Kinds
Acute paraproctitis, depending on the location of its localization, is of 3 types:
- Subcutaneous - located directly at the anus.
- Acute ischiorectal paraproctitis - is located in an area limited by the bones and gluteal muscles, and does not affect other tissues except the pelvic floor.
- Submucosal - localized inside the rectum near the anus.
Treatment of paraproctitis with folk remedies
Although traditional methods of treatment often cause laughter, they allow you to actively fight paraproctitis. There are several useful substances that relieve symptoms of the inflammatory process:
1.
Mumiyo . For one basin of water you need to take 10 tablets. Dissolve them in a glass and pour the contents into 5 liters of warm water. We sit in the bath for at least 15 minutes. You need to do the procedure every day.
2. Badger fat . It is worth preparing small tampons, soaking them in fat and inserting them into the anus overnight. Don't be afraid to overexpose the product. It does not cause side effects.
3. Rowan. Fresh juice should be taken before each meal. And compresses from the same juice should be applied to the anus. You can do them at night so that you have time to lie down quietly.
4. St. John's wort. An effective remedy for ulcers. You need to throw 3 tablespoons of St. John's wort into boiling water. It cooks for about 15 minutes. Place the hot grass remaining after straining on a vertical surface and cover it with cellophane or a thin cloth. Then we sit on top. The procedure lasts until the grass cools down. After some time, the pus will come out safely.
Symptoms
Acute purulent paraproctitis is characterized by the following symptoms:
- Increased body temperature.
- Weakness, chills.
- Pain in the rectal area, radiating to the perineum or pelvis.
- Decreased appetite.
- The presence of compactions and redness in the anus.
- Inconsistency in buttock size.
- Irritation and redness around the anus.
Symptoms depend on the location of the source of infection and the bacteria that caused it.
If the abscess is located closer to the skin, the disease has clear symptoms and is easy to diagnose.
It is most difficult with deep abscesses, the removal of which requires complex operations.
Paraproctitis
Symptoms
There are acute and chronic paraproctitis.
The etiopathogenetic mechanisms are the same, but the clinical picture of these two types of course differs significantly. Acute paraproctitis, as follows from the definition, develops quickly (within 1-3 days), rapidly, and sometimes catastrophically. Characterized by intense pain in the perianal area, which, as it suppurates, becomes pulsating and can radiate to the perineum, lower abdomen, etc. There is a general malaise with a tendency to constant deterioration; The symptoms may initially resemble the clinical picture of acute respiratory viral infection or other similar intoxication (headache, weakness, feverish chills, high body temperature, joint and muscle aches, etc.). The acts of urination and especially defecation (which is sometimes accompanied by purulent discharge) are excruciatingly painful. With subcutaneous acute paraproctitis, pathological changes in the perianal tissues are noticeable to the naked eye: hyperemia, severe pain, extensive swelling up to asymmetry of the buttocks. In general, the possible variants of clinical manifestations are very diverse and depend on a number of factors, primarily on the localization of the phlegmonous process in this particular case; Based on the number of perirectal tissue spaces, four clinical forms of acute paraproctitis are distinguished, as well as a mixed form. Spontaneous opening of abscesses brings only temporary relief, in fact exacerbating the situation. Purulent melting (this well-established term is very accurate) literally burns fistulous tracts in the tissue with exits into the rectum, sphincters, in women into the vagina, in men into the scrotum, but more often through the skin into the outer space. Fistulas may not have an outlet, but extend from the affected crypt into the intestinal wall or other structure. When pus is released into the abdominal cavity, diffuse peritonitis is almost guaranteed.
Chronic paraproctitis, as a rule, is a direct result of self-medication, inaction (in the desperate hope that “it will hurt and stop”), irrational fears before a visit to the proctologist (which up to a certain point can suppress even the instinct of self-preservation) and, in the future, non-compliance medical orders. For chronic paraproctitis, a non-healing fistula (or several such passages) is typical, which becomes a source of severe hygienic, aesthetic and psychological problems, caused, among other things, by the spontaneous release of intestinal gases and feces through the fistula canal. If the sphincter “rings” are damaged, encopresis proper (fecal incontinence, incontinence) is also possible. Characteristic is the alternation of remissions and exacerbations, which are provoked by even minor trauma, weakened immunity, blockage of the fistula duct for one reason or another; the clinic of such relapses is generally similar to acute paraproctitis. Over a long period of time, fibrosis (scarring) and “smoldering” inflammation can force the appearance of atypical cells and the start of a malignant oncological process. In general, a high probability of malignancy is inherent in almost all proctological diseases.
Diagnostics
Most often, diagnosing paraproctitis is quite simple. The pathology is treated by a proctologist.
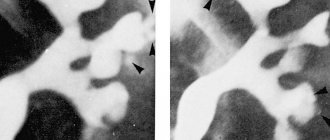
In order to make a diagnosis, in most cases it is sufficient to interview the patient, visual examination and palpation, during which the doctor can detect an infiltrate of dense consistency. In addition, there is thickening of the intestinal walls, their soreness and swelling.
It is most difficult to diagnose paraproctitis with ulcers that form deep in the pelvis. In this case, additional instrumental studies of the intestine are required.
With paraproctitis, changes can also be noticed in laboratory tests, where an increase in leukocytes and an acceleration of ESR are noted.
Prevention of the disease and prevention of relapse
Despite the seriousness of paraproctitis, preventive measures to prevent it are not difficult.
- It is necessary to undergo regular examinations by a proctologist and promptly treat diseases of the rectum.
- Avoid chronic diseases such as diabetes, colitis, and also check for helminthic infestations.
- For people suffering from gastrointestinal disorders, a certain diet is required, that is, to normalize the diet.
- It is necessary to strengthen the immune system, avoid overcooling and observe the rules of personal hygiene.
Paraproctitis is a rather delicate disease and this is what causes people to turn to a specialist late. However, it is necessary to remember and understand that without the intervention of doctors, the disease will not disappear.
A proctologist with extensive experience will tell you about the signs and symptoms of a form of acute paraproctitis in a short video:
Useful tips for treating paraproctitis using non-drug methods can be found in the video:
Causes
Paraproctitis can occur in absolutely any person. In order for an abscess to appear, it is enough to have an inflammatory process in the body. Self-infection through blood occurs quite often with this pathology.
However, in most cases, paraproctitis appears against the background of hemorrhoids and anal fissures . These diseases increase the risk of infection.
Risk factors also include people suffering from diabetes, atherosclerosis, and immunodeficiency.
Failure to comply with hygiene rules, injuries to the rectal area, anal sex and the presence of inflammatory bowel processes can cause paraproctitis.
Causes of acute paraproctitis
As mentioned above, the main cause of this disease is an infection that enters the cellular space from the surface of the rectal mucosa. The causative agents of the infection are representatives of mixed flora, namely streptococci, staphylococci and E. coli. In extremely rare cases (1-2% of patients), infection can occur due to the addition of a specific infection: tuberculosis, clostridia or actinomycosis.
Bacteria can be very different, but the result of their impact on the body is the same - the development of a disease
The entrance gates are any wounds, microscopic injuries or scars formed after operations on the mucous membrane.
In addition, there is another route of infection – internal. It includes various chronic human infections, as well as processes such as sinusitis and caries. The causative agents of these diseases follow from the epicenter of inflammation and are transferred with the flow of blood and lymph to the tissues of the rectum.
Predisposing factors
The development of the disease can also be facilitated by poor nutrition, prolonged bed rest of the patient, and the presence of one or more chronic diseases. Additional aspects that increase the risk of paraproctitis include:
- weak immunity;
- atherosclerosis;
- diabetes;
- anal fissures;
- unprotected anal intercourse.
In rare cases, if the disease is started, inflammation can cover not one, but several layers of tissue at once and reach the border with the intestines.
Treatment methods
Currently, treatment is carried out surgically or conservatively.
However, it is impossible to cure an acute inflammatory process with medications . In the best case, it is possible to stop the infection and relieve inflammation, which is not a reason to refuse surgery.
Only if the abscess is located close to the skin and the pus breaks out is self-healing possible, which is extremely rare.
Surgery for acute paraproctitis is aimed at removing the source of infection with further pumping out the pus. In addition, excision of fistulas and passages through which the infection has penetrated is performed. Without these manipulations, ulcers may appear again.
Surgery is performed under general anesthesia.
Treatment after surgery involves:
- Carrying out dressings.
- The use of general strengthening drugs.
- Antibiotic therapy.
- Disinfection of the wound.
- Careful hygiene.
Treatment at home after surgery involves the use of antibacterial baths based on chamomile, calendula, sage and oak bark after each bowel movement. Antibiotics may be prescribed. It usually takes 3 to 4 weeks for the wound to heal completely.
Diet and nutrition
During treatment, a person must adhere to a diet aimed at preventing constipation:
- Food should be consumed often, but in small portions.
- High-calorie, fatty, smoked and salty foods should be avoided.
- The diet should be dominated by vegetables, fruits, fermented milk products, and lean meats.
- Alcohol and coffee are contraindicated.
Complications of paraproctitis
People who self-medicate may suddenly feel better:
- temperature normalizes;
- pain decreases or disappears completely.
However, this apparent relief takes the disease to a new, more dangerous stage. A man or woman discovers the beginning of profuse purulent discharge from the rectum. At the same time, female paraproctitis is also characterized by bloody-purulent discharge from the vagina. These manifestations are observed after the abscess breaks through after the wall of a nearby organ dissolves.
At such moments, you do not need to do anything yourself, as urgent medical attention is required.
It must be remembered that the fistula will not heal without a course of therapeutic treatment.
Causes of the disease
Inflammation in the perirectal tissue is a consequence of the penetration of various bacteria. Most often these are staphylococcus, gram-negative and gram-positive rods. In some cases it may be a mixed microflora. Sometimes the cause of paraproctitis is anaerobes, mycobacterium tuberculosis or treponema pallidum.
Factors contributing to the development of the disease:
- traumatic damage to the anal canal mucosa;
- chronic hemorrhoids;
- inflammation of the glands, the mouths of which are located in the anal crypts;
- chronic diseases of the large intestine: Crohn's disease, ulcerative colitis;
- inflammatory diseases of neighboring organs: prostate, urethra, uterus, appendages;
- decreased immunity.
Drug treatment
The solution to the question of how to treat paraproctitis almost always comes down to surgical intervention. The operation can be performed under intravenous anesthesia or using mask anesthesia. Radical surgery involves opening the formed abscess, draining its cavity and blocking the passage through which the infection can spread to deeper layers of tissue. Only in this case can the patient count on a complete recovery.
But, as practice shows, radical surgery is performed infrequently, since very few specialists have sufficient experience to perform such a procedure. In most cases, surgical intervention is limited to opening and draining the abscess, which leaves the possibility of recurrent infection. With chronic paraproctitis, treatment does not end there. In parallel, antibiotic therapy and physiotherapy are carried out. For 3-4 days after the diet, patients must adhere to a slag-free diet. In the absence of independent stool, it is necessary to give a cleansing enema.
Treatment
Therapy for both acute and chronic paraproctitis involves surgery: opening the abscess or draining it. Before and after surgery, painkillers and antibiotics are prescribed, as well as the use of physiotherapeutic procedures: microwave and ultra-high frequency therapy.
If you ignore the problem, you risk the development of complications: breakthrough of the abscess, formation of phlegmon, pelvioperitonitis, spread of the inflammatory process to the scrotum and urethra.
data-ad-format="auto">
Doctor's review
Paraproctitis is a purulent inflammation of the tissues surrounding the rectum.
Often occurs with the formation of purulent fistulas. The cause of this condition is microbial agents. The presence of any pathology of the rectum increases the likelihood of disease: fissures, hemorrhoids, inflammation of the mucous membrane, constipation, tumors.
A visit to a proctologist will help to exclude pathologies of a tumor nature.
In acute cases, surgical treatment is indicated. Increases the risk of a sedentary lifestyle, the presence of inflammatory diseases, and decreased immunity. Prevention is daily bowel movements, hygiene of the anal area, treatment of inflammatory diseases.
If you have intestinal diseases, an annual visit to a proctologist is mandatory.