice.
Taking antibiotics is 100% justified when:
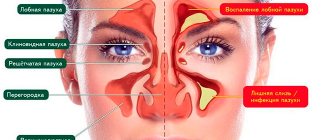
- acute purulent sinusitis (in children under 6 months)
- exacerbation of chronic sinusitis
- acute tonsillitis (streptococcal)
- acute otitis media (in children under 6 months)
- paratonsillitis
- epiglotite
- bacterial pneumonia (pneumonia)
Why are they dangerous?
- Children are not encouraged to take aminoglycoside antibiotics, which have a negative effect on the child’s auditory organs and renal system. These include Kanamycin and Gentamicin.
- Children under 8 years of age are prohibited from being prescribed antibiotics of the tetracycline group (doxycycline, tetracycline, minocycline). The latter can help thin the enamel of teeth, as well as slow down the growth of the bone skeleton.
- Taking chloramphenicol can lead to the formation of aplastic anemia in children.
- Fluorinated quinolones (pefloxacin, ofloxacin) also belong to the category of antibiotics prohibited for children; they disrupt the proper development of joint cartilage.
All of the listed groups of antibiotics are prescribed to children extremely rarely, when the disease cannot be treated with other drugs, and the benefits of taking an antibiotic outweigh the estimated risk.
Almost all antibiotics have a bad effect on the liver, are quite toxic, cause allergies and other undesirable effects (nausea, vomiting, dizziness, disruption of the gastrointestinal tract).
Indications for use
Antibiotics are prescribed to infants only to treat bacterial infections.
Main indications:
- respiratory and otolaryngological diseases - non-viral bronchitis, pneumonia, tonsillitis, otitis media, sinusitis, whooping cough, diphtheria and so on
- gastrointestinal pathologies – salmonellosis, dysentery
- dermatological problems – boils, erysipelas
- urological diseases - cystitis, pyelonephritis and so on
You should not give your child medicine simply because he has a stomach ache or diarrhea. Dr. Komarovsky draws the attention of parents to the fact that all decisions regarding antibiotic therapy for intestinal infection or bronchitis should be made by a doctor. His task is to choose the drug, the method of administration and the duration of administration.
The optimal way to select an antibiotic is to conduct a bacterial culture of sputum, urine or feces. It allows you to identify the culprit of the infection and its susceptibility to medications. But the analysis takes some time, which is why in many cases broad-spectrum antibiotics are prescribed, which act on most bacteria. Why are they dangerous?
Side effects may occur after taking these medications, including:
- dysbacteriosis
- allergy
- irritable bowel
- diarrhea
- decreased immunity
- constipation and so on
Some drugs affect not only the intestines: gentamicin has a bad effect on the kidneys, tetracycline has a bad effect on the liver, and chloramphenicol has a bad effect on hematopoiesis.
Possible negative consequences are not a reason to refuse medications. Bacterial diseases cannot be cured without them.
You can minimize side effects by strictly following your doctor’s instructions and taking probiotics (“”).
For infants, doctors try to prescribe the least toxic antibiotics in the form of solutions and suspensions; in rare cases, injection is practiced.
For babies
For infants, antibiotics are prescribed only in very severe cases. They are administered mainly orally (considered the most gentle way) as suspensions or drops. The finished mixture has a limited shelf life, so it is sold in pharmacies as a bottle with powder for diluting the suspension. After treatment is completed, the drug is not at all suitable for long-term storage. If there are reasons why the baby cannot take medications by mouth, he is prescribed injections.
Drugs approved for use in infants:
- Augmentin, Amoxiclav, Cefuroxime, Asketil, Ceftriaxone, Sumamed - from the very beginning of life;
- Ikzim, Zinnat, Pancef, Hemomycin - from 6 months;
- Flemoxin – from 1 year;
- Amoxicillin – from 2 years;
- Klacid - from 3 years old.
What types of medications can be used?
Note! Among several groups of antibiotics for the treatment of children, it is recommended to use the following types of drugs:
- Penicillins and protected penicillins. The first group includes the drugs flemoxin solutab, amoxicillin and amosin. These are the least toxic agents with a wide spectrum of action. But many pathogenic microorganisms can quickly develop resistance to such drugs. In such cases, an alternative can be protected penicillins, which are not destroyed by the protective mechanisms of bacteria (augmentin, flemoclav, amoxiclav).
- Macrolides . Antibiotics with hypoallergenic properties and minimal side effects. They act slowly, but are highly effective against pathogens such as legionella, mycoplasma, chlamydia, streptococci and staphlococci. These drugs include clarithromycin and sumamed.
- Cephalosporins . In pediatrics, fourth-generation antibiotics of this group are mainly used. They act faster than macrolides, but can cause serious side effects, although they are generally low-toxic. Among the antibiotics in this group are Suprax, Zinnat and Cephalexin.
- Nitrofurans (nifuratel, furazidin, nifuroxazide). The drugs have a wide spectrum of action and high efficiency.
- Fluoroquinolones . The most powerful drugs used in childhood. Their use is justified when antibiotics of other groups are ineffective or bacteria develop resistance to them. Fluoroquinolones include levofloxacin, moxifloxacin and drugs based on these antibiotics.
How to boost immunity after treatment
Taking antibiotics mainly contributes to the formation of intestinal dysbiosis in children, because practical bacteria living in the digestive tract are also affected. Due to this, simultaneous use of drugs that restore intestinal microflora is necessary. Probiotics are live cultures of bifidobacteria or lactobacilli that enrich and normalize the flora of the gastrointestinal tract, thus increasing the body's immunity.
Widely used probiotic preparations:
- Linex - restores the natural intestinal flora, eliminates diarrhea in a child after taking antibiotics. Can be prescribed from the very beginning of life.
- Bifiform - promotes the colonization of bacteria that produce lactic and acetic acid, which prevents the proliferation of harmful microorganisms. Approved for use in neonates.
- Bifidumbacterin - restores flora, improves the functioning of the gastrointestinal tract, and has immunomodulatory properties. Can be prescribed from the very beginning of life.
- Laktiv-ratiopharm - has bifidobacteria and lactobacilli, has a beneficial effect on the microflora and the entire body of the child. Prescribed for children from 2 years of age.
- Hilak - normalizes the pH balance of the stomach, suppresses the growth of pathogenic bacteria. Prescribed to children from birth.
Along with taking antibiotics, children with low immunity are advised to use drugs that increase the body's resistance to infectious and non-infectious infections and tissue restoration.
Key groups of immunomodulators:
- Interferon - prevents infections from affecting the body, increases defenses. Prescribed for children from 1 year of age.
- Immunoglobulin - has a lot of antibodies that successfully resist harmful microorganisms and viruses. Can be prescribed to children from the very beginning of life.
- Anaferon is a homeopathic immunomodulator that increases the level of antibodies in the body. Allowed for consumption from 6 months.
- Aflubin is a group homeopathic drug that has immunostimulating, antipyretic, and anti-inflammatory properties. Prescribed to children from birth.