Inflammation of the vulva is called vulvitis, and inflammation of the vaginal mucosa is called vaginitis. These diseases are often combined with each other, which is called vulvovaginitis. There are two mechanisms for the development of such a disease:
- Primary - vaginitis. In this disease, microorganisms that provoke inflammation release decay products and toxins. As a result, the glands begin to work more actively, and the volume of discharge from the genital tract increases. They have an irritating effect on the vulva, which leads to general inflammation;
- Primary - vulvitis. There is an ascending infection. In the absence of treatment for vulvitis in women, the pathogenic flora “rises” higher to the vaginal mucosa, provoking inflammation.
There are also cases of simultaneous spread of inflammation to all mucous membranes of the genital tract. The cause may be both pathogenic microorganisms and those that are present in the flora in small quantities in a normal state.
Causes of vulvitis
Against the background of severe viral infections, disruptions in the gastrointestinal tract and immunity, even a wet swimsuit or cold stool can cause vulvitis.
The development of vulvitis is provoked by:
- vegetoneurosis;
- tight clothes;
- increased sweating;
- synthetic pads and underwear;
- poor hygiene during menstruation;
- injury to the mucous membrane and skin in the pubic area;
- taking heavy antibiotics or a course of radiation therapy;
- constant humidity in the area of the external genitalia;
- maceration of the vulvar mucosa with secretions from the cervical canal or vagina;
- metabolic and hormonal dysfunctions: diabetes mellitus, vitamin deficiency, ovarian hypofunction, allergic reactions, obesity.
The risk of developing an inflammatory process is significantly increased by delicate mucous membranes, folds, and accumulation of blood vessels and nerve endings near the surface of the epidermis. In rare cases, vulvitis is diagnosed against the background of diphtheria, tuberculosis, or immunodeficiency.
Vulvitis is caused by the following infections and fungi:
- chlamydia;
- gonococci;
- helminths;
- Trichomonas;
- streptococci;
- staphylococci;
- coli;
- yeast fungi.
How to cure vulvitis
A gynecologist conducts an examination and takes all the necessary tests. The On Clinic medical center has modern diagnostic equipment. After receiving the results, a final diagnosis will be made and the correct treatment will be selected.
To treat vulvitis, complex therapy is used, both local and general. The first step is to relieve acute inflammation, which is accompanied by itching and pain. Women are advised to abstain from sexual intercourse.
It is very important not to procrastinate with this disease and seek professional help in a timely manner. Our clinic’s specialists will be able to prescribe effective treatment for vulvitis, taking into account the individual characteristics of the patient.
If you do not consult a doctor in time, this disease develops into a chronic disease, which is characterized by frequent relapses. For girls, this can lead to fusion of the labia; in adult women, the genitals may become deformed, which will cause discomfort during intimacy. In addition, if vulvitis is not treated in girls, the outcome may be more disastrous - not taking inflammation of the external genital organs seriously can lead to infertility.
Causes of vulvovaginitis, treatment and first symptoms
Vulvovaginitis is one of the most common gynecological diseases. Girls of the first year of life, as well as persons of prepubertal and postmenopausal age groups are most susceptible to this pathology. But in the presence of predisposing factors, combined lesions of the vulva and vagina can also develop in women of reproductive age.
Although vulvovaginitis is not a potentially life-threatening condition, special attention is paid to its treatment. This is due not only to the physical discomfort that patients experience.
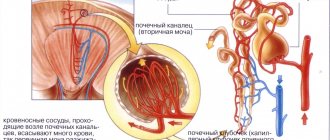
Inflammation of the external genitalia and vagina can be complicated by an ascending urinary infection with the sequential development of urethritis, cystitis and pyelonephritis.
Possible damage to the cervix with infection of the endometrium.
What it is?
Vulvovaginitis is inflammation of the vulva (vulvitis) and the vaginal mucosa (vaginitis). It occurs mainly in girls, elderly women and very rarely in women of childbearing age. The causative agents of vulvovaginitis are purulent and intestinal flora, helminths (pinworms), etc.
Classification of vulvovaginitis
Currently, several characteristics of the disease are taken into account when making a diagnosis. Therefore, several clinical classifications of vulvovaginitis are used simultaneously:
- By type of pathogen: nonspecific bacterial, specific, tuberculosis, diphtheria, viral, fungal (candida), protozoal.
- According to the presence of an infectious agent: infectious and primary non-infectious.
- By type of course: acute, subacute and chronic.
Primary non-infectious forms of the disease include allergic vulvovaginitis, inflammation due to foreign bodies in the vagina, masturbation and trauma, helminthic infestations, tissue changes due to dysmetabolic and endocrine disorders.
Signs of chronic vulvovaginitis
The chronic form of vulvovaginitis is characterized mainly by constant itching in the vulva and whitish thick “curdled” vaginal discharge. Redness, swelling, pain and burning disappear. For little girls, this stage of the disease is dangerous due to fusion (synechia) of the labia, up to the closure of the urethra.
A long course of vulvovaginitis can contribute to the formation of condylomas, polyps, and scar formations in the vagina, which in the future can negatively affect a girl’s sex life and her reproductive function. Less commonly, severe damage and rejection of the vaginal mucosa occurs.
Treatment of vulvovaginitis
After identifying the cause of vulvovaginitis , etiotropic treatment begins:
- if vulvovaginitis has developed due to another disease, it is necessary to treat the underlying disease,
- for allergic vulvovaginitis, it is enough to stop exposure to the allergen and use an antiallergic drug, such as Suprastin or Zoditec,
- vulvovaginal candidiasis is treated with the following drugs: Clotrimazole (vaginal tablets and 1% cream), Miconazole (2% cream or vaginal suppositories), Butoconazole (vaginal cream), Tioconazole (6.5 ointment), Terconazole (vaginal suppositories, cream), Nystatin (vaginal tablets), Fluconazole (150 mg - single dose, tablets orally), Diflucan,
- for the treatment of bacterial vulvovaginitis the following are used: Metronidazole (tablets or vaginal gel), Clindamycin in tablets and in the form of 2% vaginal cream, Terzhinan (vaginal tablets), Polygynax, oral tablets - Augmentin, Ampicillin, Cefradine,
- for vulvovaginitis caused by the herpes virus, the following are used: Zavirax, Acyclovir, Valocyclovir, Larifan, Neovir,
- Metronidazole and Tinidazole (oral tablets) are used in the treatment of trichomonas vulvovaginitis.
To alleviate the condition and relieve the inflammatory process in the area of the external genitalia, baths with chamomile, calendula, sage, St. John's wort, eucalyptus or soda are used. There are special aerosols for irrigation of the genitals (Hyposol). To restore the proper microflora of the vagina, vaginal suppositories “Vagilak” or “Acilakt” and the introduction of lactobacterin are used.
Prevention
You can reduce the risk of developing an inflammatory process by following simple rules such as:
- the use of contraceptives, which are selected together with the attending physician,
- undergoing regular examination by a gynecologist,
- exclusion of casual sexual relations,
- maintaining intimate hygiene,
- timely and correct treatment of infectious lesions,
- wearing underwear of the appropriate size, choosing natural hypoallergenic fabrics,
- limiting the use of hygiene products with strong aromatic fragrances and artificial colors,
- refusal of frequent douching in order to preserve the natural microflora of the vagina,
- use antibiotics only on the recommendation of a doctor, take probiotics.
Vulvovaginitis is not a serious disease, but it causes severe discomfort. With timely diagnosis and proper treatment, it goes away quickly. When the first symptoms appear, a woman or girl is advised to see a doctor. Self-therapy at home is also not worth it to prevent complications.
Source: https://infeksiya.ru/bolezni/ginekologiya/prichiny-vulvovaginita-lechenie-i-pervye-simptomy-foto.html
Causes of the disease
The proliferation of opportunistic and pathogenic microorganisms is the main cause of inflammation. Several factors can “predispose” the surface of the mucous membranes to this:
- Poor hygiene: too infrequent or frequent washing;
- Mechanical microdamage to the mucous membranes during active sexual activity, wearing tight clothing, accidental injury during washing, gynecological intervention;
- Chemical exposures and allergies - to underwear, sanitary pads, including those used for urinary incontinence, etc.;
- Antibacterial therapy (causes microflora disruption);
- Hormonal changes - menopause, pregnancy, puberty in girls;
- Endocrine disorders - insufficient ovarian function, diabetes mellitus;
- Metabolic disorders - lack of vitamins/minerals;
- Fistulas of the intestines, urinary system.
Based on the reasons, primary vulvitis is distinguished, when inflammation forms as a result of damage or poor hygiene, and secondary - the cause of the disease is inflamed organs (uterus, kidneys, etc.).
Thus, in sexually mature women, the mucous membrane is better protected from the proliferation of bacteria and fungi, which is associated with the composition of the flora (lactic acid bacteria, etc.), and the level of acidity of the secretion. In girls, the mucous membranes are thinner, and the microflora is dominated by cocci, the secretion environment is alkaline. During menopause, a decrease in the level of female sex hormones leads to structural changes in the mucous membrane and atrophic processes. There is less secretion, the mucous membrane becomes thinner, and is not sufficiently moisturized. It is susceptible to microtraumas and infections.
Reasons for development
The following reasons most often lead to the development of inflammation in the vulva:
- Violation of personal hygiene rules, sex with casual partners, including oral. In this case, infectious vulvitis usually develops. Depending on the flora that caused its development, it is in turn divided into specific (gonorrheal, trichomonas, tuberculosis, diphtheria, etc.) and non-specific. In the latter case, the causative agents of the disease may be E. coli, streptococcus, enterococcus, pathogenic fungi, etc.
- Long-term use of certain medications (hormones, antibiotics, immunosuppressants), which helps to reduce the body's defenses and the death of normal microflora. As a result of this, patients often experience various forms of dysbiosis, including vulvitis, which is usually fungal in nature.
- Some systemic diseases, such as leukemia, diabetes.
- Disintegration of malignant tumors of the ovaries, uterus, cervix or vagina.
- Other infectious and inflammatory gynecological (endometritis, endocervicitis, vaginitis) and/or urological (cystitis, urethritis, urinary incontinence, genitourinary fistula) diseases.
- Helminthic infestations (helminthiases).
- Allergic reactions to some components of cosmetics and perfumes (deodorants, scented sanitary napkins, soap, etc.).
- Wearing synthetic underwear.
- Use of local contraception.
- Irritation of the vulva with chemicals, for example when washing with concentrated solutions of antiseptic drugs.
- Mechanical irritation of the external genitalia that occurs during masturbation, cycling, and horse riding.
- Taking hot baths or douching with a hot solution.
Most often, vulvitis is observed in girls before menarche and in women after menopause. This is due to the fact that low estrogen levels create optimal conditions for maintaining the activity of the inflammatory process in the genitals.
Symptoms of the disease
Inflammation of the mucous membranes has a number of characteristic symptoms. They depend on whether only the vulva is susceptible to inflammation or whether the tissue of the vaginal mucosa is involved. In general, this condition is characterized by:
- Swelling, redness of the vulva, sometimes - the appearance of areas of erosion, ulcers;
- Painful sensations, burning, itching (unpleasant symptoms intensify with physical activity, acts of defecation, urination, sexual intercourse);
- Increased discharge, its atypical nature: serous-purulent, curd-like, ichorous appear (depending on the causative agent of the infection, the severity of the disease). So, when infected with E. coli, watery leucorrhoea appears, with staphylococcus - yellow, and with candidiasis - curdled white plaque.
Due to itching and pain, irritability, insomnia, and decreased libido may occur. Girls may show signs of increased nervous excitability and sleep disturbances.
Classification, diagnosis and symptoms of vulvitis
There are acute and chronic forms of the disease. Acute vulvitis is characterized by a sharp and sudden onset, often with signs of general intoxication - weakness, chills, fever. The key symptom is itching, burning and redness of the external genitalia. There may be severe pain in the perineal area, which intensifies during sexual intercourse, walking and urination.
Even a medical student knows what vulvitis looks like. Therefore, it is not difficult to make a diagnosis; the doctor becomes aware of the disease already during the initial examination in the chair. All external genital organs show obvious signs of inflammation: swelling, redness, and sometimes deformation. The clitoris may thicken, and the labia may acquire a heterogeneous structure.
Chronic vulvitis usually develops as a result of an incorrectly or insufficiently treated acute form. Microorganisms develop resistance to etiotropic drugs, after which the disease becomes chronic. It is characterized by a sluggish and blurred course, with periods of remission and exacerbation.
Depending on the etiology, vulvitis is classified into primary and secondary. Primary vulvitis usually occurs against the background of an inadequate immune response, the coincidence of a number of provoking factors and underlying diseases, such as diabetes, which further reduce the resistance of the vulva to external infectious and other agents.
Secondary vulvitis (occurs more often) is observed due to related inflammatory diseases of the reproductive system or pelvic organs. Usually these are diseases in which there is vaginal discharge: endometritis, cystitis, urethritis (purulent), endocervicitis, adnexitis, and so on. Pathogens through secretions enter the external genitalia and infect them - thus developing secondary vulvitis.
In addition to the main symptoms, especially in the case of acute vulvitis, there are several additional signs that can help make the correct diagnosis. For example, the mucous membrane of the labia minora may become covered with small blisters and become grainy and rough to the touch. These are inflamed and enlarged sebaceous glands, which are also affected by infection.
Various plaques, ulcerations, films and areas of roughness on the skin and mucous membrane of the vulva may also be observed. However, this occurs much less frequently and is associated with atypical infectious pathogens, for example, the herpes virus or diphtheria bacillus. Vulvitis, the symptoms of which are unusual, requires additional attention from a doctor.
If adequate treatment and care for the affected area is not observed, the disease may become more complicated or spread beyond the genitals. As a result, the inflammatory process spreads to the perineum and even the surrounding skin (thighs, buttocks, and so on).
Symptoms of vulvitis in women
During the acute phase of inflammation, the following is observed:
- swelling and redness of the external genitalia;
- itching, burning;
- painful sensations when urinating, walking, sexual intercourse;
- mucous plaque mixed with pus;
- enlarged inguinal lymph nodes;
- temperature increase;
- general weakness, fatigue.
Signs of vulvitis in chronic form are the same symptoms, but in a less pronounced form. As the pathology develops, ulcers of the mucous membrane and scars appear that deform the surface.
Vulvitis: symptoms and treatment
Vulvitis is an inflammatory process affecting the vulva (as the external female genitalia are called in medical terminology). This disease occurs quite often in clinical practice, and it affects not only adult women, but also very young girls, as well as elderly patients, and in all cases absolutely the same symptoms are observed.
With the development of the pathological process, the labia majora and minora, the clitoris, the vestibule of the vagina, as well as the hymen (in girls who have not yet been sexually active) become inflamed. Vulvitis is characterized by the appearance of burning and itching in the area of the external genitalia, swelling and hyperemia of the labia, the occurrence of copious discharge and pain that intensifies after urination.
Signs of vulvitis
In gynecology, a distinction is made between chronic and acute forms of the disease. The photo of a patient with vulvitis clearly shows hyperemia, redness and modified mucous membrane.
Signs of acute vulvitis:
- swelling of the clitoris;
- itching and burning of the vulva;
- redness of the labia;
- enlargement of sebaceous glands;
- the appearance of ulcers and erosions;
- painful urination;
- roughness of the labia minora;
- bloody or serous-purulent discharge;
- damage to the inguinal folds (in rare cases);
- blisters with fluid (herpetic vulvitis);
- enlarged lymph nodes in the groin, sometimes an increase in temperature may be recorded;
- curdled, yellow-green or white discharge of a watery nature (if the cause of vulvitis is E. coli, staphylococcus).
Manifestations of chronic vulvitis:
- swelling of the vulva;
- itching and discharge;
- epithelial defects;
- hyperemia on the vulva;
- redness of mucous membranes;
- hypertrophy of the sebaceous glands.
Types and forms of vulvitis
In clinical practice, a distinction is made between primary (isolated) and secondary vulvitis.
1. It should be noted that in adult women the primary form of the disease practically does not occur, since the mucous membrane, due to the predominance of fermented milk microflora, normal hormonal levels and an acidic pH environment, is more resistant to infection. However, primary vulvitis is quite often registered among old women and girls. This condition occurs due to the anatomical and physiological characteristics of the vulvar mucosa and changes occurring due to low levels of female sex hormones. In women of advanced years, during the postmenopausal period, atrophy of the mucous membrane of the urogenital organs is observed, the amount of vaginal discharge is significantly reduced, the mucous membranes become thinner and dry out. As a result, they are easily damaged and become extremely vulnerable to infection.
In childhood, the skin and mucous membranes of the vulva are thinner, and therefore they are easily injured. The vaginal microflora of girls, in contrast to the “adult” microflora, is predominantly coccal, the pH is alkaline, and local immunity is not fully formed. Also, very often, vulvitis in girls can occur due to the presence of pinworms. They cause severe itching; scratching causes injury to the mucous membrane and infection. Sometimes vaginal discharge occurs in newborn girls. They are provoked by maternal estrogens entering the child’s body before birth. This condition should not be considered a pathology, and it will soon go away on its own.
2. Secondary vulvitis is a pathological condition that is much more common. It occurs due to irritation of the external genitalia by infected vaginal and cervical discharge or infected urine (in case of urinary tract diseases).
Depending on the type of pathogen, it is customary to distinguish between bacterial and candidal vulvitis, and depending on the nature of the pathological transformations of the mucous membrane of the external genitalia, vulvitis is divided into atrophic, ulcerative and adhesive.
Candidiasis vulvitis
This is a disease caused by yeast-like fungi from the genus Candida. It affects the labia majora and minora, the clitoris and the vestibule of the vagina. As a result, severe itching and burning develops, which intensifies before the onset of menstruation and subsides slightly in the postmenstrual period. In patients with candidiasis vulvitis, the mucous membranes acquire a purple-bluish color, sometimes rashes in the form of small bubbles (vesicles) appear on the vulva, and a white cheesy film forms in the area located between the labia minora.
In women suffering from ovarian hypofunction, diabetes mellitus and myxedema, the pathological process sometimes spreads to the perianal region and to the femoral-inguinal folds.
Bacterial vulvitis
Bacterial vulvitis is a pathological condition provoked by opportunistic microflora or sexually transmitted infections (gonococci, trichomonas, chlamydia). Mycobacterium tuberculosis can provoke the disease much less often.
During pregnancy, bacterial vulvitis, as a rule, develops against the background of reduced immunity, due to the activation of staphylococcal microflora. Due to the significant functional and hormonal changes occurring in the body of the expectant mother, specific and nonspecific pathogens are much easier to penetrate into the thickness of the mucous membrane of the external genitalia.
Atrophic vulvitis
This form of pathology is characterized by thinning of the vulvar mucosa, which very often occurs in women after menopause. It should be emphasized that without hormone replacement therapy, atrophic vulvitis will steadily progress and, ultimately, lead to the formation of painful erosions.
Ulcerative vulvitis
Ulcerative vulvitis is a chronic form of the pathological process, which is characterized by the formation of plaque on the damaged mucous membrane of the external genitalia, in the place of which, after removal, ulcers remain. Most often, this pathology is found in patients of reproductive age.
Note: After the ulcers heal, there is often obvious deformation of the external genitalia.
Adhesive vulvitis
Adhesive vulvitis, or fusion (synechia) of the labia minora, is a disease of unknown etiology that occurs in girls under five years of age. It is characterized by sticking together of the labia, which is how it got its name. At an early stage of the pathological process, an epithelial bridge is formed between the labia minora, which almost completely covers the vulva. In some cases, children complain of slow urination, but at the same time, much more often, synechiae are detected completely by accident, during a thorough examination of the external genitalia. In this case, the labia minora are connected along the “edge” to the anterior edge, where a small hole remains from which urine comes out.
As a rule, this condition does not cause any subjective sensations, and with the onset of puberty it heals itself. However, with the development of a rough adhesive process, in some cases surgical intervention (dissection of the labia minora) is indicated.
Consequences of vulvitis
The acute form of vulvitis in children is accompanied by nervous excitability and sleep disturbances. If diagnosis and treatment are not timely, the disease develops into a relapsing chronic form.
As a result of vulvitis suffered by a girl at an early age, genital deformities develop and fusion of the labia minora (synechia) occurs. Untreated chronic inflammation can subsequently cause anorgasmia, miscarriages, and infertility.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Symptoms of the disease and causes
A burning sensation and constant obsessive itching, as well as swelling of the tissues; in the most advanced cases, ulcers, pain when urinating, uncharacteristic yellow or greenish discharge (in the presence of ulcers, it may be mixed with blood) color are observed - these are clearly expressed symptoms of vulvitis.
With this disease, there is an unpleasant odor that does not disappear after hygiene procedures, pain during sexual intercourse and when wearing tight-fitting clothes. Sometimes an increase in temperature may occur.
There are many photos posted on the Internet where you can see redness, small vesicles, and pimples on the external genitalia of girls with vulvitis.
If you detect at least one or more symptoms, you must definitely go and see a doctor for examination.
It is necessary to get rid of vulvitis as quickly as possible at the initial stage, so the treatment will be short-lived and will not have time to cause any complications.
The causes of occurrence are divided into primary and secondary.
Primary causes of vulvitis:
- The presence of parasites, helminths (most often in children);
- Lack of hygiene, use of aggressive agents, as they can cause allergies and rashes;
- Violation of the acidic microflora of the vagina, both by local medications and by taking antibacterial agents;
- Unprotected (without barrier means) sexual contacts;
- Violation of the integrity of the skin or mucous membrane of the genital organs, any injuries.
Secondary causes of vulvitis:
- Inflammatory processes in other organs;
- Fistulas, weak immunity;
- If there are skin diseases, psoriasis or sometimes eczema may occur;
- And also if you have allergies, this can also lead to the development of vulvitis.
Women who have already crossed the age of 40–50 years are most susceptible to vulvitis. Their female hormone estrogen drops, which affects the vagina and the normal state of the flora. Conditionally pathogenic bacteria can change their character to pathogenic and cause inflammation. But only under the condition of the necessary environment for this.
Pathogens:
- streptococci;
- chlamydia;
- candida fungi;
- trichomoniasis;
- enterococcus;
- coli;
- other pathogenic bacteria.
Vulvitis is divided into chronic and acute forms:
- Chronic form - during remission (external well-being, absence of symptoms), many of the symptoms may be absent. But under unfavorable conditions in the case of illness, a cold, or simply a drop in immune defense, it can turn into an acute form. The chronic form develops in the case of a very long course of the disease, without treatment. It is more dangerous because this external well-being is dangerous, there is inflammation, which means the body is constantly in a state of stress.
- Acute form - all the symptoms are very pronounced, there is no relief. Treatment and diagnosis are necessary.
Diagnosis of vulvitis
The diagnosis of vulvitis is made based on examination of the patient’s external genitalia. For an accurate diagnosis, the gynecologist uses a hand-held magnifying glass, conducts vaginal-abdominal and rectal examinations, takes a smear for cytology, and examines peripheral lymph nodes.
To identify the causes of the inflammatory process, additional diagnostics are required:
- Analysis of urine;
- vulvoscopy;
- HIV test, RW;
- general blood analysis;
- cultural sowing;
- bacterioscopy of smears;
- tests for helminths (feces or blood).
Treatment of vulvitis
Complex therapy for inflammation of the external genitalia includes:
- drug correction;
- intravaginal irrigation and baths;
- supportive therapy (homeopathy, hormones, macroelements, vitamins, immunostimulants).
During treatment, women are advised to refrain from sexual intercourse, going to the pool and the beach, and are prohibited from using vaginal tampons and panty liners. If a bacterial source of vulvitis is identified (candidiasis, tuberculosis, gonorrhea, chlamydia, trichomonas fungus), appropriate medications are prescribed (injections, tablets, suppositories, creams).
In little girls, in most cases, inflammation of the labia is provoked by opportunistic microflora. The photo of vulvitis in children shows redness not only in the area of the external genitalia, but also inflammation in the inguinal folds, on the thighs and buttocks. The gynecologist prescribes local antibiotics in the form of ointments and baths with anti-inflammatory herbs (chamomile, calendula, string, eucalyptus).
To relieve symptoms of acute vulvitis, the following therapeutic methods are used:
- Ural Federal District;
- hydrocortisone ointment;
- anti-inflammatory suppositories;
- baths with herbs and potassium permanganate;
- compresses with Furacilin, lead water, eucalyptus infusion;
- irrigation of the external genitalia with potassium permanganate, boric acid solution;
- the use of powders with streptocide, camphor, folliculin, zinc oxide, talc, anesthesin.
If vulvitis is allergic, antihistamines and dietary supplements are prescribed.
How to treat vulvitis in girls
Vulvitis in girls must be treated with special care. Treatment begins immediately after the examination, since the child suffers greatly from the symptoms of the disease. Treatment for children should be comprehensive (general and local). Special powders and sitz baths with a pale pink solution of potassium permanganate, antibiotics, anthelmintics and vitamins are recommended.
Vulvitis during pregnancy
During pregnancy, the body begins to produce hormones that promote growth, fetal formation and a favorable course of pregnancy. All endocrine glands of the body are completely rebuilt: reproductive, thyroid, adrenal glands, pituitary gland. At the same time, the adrenal glands sharply increase the production of glucocorticoids and mineralocorticoids, which suppress the mother’s immunity to preserve the fetus.
The most common causes of vulvitis in pregnant women are yeast, E. coli, staphylococci and streptococci. In the first and second trimesters of pregnancy, candidal vulvitis, hyperpigmentation and striae formation are often diagnosed. The gynecologist must select the optimal therapy for the pregnant woman and a set of supportive procedures to prevent relapses. Untreated vulvitis can lead to infection of the fetus during passage through the birth canal.
Folk remedies for treating vulvitis
It should be noted that herbal infusions, plant juice and any homeopathic medicines are not able to cure vulvitis, which is caused by gonorrhea, trichomonas fungus, tuberculosis, herpes, staphylococcus or chlamydia. Folk remedies help only with the non-infectious nature of the disease.
Proven anti-inflammatory and immunostimulating agents:
- Kalina. A tablespoon of dried inflorescences is poured into a glass of water and kept in a steam bath for 8-10 minutes. The strained decoction should be taken three times a day, one tablespoon at a time.
- Stinging nettle. Young nettle leaf juice is taken one teaspoon three times a day.
- St. John's wort. A tablespoon of dried collection is poured with a glass of boiling water and left for 40-50 minutes. The decoction is filtered and drunk 50 ml three times a day.
- Wintergreen round-leaved. The succulent leaves of the plant are doused with boiling water, crushed and applied to the vulva for 5-10 minutes. Such phytoapplications are good at relieving itching, burning and hyperemia of the mucous membrane.
- Lungwort. Freshly squeezed juice of the leaves of the plant is diluted 50/50 with water and applications are made to the vulva twice a day. Lungwort has anti-inflammatory and antiseptic effects.
Vulvovaginitis in women and girls
Vulvovaginitis (vulvovaginosis) is inflammation of the mucous membranes of the vulva and vagina. The disease can be infectious or non-infectious in nature. It is not difficult to identify vulvovaginitis; it is enough to recognize the symptoms in time and begin treatment.
Causes
- failure to comply with intimate hygiene rules;
- long-term use of antibacterial drugs, corticosteroids, cytostatics, etc.;
- frequent washing with alkaline reaction products;
- regular vaginal douching;
- wearing uncomfortable (tight) underwear;
- injuries when introducing any objects into the vagina;
- chronic diseases (diabetes mellitus, obesity, helminthiases, diseases of the genitourinary system), leading to a decrease in local immunity;
- the formation of diaper rash as a result of insufficient air access to the genitals;
- improper use of tampons;
- disturbances in the blood flow of the external genitalia and vagina in women over fifty years of age;
- allergies to medications, contraceptives, condoms and lubricants;
- decreased immune function;
- hypovitaminosis and vitamin deficiency;
- hypothermia.
The direct causes of the development of vulvovaginitis include infection with the following microorganisms:
- bacteria: streptococci, staphylococci, Haemophilus influenzae and Escherichia coli, enterococci, gonococci, chlamydia;
- herpes viruses or HPV (human papillomavirus);
- fungi from the genus Candida;
- protozoa: Trichomonas and amoebas.
In addition, vulvovaginosis can be caused by helminthic infestation (enterobiasis, pinworm infection).
Symptoms of the disease
- burning and itching in the genital area;
- the appearance of vaginal discharge (yellow, green, yellow-green, brown, cheesy).
The nature of the discharge may be different.
If the disease is caused by bacteria, then the vaginal secretion is thick, heterogeneous, and purulent. With vulvovaginitis caused by Trichomonas, the discharge is purulent, foamy, with an unpleasant fetid odor.
A fungal infection is characterized by a curd-like discharge.
During an examination of the genital organs, the doctor pays attention to the following signs:
- Swelling and redness of the mucous membrane. Such a change can affect the labia, the area of the vestibule of the vagina, and the vaginal walls.
- The appearance of erosions. This symptom is characteristic of herpetic and diphtheria vulvovaginitis.
- Formation of bubbles filled with clear liquid. This symptom is characteristic of herpes.
- Synechia (fusion) between the labia minora. Often found in young girls. The cause is chronic vulvovaginitis.
Acute vulvovaginitis can also manifest as general symptoms, especially for girls of preschool age. In this case, the child may become capricious, whiny and get tired quickly. If the patient is sexually active, then symptoms arise in the form of decreased sexual desire, anorgasmia and pain during sexual intercourse.
Types of vulvovaginitis
Depending on the causative agent of the disease, there are several types of vulvovaginitis:
- bacterial;
- fungal;
- viral;
- atrophic.
Separately, there is a specific vulvovaginitis caused by chlamydia, gonococci, trichomonas and other pathogenic microorganisms.
Fungal vulvovaginitis occurs due to the proliferation of a fungus (most often the genus Candida). There are two possible flow options:
- Acute candidal vulvovaginitis is characterized by pronounced symptoms in the form of: swelling and hyperemia of the labia, vestibule and vaginal walls;
- severe itching and burning;
- white discharge with a cheesy consistency.
Signs of trichomonas vulvovaginitis:
- itching;
- redness of the vulva;
- burning in the area of the external genitalia and vagina;
- vaginal discharge is yellowish-green in color with an unpleasant odor;
- pain during intercourse;
- pain when urinating (if the disease is accompanied by urethritis).
Trichomoniasis can occur without symptoms or, conversely, with their intensification during menstruation.
Chlamydial vulvovaginitis refers to infections that are transmitted sexually and domestically. It is characterized by such symptoms as itching in the perineum, painful urination, and scanty mucous discharge. The disease may be asymptomatic. Often the only manifestation of chlamydia is infertility.
https://www..com/watch?v=vHQUEJPhL_U
With atrophic vulvovaginitis, there is a decrease in the secretion of vaginal mucus and active proliferation of bacteria on the surface of the labia and vagina. Occurs in women over fifty years of age due to a decrease in estrogen levels during menopause.
Diagnostics
PCR and ELISA diagnostics are actively used to identify pathogens.
In childhood, the doctor prescribes an examination of the body for the presence of helminths. To do this, you need to take a stool test three times and scrape for enterobiasis. If there is a need for further research, a serological blood test is prescribed.
To assess the condition of the vaginal walls in girls, the examination should be carried out as carefully as possible to preserve the hymen. Mirrors are not used during examination of the child. An informative way of diagnosing is to use a vaginoscope, which is equipped with a camera and a light bulb.
If a woman has vulvovaginitis, the doctor should evaluate the condition of the cervix and other organs. According to indications, it is recommended to undergo colposcopy, ultrasound of the uterus and appendages using an abdominal or vaginal sensor.
Treatment
Therapy includes taking antibiotics, which are available in the form of suppositories, vaginal tablets or creams.
- The most convenient means of treatment are suppositories or vaginal tablets. In most cases, broad-spectrum antibiotics or antiseptics are used; for fungal infections - antimycotics. To restore the vaginal microflora after a course of antibacterial therapy, it is recommended to use special products - probiotics.
- The treatment process includes the use of sitz and vaginal baths. Hydrogen peroxide, furatsilin, chlorhexidine, lysozyme can be used as solutions. To avoid burns to the mucous membrane, you must follow the dosage prescribed by your doctor.
- Decoctions of sage, chamomile, eucalyptus or calendula are used as anti-inflammatory agents. It is important to remember that folk remedies refer to additional activities. They cannot completely rid a woman of the problem.
- Physiotherapy for vulvovaginosis includes ultraviolet and UHF perineal irradiation, darsonvalization, electrophoresis, and laser irradiation of blood. These techniques make it possible to shorten the duration of treatment and eliminate unpleasant symptoms.
- Antimicrobial and anti-inflammatory therapy is supplemented by taking vitamin complexes and immunostimulating drugs. If necessary, the doctor can prescribe medications to eliminate the lack of estrogen, drugs for worms. They also sanitize foci of chronic infection.
During the treatment process, a woman should refuse sexual relations. They can be resumed only when the treatment is over.
Treatment of vulvovaginitis in girls
Suppositories and vaginal tablets are not prescribed to girls, so doctors give preference to creams. Local procedures have proven themselves to be excellent. These include baths with the addition of medicinal herbs and antiseptic solutions. Ultraviolet irradiation of the perineum is also carried out.
If a child has a tendency to masturbate and insert various objects into the vagina, then consultation with a psychologist, neurologist and psychiatrist is required. In some situations, medications are prescribed to prevent neurotic and behavioral disorders.
Parents of girls are taught hygiene rules and given several recommendations on choosing children's underwear and laundry products.
Preventive actions
- daily washing;
- wearing high-quality underwear made from natural fabrics;
- refusal to wear tight and tight-fitting panties;
- refusal of uncontrolled use of antibiotics;
- eliminating the frequent use of gaskets.
Vulvovaginitis is not a serious disease, but it causes severe discomfort to the patient. With timely detection and proper treatment, the disease resolves quickly. You should not self-medicate.
When the first symptoms are detected, a woman or girl should see a doctor.
Vulvovaginitis - causes, symptoms, diagnosis, treatment
Vulvovaginitis is the most common disease in girls and older women. In adolescents and women during the reproductive period, the disease is diagnosed extremely rarely. What causes provoke the development of the disease, what symptoms and diagnostic measures are characteristic of vulvovaginitis, as well as treatment methods will be discussed in the article.
General information about vulvovaginitis
Vulvovaginitis is a disease that affects the lower parts of the female genital organs . From a medical point of view, these are two diseases - vulvitis and vaginitis - combined into one.
Vulvitis is an inflammatory process affecting the external female genitalia (Vulva).
Vaginitis is an inflammation of the vaginal mucosa in which bacteria multiply.
According to statistics, vulvovaginitis is most often diagnosed in girls from 2 to 9 years old, in women who have reached menopause, and also during pregnancy.
Unfortunately, patients rarely talk about the pathology, considering the disease something shameful, but doctors recommend not postponing a visit to the gynecologist, since otherwise serious complications are possible - scarring on the walls of the vagina, fusion of the labia, reproductive dysfunction. It is especially important to prevent complications in girls, so that the disease does not lead to serious consequences in the future.
Some statistics
Among obstetric and gynecological pathologies, vulvovaginitis accounts for 60% of all diseases of an infectious nature. During the perimenopausal period (from 45 years to menopause), the disease is detected in 10% of patients. At the age of 55 to 60 years, the percentage of cases increases to 30%, and at 75 years and older, 2/3 of patients experience characteristic symptoms.
The mechanism of development of vulvovaginitis is associated with changes in the microflora in the female genital tract. In the body of a healthy woman, the genital tract contains aerobic and anaerobic microorganisms in a ratio of 1:10, respectively. The dominant vaginal flora is lactobacilli .
They are the ones who maintain the acidic environment of the vagina, in which pathogenic microflora die. With a change in acidity, the vaginal flora changes, and pathogenic microbes easily enter the body. Thus, vulvovaginitis and other infectious pathologies develop.
Causes of vulvovaginitis
Regardless of the type of disease, the main cause is infection with pathogenic microbes, pinworms and yeast-like fungi.
In addition, thermal, chemical and mechanical factors play a role in the development of the pathological process.
In childhood, the inflammatory process manifests itself due to insufficient care. By the way, excessive hygiene procedures can also provoke gynecological disease.
Important! A child is strictly prohibited from sharing the same set of bed linen and towels with his mother or sister.
Other causes of illness in childhood:
- pinworms - at night, helminths crawl into the vagina;
- childhood diathesis.
During pregnancy, vulvovaginal candidiasis is often diagnosed. In the first trimester, the mucous membranes of the vagina and vulva are filled with blood and glycogen, and this is a favorable environment for the spread of pathogenic microflora, namely Candida fungi.
Causes of gynecological disease in adolescence and young patients:
- regular use of tight underwear with a high content of synthetic fibers;
- injuries to the vaginal walls during intimacy;
- venereal diseases;
- excessive or insufficient hygiene procedures;
- weakened immunity after influenza, pneumonia, dysbacteriosis.
Source: https://xn--80aadc3bb0afph1dp3h.xn--p1ai/zhenskoe-zdorove/vulvovaginit-u-zhenshhin-i-devochek.html
Prevention of vulvitis
Girls should be taught to properly care for their genitals from birth. Regular washing with non-alkaline compounds, clean linen and proper hygiene of the child after using the toilet can prevent inflammatory and serious infectious diseases of the reproductive system.
The basis of prevention is compliance with three simple rules:
- underwear made from natural materials;
- healthy lifestyle;
- hygiene.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Examination and treatment of children
Diagnosis of vulvovaginitis in girls is quite simple. Doctors first ask parents what symptoms they have noticed in their children. The type of soap used, the nature and duration of the discharge are determined. Experts are interested in which direction sick children wipe their anus and whether they come into contact with infected relatives.
After receiving the necessary information, the babies are examined in the knee-chest position to exclude the presence of a foreign body in the vagina and in the “frog position” in order to take material for research. The smear is taken using a swab soaked in sterile saline solution. When collecting material, specialists do not touch the hymen. After receiving culture results, doctors make a diagnosis.
If, upon examination of the smear taken, normal microflora is detected, the doctor will diagnose the child with “nonspecific vulvovaginitis . In such cases, experts give the following recommendations:
Drug treatment of vulvovaginitis (nonspecific) in girls is prescribed if, following the above tips, a positive result does not appear after 3 weeks. Sick girls are prescribed drugs such as Ampicillin, Cephalexin. Typically, these medications are taken orally for 10–14 days. Sometimes specialists prescribe creams that contain antimicrobial components (sulfanilamide, sulfabenzamide).
Antimicrobial therapy may not be effective. If there is no positive result, the doctor will prescribe estrogen creams (hormone therapy). These products are used for 2-3 weeks.
If fungi of the genus Candida (a mycotic type of disease) are detected in a smear, experts recommend antifungal drugs in the form of ointments or creams (for example, Nystatin). Treatment of viral vulvovaginitis is carried out in the following directions: increasing the body's resistance to the effects of pathogenic factors and inhibiting the vital activity of microorganisms that cause the disease. For this purpose, antiviral drugs (Acyclovir, etc.) are used. Treatment of trichomonas vulvovaginitis involves the use of medications such as Metronidazole, Trichopolum.
Possible complications and danger of the disease
Untimely or improper treatment of vulvitis/vulvovaginitis can cause the disease to become chronic. It is characterized by periodic exacerbations, difficulty in therapy, and hypertrophy of the sebaceous glands may occur. Girls may experience synechiae, which sometimes requires surgical intervention.
Vulvovaginitis can cause diseases of the urinary system, cervix, pelvic organs - adnexitis, endometritis, etc., as well as associated infertility.
Diagnosis is carried out by a gynecologist as follows:
- Inspection;
- Collection of complaints, medical history;
- Colposcopy (if necessary);
- Lab tests.
To determine which microorganisms provoked the pathological process, bacterioscopy of smears is performed, as well as cultural inoculation with determination of sensitivity to antibiotics. It is also important to identify concomitant diseases that may cause inflammation or affect the body's defense mechanisms.
Treatment of vulvitis in women involves an integrated approach and the use of systemic and local therapy. It is important to exclude irritating factors and causes of inflammation simultaneously with measures to eliminate inflammation of the external genitalia.
Treatment of vulvitis in a girl involves bed rest. For adult patients, this is not necessary if they feel relatively well.
The doctor selects medications based on test results:
- Antibacterial;
- Antifungal;
- Antiviral, immunomodulatory, etc.
Not only the type of bacterial pathogen is taken into account, but also sensitivity to antibiotics. This allows you to choose effective treatment. If there is a candidiasis form of the disease, antifungal agents are prescribed. In case of chronic recurrent vulvitis, the patient may be recommended additional treatment: taking vitamins, restoratives, immunomodulators.
Specific vulvitis (gonorrheal, chlamydial, etc.) require a special approach. Diseases caused by the proliferation of opportunistic flora can be treated using local remedies.
Local therapy also acts as an addition to the main systemic treatment. It allows you to quickly relieve painful symptoms and increase the effectiveness of the course, speeding up recovery. The genitals can be treated using solutions and antiseptics prescribed by a doctor, baths, compresses, and douching. Vaginal tablets and suppositories are widely used. Even in cases where only the vulva is inflamed and the vaginal mucosa is not involved, suppositories will be an effective way to prevent infection.
If vulvitis is caused by an allergic reaction, antihistamines are used; in cases where it is the result of mechanical damage to tissue, the doctor may recommend regenerating, reparative agents. Normalization of hormonal levels and metabolic processes is a prerequisite for recovery.
You can get help from a qualified gynecologist: contact the Family Doctor clinic, experienced specialists will help in solving a delicate disease. The modern equipment of the gynecology department will allow you to undergo a range of necessary examinations, and an experienced specialist will prescribe effective treatment.
Consultations and appointments at the clinic are carried out by appointment. We work on weekends and holidays. Make an appointment by calling the contact center, through the on-line registration form and at the clinic reception. Cost obstetrician-gynecologist, ultrasound diagnostics doctor, leading specialist of the clinic obstetrician-gynecologist, ultrasound diagnostics doctor obstetrician-gynecologist, ultrasound diagnostics doctor obstetrician-gynecologist, ultrasound diagnostics doctor obstetrician-gynecologist, ultrasound diagnostics doctor, leading specialist of the clinic doctor obstetrician-gynecologist, ultrasound diagnostics doctor, leading specialist of the clinic obstetrician-gynecologist, ultrasound diagnostics doctor obstetrician-gynecologist, gynecologist-endocrinologist, ultrasound diagnostics doctor, candidate of medical sciences, leading clinic specialist obstetrician-gynecologist, ultrasound diagnostics doctor obstetrician-gynecologist, ultrasound diagnostics doctor, obstetrician-gynecologist, ultrasound diagnostics doctor, obstetrician-gynecologist, ultrasound diagnostics doctor, obstetrician-gynecologist, ultrasound diagnostics doctor, obstetrician-gynecologist, ultrasound diagnostics doctor
Causes of vulvitis
Most often, the causative agents of the disease are opportunistic bacteria, which in a healthy body do not cause any negative symptoms. At the same time, infections transmitted through sexual contact and, in rare cases, mycobacterium tuberculosis can provoke the development of inflammation.
However, for the development of the inflammatory process, the presence of predisposing factors is necessary. These include a decrease in the body's immune defense and damage to the mucous membrane of the external genitalia.
1. Very often vulvitis develops against the background of colpitis or vaginitis. At the same time, the pathological process can result from trauma to the vulva, poor intimate hygiene, endocrine disorders, genital and extragenital pathologies. Urinary tract infections (UTIs) and intestinal dysbiosis can also provoke the development of the disease. frequent acute respiratory infections, sore throats. childhood infectious diseases, helminth infections, urinary incontinence, hepatitis with jaundice and various skin pathologies.
2. In girls, the development of vulvitis can be caused by mechanical, thermal and chemical factors, as well as the penetration of foreign objects into the vagina. In older women, the disease is often a consequence of cystitis or diabetes.
3. Itching of the vulva can be provoked by a scabies mite or a pubic louse (in this case, against the background of the disease, severe itching in the pubic area develops, and vulvitis itself is an allergic reaction to parasite bites).
4. Another cause of vulvitis is seborrheic dermatitis of the external genitalia. This is a rather rare disease of unknown etiology, during the development of which inflammatory foci appear on the skin and mucous membranes, varying in color intensity, covered with thin, easily removable crusts.
5. Hidradenitis suppurativa can also provoke the development of the disease. This is a chronic infectious skin lesion, which is characterized by a long, persistent course. Patients suffering from this pathology experience unpleasant-smelling discharge that corrodes the skin and mucous membranes and leads to the formation of painful scars.
6. And finally, psoriasis (skin pathology of unknown etiology) can cause vulvitis.
Symptoms of vulvitis
- redness and swelling of the external genitalia
- sores
- erosion
- burning, itching
- pain when walking, during sex, touching, urinating
- leucorrhoea (color depends on the causative agent of the disease)
You should not allow the infection to start, otherwise it can become severe, completely excluding you from the usual course of life. A severe form of vulvitis is accompanied by fever and enlarged lymph nodes in the groin. At the same time, the woman is forced to remain in bed, because any movement begins to cause pain.