Cystocele - main symptoms:
- Lower back pain
- Lower abdominal pain
- Urinary incontinence
- Pain during sexual intercourse
- Feeling of incomplete bowel movement after bowel movement
- Painful periods
- Violation of the process of defecation
- Prolapse of the uterus from the vagina
- Increasing the duration of the menstrual cycle
- Haemorrhoids
- Bladder stones
- Inflammation in the bladder
- Stagnation of urine
What is a cystocele
A cystocele is a hernia of the bladder in which it protrudes into the vaginal cavity. In most cases, the accompanying deviation is prolapse of the urethra. This disease most often occurs in women after 40 years of age. The disease is secondary, it is preceded by a violation of the elasticity of the muscles and ligaments of the pelvic floor, which leads to the formation of a hernia.
- Etiology
- Symptoms
- Diagnostics
- Treatment
- Possible complications
- Prevention
Pathology is diagnosed after examination by a specialist and additional research: blood and urine tests, and ultrasound diagnostics.
Treatment of cystocele will depend on the degree of the disease: conservative therapy is used for the first and second degrees, and the third degree is treated surgically.
Causes of the disease
This pathology occurs due to a violation of the functional characteristics of the muscles and ligaments of the pelvic floor.
Factors contributing to this pathological process are the following:
- excess body weight;
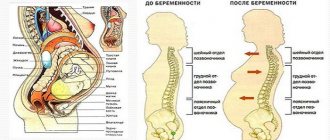
- complications during childbirth;
- disturbance in the location of the pelvic bones after childbirth;
- the child was born with a large weight;
- age characteristics;
- heavy physical work, when the main weight falls on the abdominal muscles;
- genetic predisposition;
- disturbances in intestinal function;
- heavy sports involving lifting dumbbells;
- varicose veins of the small pelvis;
- degenerative changes in connective tissue.
Women who have had their uterus removed are at risk. The likelihood of a hernia occurring in women after a cesarean section is much lower than after an independent birth.
In men, a hernia of the bladder is not so common and occurs against the background of prostate adenoma or due to flabbiness of the abdominal muscles, which leads to infringement of internal organs and their displacement. Over time, the hernia enlarges and protrudes through the abdominal wall.
Normal and cystocele
Causes of rectocele
The reasons for the development of this disease are:
Surgeon
- Multiple pregnancy, frequent and difficult labor, polyhydramnios.
- Heavy physical activity, repeated regularly.
- Prolonged increase in intra-abdominal pressure (constipation, paroxysmal cough).
- Chronic gynecological, proctological diseases.
- Natural age-related weakening of the pelvic floor and perineal muscles.
- Congenital pathology or genetic predisposition.
When answering the question of what rectocele is, it should be remembered that women with a history of more than three births are at risk. Also, a high risk of development occurs in persons with obesity of 3-4 degrees, with low physical activity.
Symptoms of the disease
Cystocele is associated with a disruption and shift in the bladder when the organ is not positioned correctly. The disease may be accompanied by uterine prolapse (ureterocele) and rectal prolapse (rectocele).
There are main degrees of cystocele:
- 1st degree – is the most favorable, when the bladder descends with significant straining. Symptomatically manifests itself in pain in the lower abdomen or lower back, there is painful sexual intercourse, increased pain during menstruation, prolonged menstruation.
- 2nd degree – at rest there is prolapse of the vaginal wall. Symptoms: frequent occurrence of urolithiasis, cystitis, pyelonephritis, stagnation of urine is observed, and urinary incontinence may occur.
- Grade 3 is the most severe, when the vaginal wall is located outside of it. Symptomatically, this manifests itself in constant injury to the uterus when walking, since its walls come out, which leads to poor circulation, tissues can swell and become inflamed, and bedsores may appear.
Rectocele is accompanied by problems with defecation, there is a feeling of incomplete bowel movement, and the frequency of the urge to defecate increases. Against this background, infectious inflammation may develop. If this disease is not treated, the patient's condition may worsen and lead to chronic hemorrhoids and rectal fistula.
Cystocele
Prolapse and prolapse of the pelvic organs in women (cystocele, rectocele, etc.) “Pelvic organ prolapse (pelvic organ prolapse): prolapse of the bladder (cystocele), prolapse of the rectum (rectocele), prolapse and prolapse of the uterus, prolapse vagina, prolapse of the vaginal walls" One of the most frequently diagnosed diagnoses in antenatal clinics and gynecological hospitals. In Russia, uterine prolapse and prolapse of the vaginal walls are observed in 15-30% of women, and over the age of 50 years, the frequency of prolapse increases to 40%. Among elderly and senile women, the frequency of genital prolapse reaches 50-60%.
Patients suffering from prolapse of the pelvic organs (cystocele, rectocele, prolapse of the vagina and vaginal walls, uterine prolapse) most often complain of a noticeable anatomical defect, as well as aching pain/feeling of heaviness in the lower abdomen, a feeling of a foreign body in the vagina, urination disorders ( urinary incontinence, difficulty emptying the bladder) and defecation (constipation, gas incontinence), sexual dysfunction, vaginal discharge.
Classification of pelvic organ prolapse (pelvic organ prolapse) (ICS-1996, POP-Q):
- Stage 1 – The most prolapsing point of the vagina is more than 1 cm above the level of the hymenal ring (entrance to the vagina)
- Stage 2 – The most prolapsing point of the vagina is less than 1 cm above and less than 1 cm below the level of the hymenal ring
- Stage 3 – The vagina prolapses, but not completely (at least 2 cm of its length remains inside)
- Stage 4 – The vagina falls out completely
The most common types of pelvic organ prolapse are:
- cystocele (prolapse of the bladder and prolapse of the anterior vaginal wall),
- rectocele (prolapse of the rectum and prolapse of the posterior vaginal wall),
- uterocele.
Among the factors contributing to the development of pelvic organ prolapse (cystocele, rectocele, vaginal prolapse and uterine prolapse), the following are traditionally identified:
- traumatic and long labor,
- systemic dysplasia (insufficiency) of connective tissue,
- estrogen deficiency (decrease in general and local levels of female sex hormones),
- chronic diseases accompanied by increased intra-abdominal pressure (bronchitis, asthma, constipation, etc.),
- disruption of blood and lymph microcirculation processes in the pelvis,
- obesity,
- A sedentary lifestyle can also be a factor in the development of uterine prolapse (uterine prolapse), rectocele or cystocele.
In recent years, increasing importance has been attached to systemic “connective tissue dysplasia” in patients suffering from pelvic organ prolapse: cystocele, rectocele, uterine prolapse. Prolapse of the bladder (cystocele), rectum (rectocele) and prolapse/prolapse of the uterus (uterocele) are essentially hernias of the abdominal fundus.
A hernia is a protrusion (extension) of the contents of the abdominal cavity beyond its limits in the presence of membranes (for example, peritoneum) in this protrusion. The abdominal cavity (belly) is a closed container containing a large number of organs tightly adjacent to each other. The pressure in the abdomen is constantly changing - from almost zero values (lying at rest) to 200 cm of water column (when coughing, sneezing, laughing, straining, lifting heavy objects)! This pressure has nowhere to go - it spreads to the walls of the abdominal cavity. There are four of them: upper (diaphragm), lower (pelvic floor, vagina), anterior (anterior abdominal wall) and posterior (posterior abdominal wall). The back wall of the abdomen, where the spine and ribs are located, is rigid and cannot be deformed by changes in pressure. The remaining walls of the abdomen consist of soft tissues and one way or another change their configuration during pressure surges in the abdominal cavity. The “load-bearing structures” in all abdominal walls are fascia (connective tissue films) and, to a somewhat lesser extent, muscles. The latter perform mainly motor and “supporting” functions. The entire abdominal cavity is surrounded by the so-called “intra-abdominal fascia” or f. endoabdominalis (in the pelvic floor this fascia is called “intrapelvic” - f. endopelvicalis). In most areas of the abdominal wall, this fascia is “protected” from the outside by powerful muscle-connective tissue formations - the oblique and rectus abdominis muscles, the levator ani muscle, etc. But there are so-called “weak spots” of the abdominal wall, where f. endoabdominalis is forced almost “alone” to resist intra-abdominal pressure. One of these places in the anterior wall of the abdomen is the inguinal canal, where the well-known inguinal hernias are formed.
The vagina, like the anterior abdominal wall, is located on the border between the abdominal organs and the environment. The only difference is that the vagina is a component of the bottom of the abdominal cavity or pelvic floor. The anterior and posterior walls of the vagina are separated from the bladder and rectum only by layers of the intrapelvic fascia. If it is defective, the bladder and/or rectum begin to “fall” into the vaginal lumen - hernias of the vaginal walls are formed. The uterus is held in its anatomical position mainly by the so-called “uterosacral” and “cardinal” ligaments, which are actually thickened sections of the same intrapelvic fascia. Damage to these “ligaments” leads to the fact that the uterus “sinks” into the vagina - a hernia of the “dome (apex) of the vagina” is formed.
Thus, prolapses (prolapses) of the pelvic organs (cystocele, rectocele, uterine prolapse, uterine prolapse) are typical hernias of the abdominal cavity (pelvic floor).
Since ancient times, surgeons have been engaged in plastic closure of defects of the anterior abdominal wall due to hernias, using the patient’s own tissue. But, despite the most sophisticated suturing methods, the results were far from reassuring - up to 60% of patients returned with a recurrence of the hernia. In the early to mid-80s, a revolution occurred in hernia surgery - the concept of “tension-free hernioplasty” using mesh endoprostheses made of monofilament polypropylene was proposed. The use of seemingly simple “grids” led to completely immodest results. In particular, the frequency of relapses after surgical treatment of inguinal hernias decreased from 15-20% to 0.1-0.5%!
Only a decade later (in 1995) “synthetics” came into surgery for urinary incontinence in women. And again there was a revolution! But this time - in urogynecology. TVT (Tension-free Vaginal Tape) technology has appeared - “tension-free vaginal tape.” The use of TVT has revolutionized the way doctors and patients think about the surgical treatment of stress urinary incontinence. Now the operation lasting 20-30 minutes under local anesthesia ensured almost 90% success in the long-term follow-up period.
The amazing success of TVT has inspired urogynecologists to use polypropylene meshes in the surgical treatment of prolapse and prolapse of the uterus and other pelvic organs. At first it was simply “strengthening” the sutures with a mesh after traditional anterior colporrhaphy, then a “posterior” sling appeared, which made it possible to very effectively combat uterine prolapse.
The indication for surgical treatment using synthetic mesh prostheses is prolapse of the pelvic organs (cystocele, rectocele, uterine prolapse, uterine prolapse) stage III - IV.
Traditional surgical interventions for SEVERE forms of cystocele, rectocele or uterine prolapse, involving plastic surgery with one’s own tissues (without the use of “meshes”), cannot currently be considered the optimal choice
The reason is an extremely high risk of relapse (at least 30-50%) with a fairly large number of complications (sexual dysfunction, pain, etc.). Unfortunately, in Russia and the CIS, anterior and posterior colporrhaphy, colpoperineolevatoroplasty, etc. still remain the main operations performed for cystocele and rectocele. And hysterectomy (removal of the uterus) is often used for “treatment,” which in most cases is completely unjustified and even harmful.
Vaginal surgeries involving the use of endoprostheses are usually performed under regional anesthesia. There are practically no cosmetic defects left after the operation (all incisions are in the vagina). In the vast majority of cases, the operations are easily tolerated, and the patient goes home on her own within 2-3 days. You can begin normal physical activity 2-3 weeks after surgery.
The use of synthetic implants in young, sexually active patients is currently the subject of lively discussion among specialists. There are both supporters and opponents of this approach. Currently, clinical experience is being accumulated in implanting “mesh” via vaginal access in such patients. New endoprostheses and surgical techniques are being explored.
And finally, a word in defense of traditional operations. Correctly performed reconstructive operations using one's own tissues in correctly selected patients provide excellent results! In a number of cases, it is possible to successfully combine the use of meshes and traditional plastic surgery.
THE MOST IMPORTANT THING for the patient:
Pelvic floor reconstructive surgery is a very specialized field that requires a thorough understanding of the anatomy and function of the pelvic organs, as well as proficiency in both “mesh” and “traditional” procedures. Knowledge makes the doctor free to choose a treatment method, and the patient happy with the results.
Diagnostics
The diagnosis of cystocele is made after examination in a gynecological chair, and additional straining of the abdomen may be required for vaginal displacement to appear.
The specialist prescribes additional studies to confirm the extent of the disease and exclude the development of an inflammatory process.
Laboratory research:
- a general urine and blood test is taken;
- stool analysis may be required;
- vaginal smear.
Instrumental diagnostics includes:
- performing an ultrasound examination of the bladder and uterus;
- uroflowmetry is prescribed;
- Cystoscopy is performed if concomitant pathological processes are suspected - neoplasms in the bladder, cystitis;
- Additionally, rectal or radiological examinations of the intestine may be performed.
Cystoscopy
After the entire complex of research activities, the diagnosis is confirmed and the degree of pathology is established. Treatment is prescribed, and in severe cases surgery will be performed.
Treatment
The first and second degrees of the disease do not require surgical intervention.
In this case, the patient should follow the following clinical recommendations:
- do not lift heavy weights - permissible weight is 3 kilograms;
- underwear should not squeeze or cause discomfort;
- maintain genital hygiene, soap should be hypoallergenic;
- if vaginal dryness is observed, it is necessary to moisturize it with linseed or olive oil;
- You should wear special pads for urinary incontinence.
Cystocele treatment is carried out only using complex measures and will depend on symptomatic manifestations:
- if estrogen deficiency is detected, hormone therapy is prescribed;
- a diet is prescribed, and the diet should contain a large amount of plant fiber to improve intestinal motility;
- for concomitant urolithiasis, painkillers, antimicrobials and agents that help remove sand from the bladder are prescribed.
The patient may be prescribed to wear a pessary - this is a special device that is inserted transvaginally and helps normalize the position of the uterus and vaginal walls. With the help of this device, the urethra returns to its place, preventing spontaneous urination.
To prevent the vaginal ring from causing itching or inflammation, patients are recommended to irrigate the vagina with decoctions of calendula, chamomile, and plantain.
Surgical intervention is prescribed at the third stage of the disease and is carried out through transvaginal access. In case of vaginal prolapse, autoplasty is performed, with the help of which the ligamentous apparatus of the uterus is tightened. But this procedure is temporary, since relapse is possible as the disease progresses.
Reconstructive intervention can be undertaken when a special mesh is implanted, which will perform a supporting function. This method is the most effective for stage 3 cystocele.
Another method is laser therapy, which is used in the first stages, but has a lot of contraindications.
After cystocele surgery, the patient will undergo rehabilitation. During this time, you should not lift heavy objects or perform sudden movements. Anti-inflammatory drugs may be prescribed. The patient must observe the rules of personal hygiene and periodically visit the gynecologist to monitor her condition.
Treatment of cystocele
Treatment depends on how severe the disease is and what associated problems are present (for example, uterine prolapse).
In mild cases, where there are no or mild symptoms, treatment may not be required at all. It is enough to observe and perform special exercises (Kegel technique) to strengthen the pelvic floor muscles. If these measures are ineffective, American doctors recommend the following options:
Vaginal pessaries. These are plastic or rubber products that are inserted into the vagina and help support the bladder. The doctor will select the product of the size you need and teach you how to use it correctly. Vaginal pessaries in the United States are recommended for women who wish to delay surgery or for whom surgery is not desirable. . Estrogen therapy. Your doctor may prescribe medications that contain the female sex hormone (estrogen), usually in the form of a vaginal cream or suppository. This treatment is suitable for women after menopause. Estrogen helps maintain pelvic muscle tone.
If conservative treatment does not help, and the symptoms of a cystocele greatly affect the woman’s quality of life, then surgical treatment may be required. During this operation, the surgeon returns the prolapsed organs to their place and removes excess tissue by “tightening” the supporting muscles. If a cystocele is combined with uterine prolapse, your doctor may recommend removing the uterus (hysterectomy).
If you are planning to become pregnant, you should postpone surgery. The use of vaginal pessaries helps relieve symptoms for a certain period of time. The effect of surgery for cystocele is not long-lasting—symptoms of the disease may return several years after surgery, requiring repeated surgery.
What to do?
If you think you have a Cystocele
and symptoms characteristic of this disease, then a gynecologist can help you.
We wish everyone good health!
Diseases with similar symptoms
Endometriosis (overlapping symptoms: 4 of 13)
Endometriosis is a gynecological non-tumor disease, accompanied by the growth of the inner lining of the uterus (endometrium) outside its cavity. Simply put, tissue that is found in the uterus of healthy women with endometriosis grows in other organs. Endometriosis, the symptoms of which women experience, develops for unknown reasons, although there is some evidence for the identification of immune, hormonal, hereditary and some other factors.
Did you like the article? Share with friends on social networks: