Content
- What does a mycologist treat?
- In what cases is it necessary to contact a mycologist?
- Consultation stages
- Diagnostics
- Treatment
In most cases, patients with severe disease are referred to a mycologist by dermatologists, therapists or general practitioners.
The professional field of a mycologist includes superficial and deep mycoses, which are caused by molds and yeasts.
Prevention of fungal diseases
During each appointment, the mycologist tells patients simple methods for preventing pathologies of fungal origin, which reduce the risk of being exposed to such diseases:
- Keep clothes and home clean. Regularly organize wet cleaning of premises, especially for people with allergic reactions.
- Adhere to hygiene rules. Avoid prickly skin conditions and diaper rash.
- Do not self-medicate. Having discovered the first symptoms of candidiasis and other fungal diseases, immediately consult a doctor to establish an accurate diagnosis and, if necessary, nip the problem in the bud by receiving professional recommendations and a course of therapy.
- Correct diet. It is very important to eat healthy foods and take enough vitamins, adjusting to the season.
- Keep your hands and feet dry and clean. If you have excessive sweating, see a mycologist or dermatologist.
What does a mycologist treat?
A mycologist treats:
- Actinomycosis is a chronic fungal disease that affects animals and humans. Caused by actinomycete bacteria, which are capable of forming branching mycelium at some stages of their development. The disease is widespread, but is sporadic. In most cases, patients are males living in cities. The disease spreads both exogenously and endogenously (in most cases, bacteria enter the body with plant shells and are activated during inflammatory diseases of the mucous membranes of the oral cavity, gastrointestinal tract and respiratory tract, and skin lesions are secondary). The form of the disease can be deep (intermuscular tissue is affected), subcutaneous and cutaneous. The disease can be acute or become chronic.
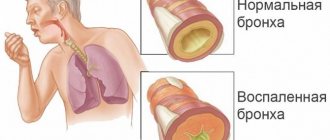
- Fungal pneumonia is an inflammation of the lungs caused by various types of pathogenic and opportunistic fungi. The disease can be either primary (develops when lung tissue is infected) or secondary (develops as a complication of other diseases). Deep mycoses of the lungs develop as a result of colonization by strains of fungi of the mucous membrane of the lower parts of the respiratory tract (a prerequisite is a decrease in immunity). Most often, pneumomycosis develops as a result of infection by Candida, Aspergillus and Pneumocystis fungi, which have a strict tropism for lung tissue. The causative agent can also be fungi of the genus Mucor (white mold), dimorphic fungi of the genus Blastomyces, genus Histoplasma and coccidia (genus Coccidioides), trichomycetes and actinomycetes bacteria that cause pseudomycosis. Fungal pneumonia can be caused by a mixed infection (a combination of different types of fungi) and a combined infection (a combination of fungi and other microorganisms). The clinical picture resembles atypical pneumonia, so the disease is poorly diagnosed, and the mycologist treats the disease in a fairly advanced stage.
- Aspergillosis, which is caused by fungi of the genus Aspergillus. Aspergillus penetrating through the respiratory tract affects internal organs (most often the respiratory system is affected). Against the background of chronic lung pathologies with non-invasive aspergillosis, a spherical formation is formed from the mycelium - aspergilloma, which may not be clinically manifested or may be accompanied by a cough with hemoptysis. Invasive pulmonary aspergillosis occurs in an acute form. When the infectious process spreads to other organs, the disease becomes severe (observed in 30% of patients), and death is possible. The same type of fungi can affect the paranasal sinuses and external auditory canal. Skin lesions are observed in only 5% of patients.
- Onychomycosis is a fungal infection of the nail plates, which in most cases is caused by keratin-eating trichophyton fungi (Trichophyton interdigitale, Trichophyton tonsurans, etc.). The causative agent can also be flocculus (Epidermophyton floccosum) and microsporia (ringworm, which is caused by fungi of the genus Microsporum). Onychomycosis can be normotrophic (the thickness of the nail does not change, the shine remains, but spots and stripes appear on the nail), hypertrophic (the color of the nail is changed, the shine is lost, the nail is thickened and deformed), onycholytic (part of the nail dies and is torn away from the nail bed). Damage to the nail can affect its free edge, both sides, the back cushion and the entire nail.
- Mucormycosis, which is caused by fungi of the genus Zygomycetes. Lesions primarily affect the nose, paranasal sinuses and head, but the lungs and gastrointestinal tract may also be affected. The subcutaneous form of the disease is common in Africa and Southeast Asia, accompanied by the appearance of irregularly shaped nodes under the skin of the chest and neck. The provoking factor for the development of the disease is weakened immunity and concomitant infections. The acute form of the disease progresses rapidly and can be fatal, so the mycologist often treats this disease together with specialists from other fields.
- Trichophytosis is a disease that can have a superficial, chronic and infiltrative-suppurative (zoophilic) form. It affects hair and affects one type of skin (only hairy or only smooth skin), as well as nails in some forms of the disease. Develops when infected with anthropophilic or zoophilic fungi.
- Favus is the collective name for human mycoses, which are accompanied by the formation of a hard crust (scab) on the skin. A hard crust forms in most cases on the scalp, but can also affect any areas of the skin and even mucous membranes. The causative agent of the disease is the fungus T. schoenleinii or T. violaceum. The route of infection is from person to person with household items or (extremely rarely) from animals. A specific element of the favus is the scutula (a pure culture of the fungus, which is located in the stratum corneum of the mouth of the hair follicle and looks like a saucer-shaped bright yellow dry spot).
- Candidiasis is damage to the skin, mucous membranes, nails and internal organs by yeast-like opportunistic fungi of the genus Candida. Provoking factors are long-term use of medications (antibiotics, cytostatics, glucocorticosteroids), endocrine diseases, microtraumas, infectious and oncological diseases, etc.
- Versicolor (pityriasis versicolor), which affects only the horny substance of the epidermis, is characterized by slight contagiousness and the absence of inflammatory phenomena. The causative agent of the disease is the lipophilic yeast-like dimorphic fungus Malassezia furfur. Increased sweating provokes the development of this mycosis.
Since it is not always possible to immediately determine the cause of skin lesions, and the infection can be mixed, the mycologist also treats various dermatitis.
A mycologist is a doctor who treats diseases of a bacterial nature if they are caused by mycoses:
- panniculitis;
- paronychia;
- impetigo.
A mycologist treats excessive sweating as a concomitant disorder of fungal diseases, as well as non-fungal nail diseases.
In addition, a mycologist can treat demodicosis, a disease caused by opportunistic demodex mites.
Origin of mushrooms
An international team of scientists has described a species of mushroom from Northern Canada and concluded that its representatives grew on Earth 1 billion years ago. Previously, the oldest fossilized mushrooms were considered to be from Scotland, which dated back to the Devonian period (410 million years ago), and Wisconsin (Ordovician period, 450 million years ago). Following these findings, it was believed that fungi appeared between 740 and 1060 million years ago. Now the time of their appearance is moving even deeper into antiquity.
In 2.2–2.4 billion-year-old volcanic rocks from South Africa, scientists have discovered numerous filament-like formations. They filled the nodules, which were formed from bubbles of gas captured by the lava. In their characteristics, these formations are similar to mushroom mycelium. There is no doubt about the mushroom nature of these threads, so the origin of mushrooms will have to be seriously ancient. Also, the presence of fungal representatives in ancient bottom rocks casts doubt on the terrestrial origin of the ancestors of fungi.
In what cases is it necessary to contact a mycologist?
A mycologist is needed for patients who:
- the nail plate is deformed;
- the color of the nails has changed or the nail has become thicker;
- localized hair loss is observed;
- patches of baldness appeared on the head;
- dandruff is present;
- the skin peels, itches or turns red (first of all, you should suspect the presence of a fungus if these disorders affect the legs);
- there are scaly bumps on the skin;
- changes in the surface of the mucous membranes are observed;
- the skin is covered with white or brown spots.
How does an appointment with a mycologist go and the diagnostic methods he uses?
Important! Before going to an appointment with a mycologist, you need not only to make an appointment, but also to prepare – physically and mentally.
Preparatory activities before visiting a doctor include:
- Remember all the features of the symptoms - when they appeared, how they are expressed, what helps to alleviate the condition.
- Collect all available medical documentation and take it with you to your doctor’s appointment.
- Wear such clothes and shoes that there will be no difficulty in undressing during the examination. Be mentally prepared for the fact that you may need to strip down to your underwear.
- The skin in the affected area should be clean. That is, you need not only to take a shower, but also not to apply any medications to the skin (nails, hair).
An appointment with a mycologist will begin with a conversation between the doctor and the patient , during which the doctor will collect data to compile an anamnesis. The specialist will ask questions about the symptoms, possible (in the patient’s opinion) places of infection, that is, whether the patient goes to the sauna, bathhouse, or whether he knows anyone with similar symptoms. Questions regarding lifestyle, the presence of pets, place of work, and the presence of acute or chronic somatic diseases will also be clarified.
After this, the doctor will perform a general examination of the patient, paying special attention to the places where the lesions appeared . If the mycologist’s office has a special ultraviolet light lamp (Wood’s lamp), the doctor examines the patient’s skin (hair, eyelashes, nails) with its help. In ultraviolet light, fungal waste products have a characteristic glow and fluoresce.
Neurosurgeon: what and how this doctor treats
It is very likely that the mycologist will take a scraping from the skin with a scalpel, remove the protruding part of the nail plate or the ends of the hair at the site of signs of the disease. Additional studies may also be prescribed for accurate differential diagnosis. For example, if mycotic lesions of the ENT organs are suspected, smears will be taken from the mucous membranes of the mouth, throat, nose, and inner surface of the ear.
Once the patient's biological material has been obtained, a variety of traditional and innovative research methods can be applied. The purpose of the research is to determine the culture of microorganisms and their type. Without this, adequate treatment is impossible. The following methods are used:
- Microscopic examination of the material (bacterioscopy).
- Sowing on a nutrient medium, often on several media.
- Crystallographic method.
- Chemiluminescence analysis.
- General clinical and/or biochemical blood and urine tests.
- Immunological blood test.
- Study of materials using potassium hydroxide (KOH) and a microscope.
- Express diagnostics by measuring the electrical resistance of the skin in the affected areas - electropuncture diagnostics according to Voll.
- Express diagnosis of fungal microorganisms using the serum portion of the patient’s blood – an immunobisensory method.
- To identify deep candidiasis, as well as for the purpose of genotyping and determining the species of microorganisms, the polymerase chain reaction (PCR) method can be used.
In the case of express diagnostics, results can be obtained within a few hours. In other cases, the results of the studies will be known to the doctor in 2-7 days . Therefore, to begin treatment, the patient will need to visit the doctor again. At the first appointment, a preliminary diagnosis can be made and temporary treatment can be prescribed to alleviate the patient’s condition while awaiting the results of laboratory tests.
to contents ^
Treatment
The mycologist selects a treatment regimen based on the type of pathogen.
To treat mild forms of mycosis, the mycologist selects topical antifungal drugs, and for the treatment of severe forms of mycosis, antifungal drugs are prescribed orally.
For some rapidly progressing fungal diseases (mucormycosis), the patient also needs surgical treatment, since the mycologist diagnoses the patient when the body tissues have already been significantly damaged.
Notes
- Kursanov, 1940.
- Vasilkov, 1953.
- ↑ 123
Zagalna mycology, 2007, p. 7. - Kursanov, 1940, p. 416.
- Zagalna mycology, 2007, p. 8.
- ↑ 123
Kursanov, 1940, p. 417. - ↑ 12
Zagalna mycology, 2007, p. 9. - Vasilkov, 1953, p. 13-14.
- Kursanov, 1940, p. 417-418.
- Zagalna mycology, 2007, p. 10.
- Kursanov, 1940, p. 418.
- Zagalna mycology, 2007, p. eleven.
- ↑ 12
Kursanov, 1940, p. 423. - Collins S.
The Present State of Russia, in a letter to a friend at London, written by an Eminent Person residing at the Great Tzars court at Mosco for the space of nine years. Illustrated with many copper plates. - London, 1671. - 144 p. - Vasilkov, 1953, p. 16.
- Zagalna mycology, 2007, p. 12-13.
- Zagalna mycology, 2007, p. 21.
- ↑ 12
Kursanov, 1940, p. 419. - Zagalna mycology, 2007, p. 14.
- ↑ 12
Zagalna mycology, 2007, p. 15. - Ainsworth, 2009, p. 2.
- Vasilkov, 1953, p. 25-29.
- Enumerationem ad 430 specierum Fungorum prope Petropolin crescentium conscripsit, quae nunquam typis excusa est et jam non existat
- Vasilkov, 1953, p. 31.
- Vasilkov, 1953, p. 35.
- Vasilkov, 1953, p. 35-38.
- Vasilkov, 1953, p. 41-42.
- Kursanov, 1940, p. 453.
- Vasilkov, 1953, p. 45.
What does he do?
In order to have the right to engage in medical practice in the field of mycology, it is necessary to obtain a diploma of higher medical education and complete a full internship course in the dermatology department under the guidance of an experienced physician. Such a doctor receives a narrow specialization after completing appropriate postgraduate education courses.
The main areas of activity of a mycologist include:
- identification and determination of the species of fungal microflora on the skin;
- prescribing diagnostic procedures depending on the expected type of mycosis;
- development of complex treatment aimed at eliminating the pathogenic agent in mycosis;
- prevention of fungal infections.
In addition, this specialist can study and improve new drugs and therapeutic regimens for different age categories of patients against mycoses and fungal infections.
An important point in the work of a mycologist is the ability to distinguish fungal diseases from other pathologies that look very similar in appearance and symptoms. Often similar symptoms are caused by allergic reactions, chronic smoking, digestive system problems, etc. A mycologist must be able to identify the difference by appearance and signs in order to reduce diagnostic time.
Most often, this doctor has to deal with the following groups of mycotic flora:
The list of pathologies included in the scope of activity of a mycology specialist is very wide. The most common diseases that this doctor has to deal with are the following:
Correct interpretation of signs and prescription of correct treatment are the primary tasks of the mycologist.
At the reception
When visiting a medical facility, the patient is referred to a dermatologist, and it is this specialist who will explain in more detail which doctor treats fungal infections.
The first consultation consists of the specialist listening to the patient’s complaints and making a visual assessment of the condition of the epidermis or nail plate. The next step is to examine the infected part of the body using a Wood's lamp. This device is necessary to detect mycosis of the skin. After this, the mycologist takes a scraping from the affected area of skin. Therefore, before examination by a specialist, it is forbidden to treat the dermis with medications. Just wash your skin. At the end of the appointment, the doctor gives a direction for additional tests and informs the date by which the results will be ready.
Literature
- Kudryashova Z. N.
Mycology with the basics of phytopathology. - Minsk, 1968. - Kursanov L.I.
Essay on the development of mycology // Mycology. - M.: Uchpedgiz, 1940. - Vasilkov B.P.
Study of cap mushrooms in the USSR: Historical and bibliographical essay. - M.-L.: ed. USSR Academy of Sciences, 1953. - 192 p. - Müller E., Löffler V.
Mycology / trans. with him. K. L. Tarasova. - M.: "Mir", 1995. - 343 p. — ISBN 5-03-002999-0. - Ainsworth GC
Introduction to the History of Mycology.
- Cambridge University Press, 2009. - 376 p. - ISBN 9780521112956. (English) ( Ainsworth J.K.
Introduction to the history of mycology) - Leontiev D.V., Akulov O.Yu.
Foreign mycology: A handbook for all initial deposits. - Kharkiv: "Osnova", 2007. - P. 192-206. — ISBN 978-966-495-040-1. (Ukrainian) (General mycology: Textbook for higher educational institutions) - World of plants. In 7 volumes/Editorial collection. A. L. Takhtadzhyan (chief editor) and others. T. 2. Mushrooms / Ed. M. V. Gorlenko. — 2nd ed., revised. - M.: Education, 1991. - 475 p.