Release form and composition
The drug Bonviva is available in the dosage form of film-coated tablets. The tablets are packaged in blister packs of 14 pieces, a cardboard box contains 2 blisters (28 tablets) and instructions for use of the drug.
One tablet contains the active ingredient ibandronic acid in an amount of 150 mg. It also contains excipients, which include:
- Stearic acid.
- Colloidal anhydrous silicon dioxide.
- Tatan dioxide.
- Lactose monohydrate.
- Microcrystalline cellulose.
- Povidone K 25.
- Crospovidone.
- Hypromellose.
- Macrogol 6000.
- Talc.
Bonviva - instructions for use, reviews, analogues, price
Bonviva refers to medicinal medications used in the treatment of bone tissue pathologies - for example, as a preventive measure for postmenopausal osteoporosis in women, as well as to prevent fractures. The effectiveness of the drug has been proven by clinical studies. The medicine has a prescription from pharmacies.
Composition and release forms
The active ingredient of the drug is, as well as additional components, depending on the dosage form. Today, there are 3 types of medication - tablets with high or low concentrations of the active substance, as well as a solution for intravenous injection. They include:
- Tablets with a concentration of 2.5 mg of ibandronic acid. Excipients include colloidal silica (anhydrous), crospovidone, lactose monohydrate and microcellulose. The coating composition includes macrogol 6000, methyloxypropylcellulose, talc and E171 (titanium dioxide).
- Tablets with a concentration of 150 mg of the active ingredient. Additional elements in the composition are similar to low concentration tablets.
- A syringe with a ready-made solution of 3 mg sodium ibandronate. The solution also contains distilled water, anhydrous acetic acid, sodium acetate trihydrate and sodium chloride.
- Tablets with a concentration of 2.5 mg of ibandronic acid. Excipients include colloidal silica (anhydrous), crospovidone, lactose monohydrate and microcellulose. The coating composition includes macrogol 6000, methyloxypropylcellulose, talc and E171 (titanium dioxide).
- Tablets with a concentration of 150 mg of the active ingredient. Additional elements in the composition are similar to low concentration tablets.
- A syringe with a ready-made solution of 3 mg sodium ibandronate. The solution also contains distilled water, anhydrous acetic acid, sodium acetate trihydrate and sodium chloride.
The tablet form has an oval, white-cream color.
Tablets with a concentration of 2.5 mg of the substance are engraved with the inscriptions “IT” and “L 3” on both sides; their quantity per package is 28 pieces (2 blisters of 14 pieces each).
High concentration tablets have “150” on one side and “BNVA” on the other; This form is produced in the amount of one or three tablets per package.
The injection solution is a colorless transparent liquid, which is located in a special 3 ml syringe. In addition to the syringe, the cardboard package contains a sterile needle. Injections are released only in a syringe; There are no ampoules or similar forms of this drug available.
All dosage forms must be stored out of the reach of children and protected from direct sunlight. The shelf life of tablets with low and high concentrations of the substance is 4 and 3 years, respectively; the injection solution can be stored for no more than 2 years.
Distribution in the body
Clinical studies have not documented a direct relationship between the concentration of sodium ibandronate in the blood and an improvement in the therapeutic effect of the drug. The tablet form is highly absorbable in the body (mainly in the upper part of the small intestine). Concentrations in the blood are dose-dependent with a single dose of 50 mg and above.
The maximum concentration of the substance is observed 30-120 minutes after oral administration with a median of 60 minutes. Bioavailability values are 0.6%. Eating food and any drinks, with the exception of water, impairs the absorption of the substance and its availability by 90%.
Eating an hour before taking the drug does not affect the effectiveness of ibandronic acid, while eating an hour after taking the medicine negatively affects certain therapeutic effects (in particular, the drug has virtually no increase in bone mineral density).
Absorption and excretion
Once in the bloodstream, the active component either binds to bone tissue or is excreted from the body along with urine. Almost half (45% to 50%) of the substance penetrates the bones and accumulates. The apparent final volume of distribution is approximately 90 liters. The values of binding to plasma proteins when administered intravenously are 87%, when taking the tablet form - 85%.
According to clinical studies, the active substance is not metabolized (there is currently no information refuting this position).
Ibandronic acid does not inhibit the liver isoenzyme cytochrome P450, as well as other enzymes. Half of the active substance that remains unbound is excreted unchanged through the kidneys.
The half-life values depend on the dosage form of the drug:
- for 2.5 mg tablets it ranges from 10 to 60 hours.
- for 150 mg tablets - from 10 to 72 hours.
- for solutions this figure is also in the region of 10 - 72 hours.
The concentration of the drug decreases to 10% after 8 hours (for oral medications) or after 3 hours for injections. The total clearance of sodium ibandronate ranges from 84−160 ml/min.
Special patient groups
Clinical studies have not revealed a relationship between the effectiveness of the drug and age.
The only limitation for older people when taking Bonviva is concomitant pathologies (including liver or kidney).
Also, no clinically significant difference in pharmacokinetic parameters was identified in individuals of different genders and ethnicities; the exception is the Negroid race due to insufficient data.
Studies were conducted on a group of volunteers with liver failure or liver dysfunction. Since the drug practically does not involve the liver (there is no metabolism, and the kidneys play the main role in removing the substance from the body), no dose adjustment is required for patients in this group.
In the presence of renal failure (with mild or moderate severity of the disease - creatine clearance indicators are more than 30 ml/min), dosage adjustment is not required. In severe renal damage, an increased concentration of ibandronic acid in the blood is observed, while the clearance of the active substance decreased to 44 ml/min.
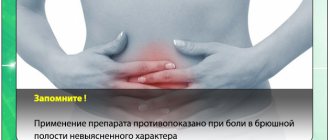
Main contraindications
Individual intolerance and hypersensitivity to any of the components of the drug is grounds for its discontinuation. Also, use is contraindicated in patients under 18 years of age, since the clinical safety of the drug has not been established for this age group. This should also include pregnancy and lactation, as well as the following pathologies:
- Hypocalcemia. Serum calcium levels should be increased before initiating bisphosphonate therapy.
- Severe renal failure (with creatine clearance levels
Source: https://Artroz.guru/bonviva.html
Pharmacological effect
Ibandronic acid is a highly active nitrogen-containing bisphosphonate, an inhibitor of bone resorption and osteoclast activity. Ibandronic acid prevents the development of bone destruction caused by blockade of gonadal function, retinoids, tumors and tumor extracts in vivo. Does not interfere with bone mineralization when administered in doses 5000 times higher than those used for treatment of osteoporosis. Does not affect the process of replenishment of the osteoclast pool. The selective effect of ibandronic acid on bone tissue is due to its high affinity for hydroxyapatite, which constitutes the mineral matrix of bone.
Ibandronic acid inhibits bone resorption in a dose-dependent manner and does not have a direct effect on bone formation. In women during menopause, it reduces the increased rate of bone tissue renewal to the level of reproductive age, which leads to a progressive increase in bone mass, a decrease in the breakdown of bone collagen in urine and blood serum, the incidence of fractures and an increase in bone mineral density.
Contraindications
For all dosage forms of Bonviva:
- Hypocalcemia;
- Hypersensitivity of the patient to the components of the drug.
For solution and tablets of 2.5 mg:
- Pregnancy and lactation period.
Additionally for the solution:
- Severe renal dysfunction.
Additionally for 2.5 mg tablets:
- Age less than 18 years.
Tablets of 2.5 mg and 150 mg should be taken with caution in severe renal impairment.
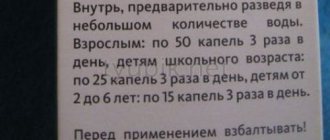
Directions for use and dosage
The osteoporosis medicine Bonviva is taken when bone mass cannot be maintained naturally through diet and exercise. Drug treatment for osteoporosis is prescribed by a doctor under the supervision of clinical blood tests. Doses and methods of administration are as follows:
- tablets with a dosage of 150 mg are taken once a month;
- tablets with a dosage of 2.5 ml are taken daily;
- injections. The drug is administered intravenously from a syringe tube with a capacity of 3 ml by a doctor once every 3 months.
The tablets should be taken standing and on an empty stomach an hour before meals so that it has time to be absorbed. Food, juices, mineral water reduce the absorption of the drug. Take the medicine with regular drinking water.
The selection of the optimal dosage of the drug was preceded by extensive clinical studies with different groups of patients. Patients in each group took bisphosphonates of varying dosages. Comparative test results showed that daily intake of 2.5 mg tablets and monthly intake of 150 mg of the drug are considered the safest and most effective.
There was a significant reduction in peripheral bone fractures by 38%. Of the proposed options for taking medications, the majority of patients chose to take 150 mg tablets once a month. This treatment regimen is considered the most convenient.
Instructions for use
The instructions for use indicate that Bonviva tablets for osteoporosis are prescribed in a dosage of 150 mg, they should be taken once every 30 days. Appointments are made on the same day of the month to avoid missed appointments. Tablets of 2.5 mg are taken 1 time/day.
Take the tablets with water 30 minutes before breakfast, do not chew them to avoid irritation of the esophagus and stomach by the components of the tablet. To take a tablet, you need about 200 ml of water. You cannot take Bonviva 150 mg, 2.5 mg tablets while lying down, and it is also contraindicated to lie down after taking it for an hour.
Drinking water with a large amount of calcium ions is contraindicated.
- If liver function is impaired, no dose adjustment is required.
- For mild and moderately severe renal dysfunction (creatinine clearance ≥30 ml/min), no dose adjustment is required. When CC < 30 ml/min, taking the drug is not recommended, because Experience with clinical use is limited.
- Elderly patients do not require dose adjustment.
If you miss the next monthly dose, you should take the pill as soon as possible, and take the next one according to the schedule established by your doctor. If your next appointment is more than 23 days overdue, you should wait until your scheduled appointment day and then continue with your schedule. Under no circumstances should you take 2 Bonviva 150 mg tablets within one week.
Directions for use and dosage of Bonviva
Bonviva tablets with a dosage of 2.5 mg are prescribed 1 pc. per day.
Bonviva 150 mg tablets should be taken 1 piece. per month on the same date. If you miss a dose, it is recommended to take the tablet as soon as possible and the next tablet as usual. If the drug is overdue for more than 23 days, then the tablet should be taken on the previously scheduled day and then adhere to this schedule. It is strictly forbidden to take more than 1 tablet of Bonviva 150 mg per week.
The tablets should be taken half an hour before meals, without chewing, with plenty of water. After taking the drug, you should not lie down for an hour.
Bonviva solution for intravenous injection is injected as a stream over 30 seconds . The injection is recommended once every 90 days. If you miss the next injection, it should be done as soon as possible, and the next injection should be given according to the new schedule 90 days after the last one.
Instructions for the solution
Bonviva solution is intended for intravenous administration only. The drug can only be administered by a specialist. It is necessary to avoid getting the drug into surrounding tissues and its intra-arterial administration. Do not use a solution that has changed color or contains impurities.
The syringe tube can only be used once. To administer the medication, use the supplied needles.
- 3 mg of Bonviva solution is administered intravenously as a bolus (over 15-30 seconds) once every 3 months.
During therapy, the patient is recommended to take additional vitamin D and calcium. If the next injection of the drug was missed, the injection should be given as soon as possible. Next, the drug is administered after 3 months from the last injection.
The drug should not be prescribed more than once every 3 months.
Side effects
Side effects common to all dosage forms of the drug include:
- Skin rash, urticaria, angioedema;
- Flu-like syndrome;
- Gastritis, diarrhea, dyspeptic disorders;
- Myalgia and arthralgia;
- Dizziness, headache;
- Osteonecrosis of the jaw (very rare).
When the drug is administered intravenously, a short-term decrease in calcium levels is possible, as well as the following side effects:
- Arterial hypertension;
- Scleritis;
- Reactions at the injection site;
- Gastroenteritis, constipation;
- Osteoarthritis, pain in bones and limbs;
- Phlebitis and thrombophlebitis;
- Urinary tract infections;
- Hypercholesterolemia;
- Upper respiratory tract infections and bronchitis.
When using Bonviva in the form of film-coated tablets, reactions such as duodenitis, stricture or ulcer of the esophagus and esophagitis are possible. For 2.5 mg tablets, back pain, weakness, urticaria and decreased alkaline phosphatase activity may additionally occur, and for Bonviva 150 mg - nausea and vomiting, dysphagia, gastroesophageal reflux, abdominal pain, flatulence, muscle spasm and stiffness.
Side effects
During the use of Bonviva, the following undesirable reactions from the body may be observed:
- Common (≥1/100 and <1/10): headache, esophagitis, nausea, gastritis, abdominal pain, gastroesophageal reflux disease, diarrhea, dyspepsia, skin rash, arthralgia, muscle cramps, musculoskeletal pain, myalgia, skeletal -muscle stiffness;
- Uncommon (≥1/1000 and <1/100): dizziness, dysphagia, esophageal ulceration or stricture, flatulence, vomiting, back pain, fatigue, inflammatory eye diseases (scleritis, uveitis, episcleritis);
- Rarely (≥1/10,000 and <1/1000): hypersensitivity reactions, duodenitis, facial edema, urticaria, angioedema.
In addition, transient flu-like symptoms often occur: chills, fever, arthralgia, myalgia, loss of appetite, nausea, bone pain, and increased fatigue. However, it is worth noting that in most cases the described phenomena were observed only after taking the first Bonviva tablet, were characterized by weak or moderate intensity, short duration and went away on their own without the use of any corrective therapy.
special instructions
- Before starting to use the drug, it is recommended to correct hypocalcemia and other disturbances in electrolyte balance and bone metabolism. Patients need to consume sufficient amounts of vitamin D and calcium. If patients do not receive enough of these substances from food, then they are required to additionally take them in the form of nutritional supplements.
- The use of oral bisphosphonates is often accompanied by esophagitis, difficulty swallowing, and the formation of gastric and esophageal ulcers. In this regard, special attention should be paid to following the recommendations for taking pills (standing or sitting position for an hour after taking).
- Osteonecrosis of the jaw has been observed with the use of bisphosphonates. Most of the cases were registered in patients with oncological pathologies during dental procedures, in people with postmenopausal osteoporosis or other diseases. Risk factors for osteonecrosis of the jaw include a diagnosis of cancer, concomitant treatments (corticosteroids, radiation therapy, chemotherapy) and other disorders (infection, anemia, gum disease, coagulopathy).
Bonviva
Osteoporosis can be confirmed by identifying low BMD (T index < -2 SD), a fracture (including a history) or low bone mineral density (T index < -2.5 SD) in the absence of a confirmed fracture.
Before using Bonviva®, hypocalcemia and other disorders of bone metabolism and electrolyte balance should be corrected. Patients should consume sufficient amounts of calcium and vitamin D. If the patient does not receive enough calcium and vitamin D from food, then additional calcium and vitamin D should be taken in the form of dietary supplements.
Before each injection, serum creatinine should be determined.
Patients with underlying medical conditions receiving nephrotoxic therapy who may experience deterioration in renal function should be closely monitored.
When bisphosphonates were used in patients with cancer, osteonecrosis of the jaw was observed, most often associated with tooth extraction and/or local infection (in particular, osteomyelitis). Osteonecrosis of the jaw developed mainly against the background of intravenous use of bisphosphonates, which was often accompanied by chemotherapy and the use of corticosteroids.
Osteonecrosis of the jaw has also been reported with oral bisphosphonates for the treatment of osteoporosis.
In the presence of associated risk factors such as cancer, radiation or chemotherapy, taking corticosteroids, as well as poor oral hygiene, a dental examination and appropriate preventive treatment are recommended before prescribing bisphosphonates.
During treatment with bisphosphonates, invasive dental procedures should be avoided.
Dental surgery during bisphosphonate therapy can increase the manifestations of osteonecrosis of the jaw. It is not known whether discontinuation of bisphosphonates reduces the risk of osteonecrosis. The decision to conduct treatment should be made for each patient individually after assessing the risk/benefit ratio.
When taking bisphosphonates, incl. and the drug Bonviva®, severe pain syndrome may occur: pain in joints, bones and muscles. Pain occurred both within 24 hours and several months after starting the drug; in most patients it resolved after stopping therapy; in some of them, symptoms recurred after re-administration of the same or a different drug.
Atypical subtrochanteric and diaphyseal femoral fractures have been reported with bisphosphonates, primarily in patients receiving long-term treatment for osteoporosis. A cause-and-effect relationship has not been established. Fractures of this type have also been observed in patients with osteoporosis who did not receive bisphosphonate therapy. Transverse and short oblique fractures can be localized along the entire length of the femur from the lesser trochanter to the supracondylar eminence. Atypical fractures occur spontaneously or as a result of minor injuries. In the weeks or months before a complete hip fracture occurs, patients experience hip or groin pain that is often accompanied by radiographic evidence of a stress fracture. Because atypical fractures are often bilateral, it is necessary to monitor the other hip in patients with a femoral shaft fracture. Poor healing of atypical fractures was noted. If an atypical fracture is suspected and pending examination results, discontinuation of bisphosphonate therapy should be considered based on an assessment of the benefit/risk ratio in each individual case.
Patients should be advised to report any hip or groin pain during bisphosphonate therapy. If these symptoms are present, it is necessary to conduct an examination to identify an incomplete hip fracture.
Use in pediatrics
Safety and effectiveness in children and adolescents under 18 years of age
not installed.
Impact on the ability to drive vehicles and operate machinery
There have been no studies on the effect of using Bonviva® on the ability to drive a car or use other machinery. The drug causes undesirable effects that may affect the ability to drive vehicles and machines.
Instructions for drug disposal
Destruction of syringes/needles
When using and disposing of syringes and other medical products containing needles, the following rules should be strictly observed:
- do not reuse syringes and needles;
— all used needles and syringes should be placed in containers (disposable, puncture-resistant containers);
— it is necessary to store the container in places inaccessible to children;
— Disposal of needle containers with household waste should be avoided;
- Containers filled with syringes/needles should be disposed of according to local regulations or as directed by a physician.
Patients should be provided with puncture-resistant containers for disposal of syringes and needles at home.
Destruction of unused medicinal product or after expiration date
The release of medicinal products into the environment should be minimized. Bonviva® should not be disposed of with wastewater or household waste. Where possible, special systems should be used to dispose of medications.
Drug interactions
Calcium foods and dietary supplements, antacids and oral medications containing calcium and other polyvalent cations (for example, aluminum, magnesium, iron), incl. milk and solid foods may interfere with the absorption of the drug, so they should be consumed no earlier than 60 minutes after taking Bonviva orally.
Bonviva does not affect the activity of the main isoenzymes of the cytochrome P450 system. At therapeutic concentrations, ibandronic acid binds weakly to plasma proteins and is therefore unlikely to displace other drugs from protein binding sites. Ibandronic acid is excreted only by the kidneys and does not undergo any biotransformation. It appears that the elimination pathway of ibandronic acid does not involve any of the transport systems involved in the elimination of other drugs.
Bonviva solution for intravenous administration is incompatible with calcium-containing solutions and other solutions for intravenous administration.
Reviews
We have selected some people's reviews about the drug Bonviva:
- Alexandra. After much hesitation, I finally took the pill. Of course, there are a lot of side effects. Before that, I suffered from constipation (sorry), but now it’s just tears, only enemas help, but you can’t do them all the time. The second point, I have problems with my hair (androgenic ) , they started to break out very badly after taking it, I had to go to mesotherapy more often. The condition of my heart also worsened, shortness of breath appeared, it was pressing. Now I’m wondering whether to continue drinking, osteoporosis has been confirmed.
- Lyudmila. I am 75 years old. I took Bonviva once a month for several years. Constant pain in the spine does not disappear, but what can you do - you cannot stop the destruction forever. Over the years, his height has decreased by 6 cm, and there is almost no clearance in the thoracic vertebrae. I am an allergy sufferer, and this drug is the only one to which I have no complaints. In January, the rheumatologist told me to take a break for 2-3 years, since recent bone density indicators had improved much, and for pain I take paracetamol 500 mg/codeine 30 mg. Today at the Pain Center they advised me to look for Bonviva in Russia and continue to take it... There are a lot of side effects in any drug, but if you can’t do without it, then it’s better not to read, but to decide for yourself - to live more or less normally or just curl up on the bed and not move ….I’m for Bonviva, I’ll try to find it in St. Petersburg’s pharmacies. Best regards, Lyudmila, Tallinn.
Women leave different reviews online. The negative point, in their opinion, is the high cost of the drug; patients also note that the drug causes side effects. But many users who have undergone treatment report that their bone health has improved significantly.
In the process of discussing the drug Bonviva, doctors’ reviews are also different. But in general, they assess the effect of the drug positively.