Diabetes insipidus – what is it?
There is a small section in the brain - the hypothalamus, which is responsible for the homeostasis of the body. The hypothalamus regulates the production of vasopressin, an antidiuretic hormone (ADH) , which plays a key role in regulating the amount of fluid in the body. Vasopressin travels from the hypothalamus to the pituitary gland, from where it is released into the blood as needed. If there is insufficient vasopressin in the blood, water absorption is impaired, which causes polyuria (excessive urination).
Diabetes insipidus is diagnosed when the hormone vasopressin is produced inappropriately ( central diabetes insipidus ) or when the kidneys' response to antidiuretic hormone is reduced ( renal diabetes insipidus ). Also, diabetes insipidus can occur in women during pregnancy ( gestational diabetes insipidus ) or when the body does not perceive thirst correctly ( nervous or insipidal form of the disease ).
Not everyone has diabetes
Diabetes insipidus is different from diabetes mellitus - they are two completely different diseases. Despite the fact that some of their symptoms have a certain similarity (constant thirst, excessive urination), the mechanism of occurrence of these diseases is different.
Diabetes mellitus causes high blood glucose levels due to the body's inability to use blood glucose for energy. People with diabetes insipidus usually have normal sugar levels, but their kidneys cannot balance the amount of fluid in the body.
Diabetes insipidus tends to occur more often in men than in women.
Below are the differences between diabetes insipidus and diabetes mellitus and psychogenic polydipsia:
| Sign | Diabetes insipidus | Diabetes | Psychogenic polydipsia |
| Thirst | Very strong | Strong | Very strong |
| Amount of urine per day | 3-15 liters | up to 2-3 liters | 3-15 liters |
| Onset of the disease | Spicy | Gradual | Spicy |
| Nocturnal enuresis | Present | Present when blood sugar level is >13.5 mmol/L | Present |
| Increased blood glucose | No | Yes | No |
| Sugar in urine | No | Yes | No |
| Relative density of urine | Low, < 1.005 | High | Low, < 1.005 |
| The patient's condition during the test with dry food | Getting worse | Without changes | Without changes |
| The volume of urine excreted during the dry food test | Does not change | Does not change | Reduces to normal values |
| Blood uric acid level | >5 mmol/l | Increases with severe decompensation | <5 mmol/l |
Causes of the disease
- benign or low-quality (with the presence of metastases) tumors of the pituitary gland or hypothalamus;
- severe head contusion, traumatic brain injury;
- pathologies of the hypothalamic-pituitary system of the brain;
- family history of diabetes insipidus;
- brain surgery;
- impaired perception of the antidiuretic hormone vasopressin by the kidneys (primary tubulopathy).
As noted by I.I. Dedov in the textbook “Endocrinology”, every 5th case of diagnosed diabetes insipidus is caused by neurosurgical interventions.
General information
Diabetes insipidus
(“diabetes”) is a disease that develops when there is insufficient release of antidiuretic hormone (ADH) or a decrease in the sensitivity of the kidney tissue to its action. Violation of the secretion of ADH by the hypothalamus (absolute deficiency) or its physiological role with sufficient formation (relative deficiency) causes a decrease in the processes of reabsorption (reabsorption) of fluid in the renal tubules and its excretion in urine of low relative density. In diabetes insipidus, due to the release of a large volume of urine, unquenchable thirst and general dehydration of the body develop.
Diabetes insipidus is a rare endocrinopathy that develops regardless of the gender and age group of patients, most often in people 20-40 years old. In every 5th case, diabetes insipidus develops as a complication of neurosurgical intervention.
Diabetes insipidus in women
Diabetes insipidus is more common in women than in men. The disease is often confused with diabetes, but these are two different diseases. Diabetes insipidus is most often diagnosed in women under the age of 25 . The causes of the development of pathology are brain damage and trauma, as well as neoplasms. Sometimes the disease develops against the background of hormonal changes during pregnancy. In the worst case, this can cause a miscarriage. Signs of the disease in women:
- headaches;
- irritability;
- menstrual irregularities;
- disturbances in blood pressure;
- increased urination;
- urinary incontinence (especially at night);
- unquenchable thirst.
The pathology is difficult for women over 30 years of age. Against the background of the disease, other disorders develop that affect further ability to conceive and can lead to infertility.
Diabetes insipidus in men
In men, the pathology does not occur as often as in women. The main feature is frequent urination both at night and during the day. Increased thirst (more than 5 liters per day) is also a cause for concern. Men over the age of 40 or during menopause are most susceptible to negative effects The symptoms of the disease in men are similar to urological diseases, so at the first signs you should consult a doctor for a diagnosis.
Changes in the sexual sphere, accompanied by an increased feeling of thirst or urination, signal the development of diabetes insipidus. Neglected treatment can provoke other abnormalities in the reproductive system in men and lead to impotence and infertility. In adolescents and young men, diabetes insipidus causes sexual infantilism.
Diabetes insipidus in children
In children, the disease occurs from birth. However, full diagnosis and confirmation of the diagnosis is made upon reaching 3 years of age. In childhood, the disease is difficult to diagnose, as it occurs in completely different ways and has different symptoms. Signs of the disease in children:
- nausea;
- vomit;
- rapid breathing (hyperpnea);
- increased excitability;
- decreased appetite;
- constipation;
- change in body temperature.
In rare cases, the disease may resolve in the absence of an increased feeling of thirst. Sometimes the disease is completely asymptomatic. Therefore, pathology can only be detected with the help of special studies and analyses. Diabetes insipidus can cause the development of psychosomatic or nervous disorders in children. In advanced cases, the disease leads to coma and death. Treatment is carried out through hormone replacement therapy.
Symptoms
We note that the disease develops suddenly. First, unbearable thirst appears, then excessive urination begins to bother you: about 20 liters of urine can come out per day.
Unpleasant symptoms begin to bother children during the day and at night, because of them he wakes up, cannot sleep, and constantly drinks water. Urine is clear and light. Due to constant lack of sleep, a person quickly gets tired, he becomes emotionally unbalanced, irritable, and his sweating decreases, while his skin is too dry.
In severe cases, the following unpleasant symptoms occur:
- Lost appetite.
- Dyskinesia is observed in the biliary tract.
- I am worried about pain under the right rib.
- Nausea, heartburn, vomiting, and belching occur.
- A bitter taste appears in the mouth.
- The functioning of the intestines is disrupted - cramping pain in the abdomen, bloating, and irregular bowel movements.
If the patient begins to limit fluid intake, his condition begins to deteriorate sharply: dry mouth appears, headache bothers him, and heart rate increases.
Dangerous! It is urgent to take action when blood pressure rarely drops, blood begins to thicken, temperature rises, and dehydration occurs.
In women, due to diabetes insipidus, the menstrual cycle is disrupted, and amenorrhea, which is associated with infertility, may subsequently develop. If pregnancy occurs, it can end in spontaneous abortion.
Symptoms in children are pronounced. The disease is especially dangerous for newborns. Their temperature rises sharply, nausea and vomiting bother them, and the functioning of the nervous system is disrupted.
Older children may experience enuresis, urinary incontinence, and also:
- Severe headache.
- Unpleasant sensations in the chest, as well as in the chest due to bronchial cancer.
- Vision is impaired when the tumor begins to put pressure on visual function.
- Body temperature rises if the brain becomes inflamed.
Types of diabetes insipidus
Diabetes insipidus can occur in various forms, depending on the etiology. The following types of diabetes insipidus are distinguished:
- central (neurogenic);
- nephrogenic (renal);
- gestational (diabetes insipidus in pregnant women);
- insipidary (dipsogenic, nervous).
Central (neurogenic) diabetes insipidus
Central diabetes insipidus occurs when the hypothalamus or pituitary gland in the brain malfunctions, resulting in disruption of the normal production, storage, and release of the antidiuretic hormone vasopressin . Vasopressin causes the kidneys to remove too much fluid from the body, leading to increased urination (polyuria).
The following reasons can lead to dysfunction of the hypothalamus or pituitary gland:
- brain surgery;
- acute or chronic infectious diseases: sore throat, influenza, sexually transmitted diseases, tuberculosis;
- inflammatory diseases of the brain;
- vascular lesions of the hypothalamic-pituitary system in the arteries of the brain, which lead to impaired circulation of the vessels supplying the pituitary gland and hypothalamus;
- tumor processes in the pituitary gland and hypothalamus, cysts (benign tumors);
- traumatic brain injuries, concussions;
- inflammatory, degenerative kidney damage that prevents them from accepting vasopressin.
Central diabetes insipidus can also result from an inherited defect in the gene that produces vasopressin, although this cause is extremely rare. In some cases, the cause of neurogenic diabetes insipidus remains unknown.
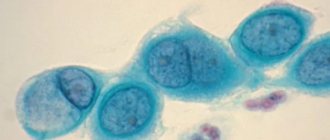
Nephrogenic (renal) diabetes insipidus
Renal diabetes insipidus occurs when the kidneys stop responding to vasopressin and continue removing too much fluid from the body. Renal diabetes insipidus can result from inherited gene changes or mutations that cause the kidney nephron cells to fail to sense vasopressin.
Other causes of the renal form of the disease:
- sickle cell anemia is a rare disease;
- congenital heredity;
- damage to the renal medulla or nephron urinary tubules;
- chronic kidney disease - polycystic disease (multiple cysts) or amyloidosis (deposition of amyloid tissue) of the kidneys; chronic renal failure;
- some drugs that are toxic to kidney tissue (nephrotoxic drugs, these include: lithium, amphotericin B, gentamicin, tobramycin, amikacin and netilmicin, cyclosporine);
- low potassium levels in the blood;
- high levels of calcium in the blood;
- blockage of the urinary tract.
The causes of nephrogenic diabetes insipidus may in some cases be unknown.
Insipidary (nervous) diabetes insipidus
A defect in the perception of the thirst mechanism , for which the hypothalamus is responsible, causes the dipsogenic (incipidary) form of the disease. This defect results in an abnormal increase in thirst and fluid intake, which suppresses vasopressin secretion and increases urine output.
The same events and conditions that damage the hypothalamus or pituitary gland - surgery, infections, inflammation, tumors, head injuries - can also damage the thirst mechanism. Certain medications or mental health problems may predispose a person to developing dipsogenic diabetes insipidus (polydipsia nervosa).
Gestational diabetes insipidus in pregnant women
Gestational diabetes insipidus occurs in women during pregnancy . In some cases, the placenta, the temporary organ that connects mother and baby, causes the mother to have insufficient vasopressin levels . In other cases, pregnant women produce more prostaglandins, physiologically active substances that reduce the sensitivity of the kidneys to vasopressin.
In most pregnant women, gestational diabetes insipidus is mild and does not cause noticeable symptoms. Gestational diabetes insipidus usually goes away after the baby is born, but it can return with another pregnancy.
Symptoms of diabetes insipidus
Typical manifestations of diabetes insipidus are polyuria and polydipsia. Polyuria is manifested by an increase in the volume of daily urine excreted (usually up to 4-10 l, sometimes up to 20-30 l). Urine is colorless, with a small amount of salts and other elements and a low specific gravity (1000-1003) in all portions. The feeling of unquenchable thirst in diabetes insipidus leads to polydipsia - the consumption of large amounts of fluid, sometimes equal to that lost in urine. The severity of diabetes insipidus is determined by the degree of antidiuretic hormone deficiency.
Idiopathic diabetes insipidus usually develops acutely, suddenly, and less often - gradually increasing. Pregnancy can trigger the manifestation of the disease. Frequent urge to urinate (pollakiuria) leads to sleep disturbances, neuroses, increased fatigue, and emotional imbalance. In children, the early manifestation of diabetes insipidus is enuresis, later delayed growth and puberty occur.
Late manifestations of diabetes insipidus are dilation of the renal pelvis, ureters, and bladder. As a result of water overload, overdistension and prolapse of the stomach occurs, biliary dyskinesia and chronic intestinal irritation develop.
The skin of patients with diabetes insipidus is dry, the secretion of sweat, saliva and appetite are reduced. Later, dehydration, weight loss, vomiting, headache, and decreased blood pressure occur. With diabetes insipidus, caused by damage to parts of the brain, neurological disorders and symptoms of pituitary insufficiency (panhypopituitarism) develop. Men develop weakened potency, women develop menstrual dysfunction.
Complications of diabetes insipidus
The greatest danger in diabetes insipidus is dehydration, which causes the loss of a large amount of fluid excreted along with urine due to frequent urination. Also, as a result of dehydration, the patient develops diseases such as: tachycardia, general weakness, possible vomiting and disturbances in mental and emotional state. Complications may include blood thickening, neurological disorders, and hypotension, which can be life-threatening. However, even with severe dehydration, the patient continues to have a high level of fluid excretion from the body. Women may experience menstrual irregularities, and men may experience decreased libido. Also, due to frequent intake of liquids, sometimes quite cold, respiratory tract diseases may develop.
Treatment
To successfully treat diabetes insipidus, the first thing you need to do is determine what its cause is. In the case of a brain tumor, kidney problems or the idiopathic nature of the disease, the treatment will be radically different.
Typically, therapy is carried out with drugs prescribed by the attending physician. They contain a synthetic analogue of an insufficiently produced hormone. Different medications may have different durations of action. Some need to be taken several times a day, others are taken once every 2-3 days.
For diabetes insipidus and the central form, drugs such as Carbamazepine or Chlorpropamide are usually prescribed, which stimulate suppressed hormonal production.
Drinking fluids in the classical way is ineffective in the case of such diabetes, so during treatment, droppers with nutritious saline solutions are used.
Treatment of women should involve a gynecologist, whose task is to correct the menstrual cycle at the hormonal level, avoiding long delays.
Complications
The main complication of diabetes insipidus is related to dehydration and its symptoms. Strong thirst constantly reminds you of this, but it is almost impossible to fully replenish fluid reserves. Severe dehydration cannot be treated with a drip.
A critical lack of fluid in the body can be recognized by the following signs:
If diabetes insipidus is not treated promptly, dehydration can lead to coma and death.
How is the diagnosis made?
Examination for diabetes insipidus includes laboratory diagnostics and special tests.
Doctors are faced with the question of the causes of increased urine production (polyuria) and dehydration in the patient. A differential diagnosis is made between central or renal diabetes insipidus and unnaturally strong thirst (polydipsia).
At the first stage, in patients with polyuria and polydipsia, the presence of hypotonic diuresis (low-density urine) is confirmed. To do this, evaluate the volume of urine per day, its relative density and osmolality.
Diabetes insipidus is characterized by:
- urine volume more than 40 ml per kg of body weight per day;
- relative density of urine less than 1005 g/l;
- urine osmolality is less than 300 mOsm/kg.
Next, exclude the main causes of nephrogenic diabetes insipidus (hyperglycemia, hypercalcemia, hypokalemia, hyperkalemia, renal failure, urinary tract infection).
Next, the patient undergoes tests:
- dry eating test;
- desmopressin test.
In patients with true diabetes insipidus, lack of fluid intake leads to rapid dehydration and weight loss. In this case, the central form of the disease is easily corrected with desmopressin.
The pathology diagnosis is completed by searching for the causes of symptomatic diabetes insipidus. At this stage, brain tumors are identified (using MRI), genetic defects, etc.
Diagnostics
To diagnose diabetes insipidus, special tests are performed, as well as laboratory and differential studies. Special tests include a test for polyuria - collecting a daily volume of urine. If it exceeds a volume of three liters, diabetes insipidus is diagnosed.
Another test requires the patient to abstain from liquids for eight hours. If polyuria persists during abstinence, weight decreases sharply and the person’s condition worsens, we are also talking about diabetes insipidus.
A blood test for C-peptide is also required to rule out diabetes, as well as a urine test for sugar and specific gravity. An ultrasound of the kidneys and bladder is performed; if there are complaints of complications, an ultrasound of the stomach may be prescribed.
To exclude neoplasms as the causes of the disease, an MRI of the brain and a functional study of the pituitary-hypothalamic region are performed.
Causes
The disease develops as a result of such factors:
- For infectious and viral diseases.
- For brain tumors – craniopharyngioma, meningioma.
- For breast cancer.
- In case of skull injury.
- In case of concussion.
- With genetic predisposition.
When vasopressin is produced in insufficient quantities, water is poorly removed from the body, subsequently the thirst center is irritated, osmotic blood pressure increases, and polydipsia develops.
Treatment for diabetes insipidus
The choice of tactics in the treatment of diabetes insipidus depends on the form of the disease. To treat the central form due to damage to the hypothalamus or pituitary gland, a synthetically produced vasopressin analogue is used.
The drug based on desmopressin is available in the form of tablets or nasal spray. Trade names: Vazomirin, Minirin, Presaynex and Nativa. It promotes the reabsorption of water in the kidneys. Therefore, when using it, you should drink only when you feel thirsty, so as not to cause water intoxication.
If you overdose on desmopressin or consume large amounts of liquid while using it, the following may occur:
- Increased blood pressure.
- Development of tissue edema.
- Decreased sodium concentration in the blood.
- Impaired consciousness.
The dose is selected individually from 10 to 40 mcg per day. It can be taken once or divided into two doses. Usually the drug is well tolerated, but side effects are possible in the form of headache and dizziness, pain in the intestines, nausea and a moderate increase in blood pressure.
When using desmopressin spray or drops, you need to remember that when you have a runny nose due to swelling of the mucous membrane, the absorption of the drug slows down, so in such cases it can be dripped under the tongue.
In the central form of diabetes insipidus, drugs based on carbamazepine (Finlepsin, Zeptol) and chloropropamide are also used to stimulate the production of vasopressin.
Nephrogenic diabetes insipidus is associated with the inability of the kidneys to respond to vasopressin, which may be in sufficient quantities in the blood. However, when testing with desmopressin, a reaction does not appear.
To treat this form, thiazide diuretics and non-steroidal anti-inflammatory drugs are used - Indomethacin, Nimesulide, Voltaren. The amount of salt in the diet is limited.
Gestational diabetes insipidus is treated with desmopressin drugs; treatment is carried out only during pregnancy; after childbirth there is no need for such therapy.
For mild or partial diabetes insipidus, non-drug therapy can be used in the form of adequate drinking regimen to prevent dehydration.
Dietary nutrition for diabetes insipidus is prescribed to reduce the load on the kidneys. Its main principles:
- Limiting protein, especially meat.
- Sufficient amount of fat and carbohydrates.
- Frequent small meals.
- Inclusion of fresh vegetables and fruits.
- To quench your thirst, use fruit drinks, juices or compotes.
The effectiveness of treatment is assessed by the well-being of patients and a decrease in the amount of urine excreted.
With full compensation, the symptoms of diabetes insipidus disappear. Subcompensated diabetes insipidus is accompanied by moderate thirst and increased urination. In the decompensated course, the symptoms do not change under the influence of therapy.
Renal diabetes insipidus is the most difficult to treat in children; it often develops severe renal failure, requiring hemodialysis and kidney transplantation. The idiopathic form of diabetes insipidus is rarely life-threatening, but cases of complete recovery are rare.
In the central form of diabetes insipidus, competent replacement therapy allows patients to maintain working capacity and social activity. Gestational diabetes, as well as drug-induced diabetes and cases of the disease in children in the first year of life usually end in recovery. The video in this article raises the topic of diabetes insipidus.
Drug treatment
The most common drug for the treatment of diabetes insipidus is Desmopressin , which is injected into the nasal passages. A prolonged preparation in the form of an oil solution of pituitrin is also prescribed . To eliminate the symptoms of neurogenic diabetes insipidus, Carbamazepine and Chlorpropamide are prescribed . These drugs stimulate the production of antidiuretic hormone.
Minirin tablets are used as a replacement for vasopressin . The dosage and course of treatment are prescribed by the attending physician depending on the degree of deficiency of antidiuretic hormone or its complete absence. Treatment with the drug begins with a small dose, which is increased if necessary. Various phosphodiesterase-5 inhibitors .
To treat nephrogenic diabetes insipidus with medications, medications are prescribed that reduce the volume of urine excreted. These include:
- thiazide diuretics - Triampur, Hydrochlorothiazide, Clopamide, Indapamide, Chlorthalidone . The drugs interfere with the reabsorption of chlorine in the urinary tubules of the nephron. As a result, the concentration of sodium in the blood decreases slightly, and fluid reabsorption increases;
- anti-inflammatory drugs - Etodolac, Diflunisal, Clofeson, Aspirin, Sulindac, Indomethacin . The drugs help reduce the flow of certain substances into the urinary tubules of the nephron. As a result, urine volume decreases and its osmolarity increases.
Adiurecrin
Medicine presented as a dry preparation of animal origin. The product acts within a quarter of an hour from the moment it enters the body. The duration of the effect is up to 8 hours. Adiurecrine is administered by inhaling the powder. Prescribed for children over 3 years of age.
There is also Adiurecrin in ointment form. This is more convenient for use, since introducing the ointment into the nasal cavity allows the drug to be evenly absorbed through the mucous membrane. In addition, the powder may get into the eyes if inhaled, which is typical for pediatric patients, but precludes the use of ointment.
In order to administer the required amount of the drug, a special tip with a piston is put on the tube. This allows you to strictly dose the drug. Adiurecrin is not used for pathology of the paranasal sinuses and respiratory tract disease. In most cases, it is prescribed for life.
Adiuretin SD
This is a vasopressin-like drug, available in the form of drops and solution for injection. Adiuretin SD is used to combat diabetes insipidus in the form of slow intravenous drip injections. The drug is used for treatment if intranasal administration is not possible.
Drops may also be prescribed. The endocrinologist, as a rule, prescribes 1-3 drops several times a day. Contraindications are chronic heart failure, polydipsia due to mental disorders and individual hypersensitivity to the components of the drug.
Minirin
Medicine in the form of spray and tablets. Used in the fight against central diabetes insipidus. Contraindications for use are psychogenic polydipsia, heart failure, decreased sodium levels in the blood, and renal failure.
Minirin is a desmopressin-based drug used in replacement therapy
Important! It should be used with caution to treat women during pregnancy and breastfeeding, as well as infants.
Diet and nutrition
The main goal of diet therapy is to reduce urination, and in addition, to replenish the body with vitamins and minerals that they “lose” due to frequent urge to go to the toilet.
It is worth giving preference to cooking in these particular ways:
- boil;
- steamed;
- stew food in a saucepan with olive oil and water;
- bake in the oven, preferably in a sleeve, to preserve all the beneficial substances;
- in a slow cooker, except for the “fry” mode.
When a person has diabetes insipidus, the diet should exclude those categories of foods that increase thirst, for example, sweets, fried foods, spices and seasonings, and alcohol.
The diet is based on the following principles:
- reduce the amount of protein consumed, leaving the norm of carbohydrates and fats;
- reduce salt concentration by reducing its consumption to 5 g per day;
- food should consist mainly of vegetables and fruits;
- to quench your thirst, use natural juices, fruit drinks and compotes;
- eat only lean meat;
- include fish and seafood, egg yolks in the diet;
- take fish oil and phosphorus;
- eat small meals often.
Sample menu for the day:
- first breakfast – omelet (steamed) of 1.5 eggs, vinaigrette (with vegetable oil), tea with lemon;
- second breakfast – baked apples, jelly;
- lunch - vegetable soup, boiled meat, stewed beets, lemon drink;
- afternoon snack – rosehip decoction, jam;
- dinner - boiled fish, boiled potatoes, sour cream, tea with lemon.
Drinking plenty of fluids is necessary - after all, the body loses a lot of water during dehydration and needs to be compensated.
Folk remedies
To improve sleep and reduce irritability, sedatives are used:
- Take equal parts of crushed valerian roots, fennel and caraway fruits, motherwort herbs and mix everything thoroughly. Then, from the resulting mixture, take two tablespoons of the raw material and pour 400 ml of boiling water, let it brew until cool and decant. Take half a glass if you feel irritable or nervous.
- Take equal parts of crushed valerian roots, hop cones, motherwort herbs, rose hips, mint leaves and mix everything thoroughly. From the resulting mixture, take one tablespoon of raw material and pour a glass of boiling water. Let it sit for an hour and then express. Take 1/3 glass at night for insomnia or increased nervous agitation.
To reduce thirst:
- Take 60 grams of crushed burdock root, place it in a thermos and pour one liter of boiling water. Leave it overnight and express in the morning. Take two-thirds of a glass three times a day.
- Take 20 grams of elderberry flowers, pour a glass of boiling water and leave for an hour. Then strain and add honey to taste. Take one glass three times a day.
- Take 5 grams (one teaspoon) of crushed young walnut leaves and pour a glass of boiling water. Let it brew and take it like tea.
Collection No. 1
Mix the following ingredients in the indicated parts:
- oily root (1);
- valerian root (1);
- pharmaceutical dill (2);
- azure bluegrass (2);
- Veronica grass (4);
- thyme herb (4);
- whitecap grass (4).
Take a tablespoon and pour 0.5 liters of boiling water. The resulting amount of infusion should be drunk over the next day. The course of treatment is 60-90 days.
Herbal medicine is an element of the treatment of diabetes insipidus
Collection No. 2
Combine medicinal plants in the indicated parts:
- dried marsh flower (2);
- fireweed flowers (2);
- marigold flowers (2);
- lilac buds (1);
- water trefoil (1);
- hop cones (1);
- wormwood grass (1).
The preparation method is similar to the first collection.
Collection No. 3
A collection of two medicinal plants will help relieve dry mouth and pathological thirst: spur grass and sandy cumin inflorescence. They must be combined in equal quantities. A tablespoon of the mixture should be poured with a glass of boiling water. This is done in the evening. In the morning, filter the infusion and take 100 ml between meals.
Burdock
Burdock, or rather its infusion, will help reduce the manifestations of pathological thirst. To prepare the remedy you need 4 tbsp. l. pour crushed raw materials with a liter of boiling water. It is advisable to brew the plant in the evening so that by morning the infusion is ready for use. After straining, take half a glass three times a day.
Elder
Folk remedies for diabetes insipidus include the use of elderflower infusion. You should take 2 tbsp. l. and pour 300 ml of boiling water. After 45 minutes the product is ready for use. To improve the taste, you can add linden honey. Take three times a day.
Walnut
An infusion of the leaves will help relieve pathological polydipsia. It is better to use young leaves. After the grinding process, 1 tsp. the substance should be poured into a glass of boiling water. In just 20 minutes the medicine will be ready.
Physical exercise
For diabetes insipidus, any physical activity is not recommended. But during the rehabilitation period, physical therapy will not hurt. A set of exercises for diabetes insipidus is aimed at activating and normalizing carbohydrate, protein and fat metabolism.
When engaging in physical therapy, you must carefully monitor your well-being and, at the first signs of deterioration, stop exercising or simply reduce the load. Classes should be carried out in a ventilated room or even in the open air. You need to breathe through your nose and your breathing should be rhythmic and free. Physical exercises must be alternated for different muscle groups and performed with moderate amplitude in the joints.
Treatment methods
First of all, it is necessary to get rid of the cause of the disease - infection, tumor, or cure brain injury. Diabetes insipidus is treated with replacement therapy. In this case, drugs with vasopressin are used, for example, Desmopressin (it can be bought in tablet form, drops in the nose). It is convenient to use Minirin in tablets. Many doctors recommend taking hormones in tablets, this way you can calculate the exact dosage and prevent the development of hyponatremia.
Drops that lead to changes in the nasal mucosa are dangerous. Additionally, it is necessary to use water-salt solutions to restore electrolyte balance. Preparations containing lithium carbonate have a positive effect on the body.
As for prognosis, if you complete a course of replacement therapy in a timely manner, there is no threat to a person’s life. It is only important to remember that with such treatment it is impossible to cure the disease. You can get rid of diabetes insipidus after the underlying cause is eliminated.
Nutrition is of no small importance. It is recommended to eat lean meats and eggs. In addition, you should give up protein for a while, otherwise the load on the kidneys will increase. But vegetable oil, butter, carbohydrates should be on your menu.
Thus, diabetes insipidus is a rather dangerous disease that cannot be ignored. It is very important to be promptly examined by a doctor and undergo a course of therapy to find out why the disease occurred, as well as how to treat it. You shouldn’t let the pathology start, otherwise everything could end in serious consequences.
What's the forecast?
The prognosis of diabetes insipidus mainly depends on what form is diagnosed in the patient. The majority of patients with diabetes insipidus have a favorable prognosis for life, but not for recovery. Diabetes insipidus does not affect performance or life expectancy, but can significantly reduce its quality.
With severe diabetes insipidus, most patients are assigned disability group 3. If diabetes insipidus is symptomatic, then when the cause is eliminated, recovery occurs. If the disease was caused by an injury, then after treatment it is possible to restore the functions of the pituitary gland. If diabetes insipidus is not treated, dehydration will cause the development of stupor and subsequent coma.
Types of disease
Diabetes insipidus has two main types.
- The first type is associated with pathologies of the head or hypothalamus. It is called central
m. It develops due to a violation of the excretion or formation of vasopressin. The first type is symptomatic and idiopathic. Symptomatic may appear due to diseases of the body due to various reasons (concussion, encephalitis). Idiopathic develops as a result of heredity. - The second type is called renal
. It appears due to a decrease in the sensitivity of kidney tissue to the effects of the same vasopressin. This type of diabetes is much less common than the first. Renal diabetes can develop as a result of damage to kidney cells by drugs or if there is a congenital predisposition.
Definition of diabetes insipidus
Prevention
There are no specific preventive measures for diabetes insipidus. It is recommended to consult a doctor in a timely manner, follow all recommendations and independently monitor your health to prevent complications from occurring.
Sources:
- https://diagid.ru/92-nesaharnyy-diabet-simptomy-lechenie-diagnostika-osobennosti-protekaniya-u-zhenschin-i-detey.html
- https://www.KrasotaiMedicina.ru/diseases/zabolevanija_endocrinology/diabetes-insipidus
- https://diabety-net.ru/diabet/nesaharnyj-diabet-prichiny-i-simptomy-lechenie-u-zhenshhin-i-muzhchin/
- https://www.medcentrservis.ru/disease/nesaharnyj-diabet/
- https://MenQuestions.ru/endokrinologiya/diabet/nesaharnyy-diabet.html
- https://GormonOff.com/zabolevanija/diabet/priznaki-nesaxarnogo-diabeta-u-muzhchin
- https://diabetik.guru/info/nesaharnyj-diabet-simptomy-u-muzhchin.html
- https://gormoon.ru/nesaharnyj-diabet-chto-eto-takoe-prichiny-simptomy-diagnostika-i-lechenie/
- https://sosudy.info/lechenie-nesaharnogo-diabeta
- https://doctor-365.net/nesaharnyj-diabet/