Sudden exanthema is an acute infectious disease of young children caused by herpes virus types 6 and 7, occurring with a temperature reaction and skin rashes. With sudden exanthema, febrile temperature appears successively, then a papular rash on the skin of the torso, face and limbs. Specific methods for diagnosing sudden exanthema are PCR detection of HHV-6 and ELISA for IgM and IgG titers. Treatment of sudden exanthema is mainly symptomatic (antipyretics); antiviral drugs may be prescribed.
Sudden exanthema
Sudden exanthema (pseudo-rubella, roseola, three-day fever, sixth disease) is a childhood viral infection characterized by high fever and a spotty rash on the skin. Sudden exanthema affects about 30% of young children (from 6 months to 3 years). In most cases, sudden exanthema develops in a child between 9 months and 1 year of age; less often up to 5 months. It is assumed that the disease is transmitted by airborne droplets and contact. The peak of the spread of infection occurs in autumn and winter; girls and boys get sick equally. Sudden exanthema is experienced by children once, after which those who have recovered develop stable immunity.
Causes of sudden exanthema
The etiological agents causing sudden exanthema are human herpes viruses types 6 and 7 (HHV-6 and HHV-7). Among these two types, HHV6 is more pathogenic and is considered the main causative agent of sudden exanthema; HHV7 acts as a second pathogen (cofactor).
HHV-6 and HHV-7 belong to the family Herpesviridae, genus Roseolovirus. Viruses have the greatest tropism for T-lymphocytes, monocytes, macrophages, astrocytes, arborescent cells, epithelial tissue, etc. Once in the body, pathogens stimulate the production of cytokines (interleukin-1b and tumor necrosis factor-α), react with cellular and circulating immune complexes , causing the appearance of sudden exanthema.
In adolescents and adults, HHV-6 is associated with asymptomatic urinary infection. In addition, reactivation of a virus that latently persists in the central nervous system can cause the development of meningoencephalitis and myelitis. HHV-6 is reported to be the culprit in benign (lymphadenopathy) and malignant (lymphoma) lymphoproliferative diseases. Some authors associate chronic fatigue syndrome with HHV-7.
Chicken pox (B01), herpes zoster (B02)
The varicella zoster virus - herpes zoster - from the group of herpes viruses after a typical infection (varicella) remains in a latent form, becoming activated when immunity decreases (shingles). Transmitted by air. The incubation period is 10-21 (14-16) days, until the 28th day after administration of immunoglobulin.
Drug sensitivity to acyclovir, valacyclavir, famcicovir.
Clinical manifestations. An acute disease with a profuse vesicular rash, it is more severe in adolescents and people receiving corticosteroids and salicylates (including Aspirin - the development of Reye's syndrome), in children with HIV and on immunosuppression - with damage to internal organs and the central nervous system. With herpes zoster, vesicles and pain are localized along the nerve. Scratching can lead to a streptococcal infection, especially when taking ibuprofen.
Treatment of chicken pox. Acyclovir reduces the intensity of the rash only when taken on the 1st day (virus replication lasts 72 hours); its administration to healthy children is not recommended. If there is a threat of a severe course, acyclovir is administered orally: children 0-12 years old 20 mg/kg - max. 800 mg - 4 times a day for 5 days, adolescents 13-18 years old - 800 mg 5 times a day for 10 days. Acyclovir is administered intravenously to persons with immunodeficiency: children 0-3 months. 30-60 mg/kg/day at least 7 days, 3 months-12 years 25-40 mg/kg, 5 days; adolescents 12-18 years old: 15-30 mg/kg/day for 5 days.
For the treatment of herpes zoster, acyclovir is administered intravenously in the same doses for 7-10 days, for milder forms - 800 mg orally 5 times a day for 5-7 days (>12 years).
Newborns are administered intravenous immunoglobulin if the mother has chickenpox before or immediately after childbirth, as well as in contact with a patient with chickenpox, if the mother did not have this infection (with a weight <1000 g, regardless of the mother’s medical history).
Prevention: acyclovir 20-80 mg/kg/day from 7-9 days after contact for 5-14 days prevents or mitigates the manifestations of infection. Protection of contact children with immunosuppression is carried out with acyclovir in combination with the administration of intravenous immunoglobulin.
Vaccination of children with leukemia, like mass vaccination in many countries of the world, is licensed in Russia. Post-exposure vaccination is effective in the first 3-4 days after exposure.
Symptoms of sudden exanthema
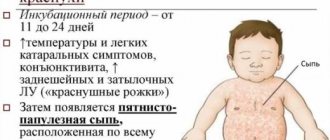
The incubation period for sudden exanthema ranges from 5 to 15 days. The disease begins with a sudden increase in body temperature to high values (39-40.5°C). The period of fever lasts for 3 days, accompanied by severe intoxication syndrome (weakness, apathy, lack of appetite, nausea).
Hemorrhoids kill the patient in 79% of cases
It is characteristic that with sudden exanthema, despite such a high temperature, in most cases there are no catarrhal symptoms (runny nose, cough). Relatively rarely, younger children experience diarrhea, nasal congestion, enlarged cervical lymph nodes, swelling of the eyelids, hyperemia of the pharynx, and a small rash on the soft palate and uvula. In infants, pulsation of the fontanel is sometimes observed.
Body temperature decreases slightly in the morning; While taking antipyretics, children feel satisfactory. Since sudden exanthema coincides with teething, parents often explain the increased temperature precisely by this fact. Sometimes, with a sharp increase in temperature to 40°C and above, febrile convulsions develop: with sudden exanthema, they occur in 5-35% of children aged 18 months to 3 years. Febrile seizures are usually not dangerous and go away on their own; they are not associated with damage to the nervous system.
A critical decrease in temperature with sudden exanthema occurs on the 4th day. Normalizing the temperature creates a false impression that the child has completely recovered, but almost simultaneously, a pinpoint or small-spotted pink rash appears all over the body. The rash first appears on the back and abdomen, then quickly spreads to the chest, face and limbs. Elements of the rash with sudden exanthema are roseolous, macular or maculopapular in nature; pink color, diameter up to 1-5 mm; when pressed they turn pale, do not tend to merge and do not itch. The rash that accompanies sudden exanthema is not contagious. During the period of rashes, the child’s general well-being does not suffer. Skin manifestations disappear without a trace after 2-4 days. In some cases, sudden exanthema may occur without a rash, only with a febrile period.
Complications from sudden exanthema develop quite rarely and, mainly, in children with reduced immunity. Cases of the development of acute myocarditis, meningoencephalitis, cranial polyneuritis, reactive hepatitis, intussusception, and post-infectious asthenia have been described. It has been noted that after suffering a sudden exanthema, children may experience accelerated growth of adenoids and frequent colds.
Features of viral exanthema in children
Viral exanthema in children is a disease characterized by rashes that appear on the child’s skin and evenly cover the entire body. It occurs frequently both in babies of the first year of life and in older children.
Causes of viral exanthema:
- measles virus;
- herpes virus;
- adenovirus;
- chickenpox, etc.
As a rule, the symptoms of exanthema are the same, with the exception of cases of measles or chickenpox. During the course of these diseases, exanthema manifests itself specifically. In this case, complex therapy is used, which is aimed at getting rid of not only the disease, but also exanthema.
Exanthema of the viral and allergic types are similar in symptoms, so it is very important to recognize in time which pathology a specific type of rash on a baby’s skin belongs to (we recommend reading: how is a viral rash on a child’s body treated?). Improper treatment of exanthema is fraught with complications.
General clinical picture
Viral exanthema in children is characterized by an increase in temperature, which usually lasts for 4-5 days. The rash at this time may become more intense under the influence of various factors: bright sunlight, hot water, emotional stress, etc. It is important to protect the child from such phenomena so as not to aggravate the situation.
With viral exanthema, in addition to skin rashes, the child’s temperature rises
In newborns, the pulsation of the fontanel may become more frequent. Exanthema, which occurs against the background of infection, is accompanied by an increase in regional lymph nodes. It is provoked by the following infections:
- in winter, as a rule, these are rhinovirus diseases, influenza virus and adenoviruses;
- in summer the causative agent is often an enterovirus;
- herpetic infections can be detected at any time of the year (we recommend reading: photo of a herpetic rash on a child’s body).
READ ALSO: Problematic facial skin: causes, treatment
Symptoms depending on the type of virus
Symptoms of viral exanthema in children vary, depending on the type of infection. The main symptoms are presented in the table.
| Virus | Symptoms |
| Enterovirus | A large number of small papules, the rash covers most of the child’s body, and intoxication of the body occurs. |
| Adenovirus | It is characterized by pinkish spots all over the body, itching, and keratoconjunctivitis may be observed. |
| Rubella, rotavirus (we recommend reading: rubella: photo of the rash) | Pink spots on the body, which upon close examination noticeably protrude above the surface of the skin, can merge with each other. |
| Epstein-Barr virus | Rashes on the body resembling symptoms of measles, pharyngitis, swelling of the eyelids. |
| Gianotti-Crosti syndrome | The rash is located asymmetrically, the spots sometimes merge with each other. |
| Parvovirus B-19 | A rash on the child’s cheeks and bridge of the nose is one of the signs. In some cases, the disease occurs hidden. |
Diagnosis of sudden exanthema
Despite its high prevalence, the diagnosis of sudden exanthema is extremely rarely made in a timely manner. This is facilitated by the transience of the disease: while a diagnostic search is underway, the symptoms of infection, as a rule, disappear on their own. However, children with a high fever or rash should definitely be examined by a pediatrician and a pediatric infectious disease specialist.
In the physical examination, the leading role belongs to the study of the elements of the rash. Sudden exanthema is characterized by the presence of small pink spots that disappear with diascopy, as well as papules with a diameter of 1-5 mm. In side lighting, it is noticeable that the elements of the rash rise slightly above the surface of the skin.
A general blood test reveals leukopenia, relative lymphocytosis, eosinopenia, granulocytopenia (sometimes agranulocytosis). The PCR method is used to detect the virus. To determine the active virus in the blood, a culture method is used. In children who have recovered from sudden exanthema, IgG and IgM to HHV-6 and HHV-7 are detected in the blood using ELISA.
In case of complications of sudden exanthema, consultation with a pediatric neurologist, pediatric cardiologist, pediatric gastroenterologist and additional instrumental studies (EEG, ECG, abdominal ultrasound, etc.) are necessary.
In case of sudden exanthema, differential diagnosis should be carried out with fever of unknown etiology, rubella, measles, scarlet fever, erythema infectiosum, enteroviral infections, allergic rash, drug toxicoderma, pneumonia, pyelonephritis, otitis.
Treatment of sudden exanthema
The contagiousness of the virus is not high, however, children with sudden exanthema should be isolated from their peers until other infectious diseases have been ruled out and symptoms disappear.
In the room where the patient with sudden exanthema is located, daily wet cleaning and ventilation are carried out every 30 minutes. During the febrile period, the child should receive plenty of fluids (teas, compotes and fruit drinks). Walks are allowed after the temperature normalizes.
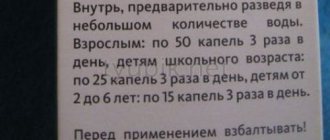
There is no specific treatment for sudden exanthema. If children do not tolerate high fever, antipyretic drugs (paracetamol or ibuprofen) are indicated. As prescribed by the pediatrician, antiviral and antihistamine drugs can be used for sudden exanthema.
Treatment
For a phenomenon such as exanthema, treatment is symptomatic. Therapeutic measures depend on the diagnosis.
Rubella and measles require symptomatic treatment and bed rest. It is extremely important to prevent the addition of secondary infections, which can result in complications such as otitis media, encephalitis, and pneumonia.
Symptomatic treatment for chickenpox is to prevent suppuration; for this purpose, aniline dyes are used to lubricate the elements of the rash.
For herpes zoster, the drug “Acyclovir” is administered; the treatment regimen is selected by the doctor individually and depends on the general condition and age of the child.
To treat ailments that develop when infected with the herpes virus, drugs such as Valaciclovir, Acyclovir, and Pharmciclovir are used.
When infected with paraviruses and enteroviruses, there is no specific therapy. Therefore, treatment consists of relieving the symptoms of the disease and alleviating the patient’s condition.