Home page / Specialists / Pulmonologist / Pulmonologist services
Pulmonology is a medical field that deals with the diagnosis and treatment of respiratory diseases. Pathologies of the respiratory system occupy a leading position among organ diseases. The environmental situation, smoking, genetics and other factors contribute to the spread of lung and respiratory diseases. Among the main pathologies that pulmonology deals with are the following:
- inflammatory processes of the upper and lower respiratory tract;
- fungal and parasitic lung diseases;
- lung tumors;
- occupational respiratory diseases;
- congenital abnormalities of the respiratory system;
- obstructive diseases and others.
Diseases of the respiratory system are treated by a pulmonologist. Based on the patient’s complaints and a series of diagnostic measures and studies, the specialist makes a diagnosis and selects appropriate treatment. In each individual case, it is necessary to take into account the place of residence, working conditions, and genetic characteristics. Therefore, a different treatment plan is developed for each patient. The pulmonologist monitors the dynamics of changes, conducts intermediate diagnostics, and, if necessary, adjusts the treatment regimen.
When to see a pulmonologist
You should consult a pulmonologist if you experience one or more of the following symptoms:
- persistent cough;
- discharge of sputum with blood;
- chest pain;
- frequent fever;
- whistling or wheezing in the lungs when breathing;
- dyspnea.
In addition, it is necessary for smokers and those who work in hazardous industries associated with chemical or mechanical air pollution to periodically visit a pulmonologist.
What drugs are used in the treatment of bronchitis?
There is a significant list of medications that are used as part of the course of treatment for bronchial inflammation.
They are divided into several separate categories, named based on the main therapeutic effect of the drug:
- antiviral group of pharmacological agents;
- category of antibacterial drugs;
- anti-inflammatory group of drugs;
- expectorant category of drugs;
- bronchodilator group of medications.
Antibacterial pharmacological agents are prescribed based on the individual clinical picture of the patient and in the presence of complications in the form of secondary bacterial infection. However, their use may be necessary at the initial stages of bronchitis development, when it is revealed that the cause of the disease lies in some pathogenic microorganism.
The medication can be prescribed for use in various pharmacological forms of release, such as:
- injection;
- tablet form;
- capsules;
- suspension;
- syrup.
With the correct selection of an antibiotic and its use according to strict indications and in full compliance with medical recommendations regarding the frequency of administration, dosage and duration of antibacterial therapy, noticeable improvements in the patient’s condition are observed already on the 3rd day.
But, most often, bronchitis is provoked by a variety of viruses, for which the use of antibacterial drugs is inappropriate and ineffective. Each of the drugs has its own indications for use and only if they are followed, the use of the medication is advisable.
Thus, it is possible to draw the following conclusions:
- If an infection enters the body, antiviral drugs must be prescribed.
- When inflammatory processes of the mucous membranes of the bronchi are accompanied by elevated body temperature, it is necessary to use antipyretic drugs.
- If the patient experiences shortness of breath, it is necessary to start taking bronchodilators.
- If you have a non-productive cough, that is, a dry cough, you need to take expectorant medications.
In order to reduce the list of pharmacological agents used, it is possible to use drugs with combined effects that combine 2 multidirectional therapeutic effects. This will reduce the load on the liver and kidneys due to the excessive toxic effects of medications on them.
Certain diseases are associated with changing weather conditions. These include bronchitis, which doctors call a seasonal pathology. It is often caused by a change in temperature. The immune system does not have time to adapt to the sudden cold snap. The danger of this disease lies in the fact that many people self-medicate and believe that with it they can safely go to work or school. In fact, this results in serious consequences, for example, pneumonia or bronchial asthma.
The main sign of a problem in the lungs is a cough. This is due to the fact that an inflammatory reaction begins in the bronchi, which gradually irritates the cough receptors. 2-3 days after the onset of the disease, sputum is released, which helps to quickly remove mucous or purulent contents in the lungs. In addition, signs of bronchitis include:
- increased body temperature;
- general weakness;
- dyspnea;
- fast fatiguability;
- discomfort in the chest area.
Any type of bronchitis has all these symptoms. In its viral form, body temperature rises especially strongly. The same process occurs with a bacterial type of pathology. This is due to the fact that due to the inflammatory process, many toxins enter the blood. They lead to a reaction in the body in the form of an increase in body temperature. In addition, intoxication also provokes severe weakness.
Department of Pulmonology "SM-Clinic"
The pulmonology department of our clinic employs highly qualified pulmonologists with extensive experience. By contacting us with their problem, patients receive not only an attentive and tactful attitude, but also prompt assistance, the possibility of high-quality diagnostics using modern equipment, and an individual treatment plan drawn up by a specialist.
The Pulmonology Department of our clinic offers services for the diagnosis and treatment of the following diseases:
- pneumonia,
- obstructive pulmonary disease,
- tuberculosis (diagnosis only),
- pleurisy,
- cough,
- bronchial asthma,
- tracheobronchitis,
- pulmonary hypertension,
- cystic fibrosis,
- emphysema and others.
The pulmonology department at SM-Clinic has all the necessary modern equipment to conduct high-quality examinations and obtain highly accurate results. An integrated approach, which in addition to hardware examination also involves laboratory tests and analyses, allows us to identify the cause of the disease and make an accurate diagnosis at an early stage of the disease, preventing its progression and complications.
Advice from a pediatric pulmonologist
Hardening is a system of measures aimed at increasing a child’s endurance, his body’s resistance to meteorological factors: cold, humidity and air movement, changes in atmospheric pressure and harmful environmental factors.
The basis of hardening is training - systematic repetition of hardening activities, starting with short-term and weak ones, with a gradual increase in duration and strength.
The basic rules of hardening are: gradual increase in the strength of the influence of the hardening factor, systematicity and consistency. Of course, how to harden is decided individually, and depends on the age and health of the child. The doctor who is observing the child should help with this.
You need to harden gradually, showing not only caution, but also patience and tact. It is very important that all hardening activities evoke positive emotions in the child, a joyful and calm mood during the procedure. It’s even better if they have the nature of a game or if the game is accompanied by positive emotions - a great healing power.
The main types of hardening: walks and air baths. In this case, natural factors are used: air, water, sunlight. So, hardening a child is carried out using various methods and can begin from the first weeks of life. Air and water procedures are accessible, most frequently used and effective for the prevention of respiratory viral infections and pneumonia.
Daily walks not only prevent the occurrence of colds, but also rickets, anemia, and improve the baby’s appetite, sleep and mood. A child born in the cold season (autumn, winter, early spring) can be taken for the first walk in the 2-3rd week of life at an air temperature of at least 10 ° C. The duration of the first walks is 10-20 minutes, and then they gradually extend to 1 hour or more. The very first walks in the first weeks of a child’s life can be arranged in the room; to do this, you need to dress the child as if for a walk and open a window, a window, or slightly open the balcony door.
It is important that the stream of cold air does not fall on the child. During strong winds, it is advisable to walk behind the house, where there is no strong wind. In winter, it is advisable to go for a walk at 11-12 noon, and if the sun appears at this time, expose the child’s face to the winter sun’s rays. Under the influence of ultraviolet rays, vitamin D is formed in the skin. We give parents this advice: not a single day without walking in the fresh air.
In the fresh air, children sleep better and fall asleep faster. The duration of sleep in the cold season is initially 20-40 minutes, and then lengthens to 1 hour or more. Naturally, in the warm season, the duration of sleep in the fresh air lengthens. In summer, it is better to put your child to sleep in the shade of trees.
You can walk with children over 3 years old in any weather. In winter, in calm weather, you can walk at an air temperature of - 15-18 ° C, with preschool children up to - 22 ° C. It is very important to dress children correctly for a walk. Clothes should be warm and not restrict movement. You should not put a hat, woolen blouse, thick socks, jacket, or felt boots on your baby in the room. In the summer, the baby should spend most of the day in the fresh air: on the playground, in the garden, in the forest, etc.
Air baths can be performed both in the room and in the air. In infants, air baths begin with leaving the baby naked for 1-2 minutes when changing diapers.
From 2-3 months, air baths are carried out systematically at a room temperature of 20-21°C, in the summer - in the shade outside under trees and at a temperature not lower than 22°C. Air baths start with 2 minutes, 2-3 times a day. The duration of the air bath is increased every week by 1 minute and by the end of the year it reaches 30 minutes. Children accustomed to air procedures can remain in the air for 45-60 minutes.
From 5 months of age you can start wiping. They are usually done in the morning after the child wakes up. To do this, use water at a temperature of 36°C. Rubbing is done with a terry cloth mitten, gradually: first with one hand (from bottom to top), then rub it with a dry terry towel until it becomes slightly red. Next, they sequentially wipe the second arm, both legs, chest and stomach, and back. The whole procedure lasts 5-6 minutes, after which the child is placed under a blanket for 10-15 minutes. Every week the water temperature decreases by one degree and is brought to 30-28°C for infants, and to 25°C for older children. You can add sea or regular salt to the water at the rate of 1 teaspoon per 1 glass of water.
Pouring can be used for children over 1 year of age. It is recommended to start this procedure in the warm season and continue in winter. Dousing begins with a water temperature of 35-36°C, gradually lowering the water temperature by 1°C every week, bringing it to 28°C for children under 2 years of age and to 25°C for older children. After dousing the child, wipe it dry.
Pouring your feet with cool water can be used as a hardening agent for children. Children can be introduced to foot baths from the age of 1.5 years. Foot baths are best done before bed. First, warm water - 33°C, then gradually reduce the temperature to 20-18°C. This is the most convenient, simple, traditional, but extremely useful form of hardening. You can also advise your baby to “trample” his feet in this water. This type of hardening can be used throughout the year. It is advisable to start foot baths in the warm season. The use of water to harden children in everyday life must be combined with the formation of personal hygiene skills.
The combination of an air bath followed by wet rubbing or bathing has a very beneficial effect. Swimming in a river, lake or sea is allowed for children over 2-3 years old. The water temperature should be no lower than 23-25°C, and the air temperature – 25-26°C. The duration of bathing should not exceed 5 minutes, and subsequently 10-20 minutes.
In the first days, it is recommended to swim no more than 1-2 times a day. While bathing, children need to be supervised and taught to swim at the same time. The best time for swimming is 10-12 noon. After bathing the child, you must immediately dry him, dress him and take him under an umbrella or canopy. Well-seasoned children can be allowed to swim in cooler water, reducing bathing time. In the summer, especially with older children, you can use water games.
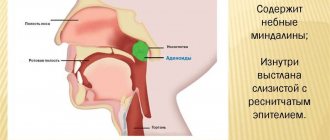
A simple but good means of hardening is to regularly rinse your mouth and throat with water at room temperature. Children can be taught to rinse their mouth from the age of three.
From the age of 5, you can learn to gargle in the morning after sleep and in the evening. It would be even better if the child does this at the same time as one of the parents. This procedure is especially useful for children with tonsil changes; in these cases, you can add one gram of table salt and 0.5 grams of baking soda to 1 glass of water. The procedure is not only hardening, but also disinfectant. The duration will be determined, of course, by the doctor.
Sunbathing can also be used with caution. If any of the hardening procedures was interrupted by illness, it can be continued only after the child has fully recovered, in consultation with a doctor. In this case, the temperature of the water and air should be slightly higher than that which was used to harden the child before the disease.
Pulmonary services
Computed tomography of the lungs.
One of the most informative, fast and accurate diagnostic methods. Shows the condition of the lungs in several projections. To obtain more detailed and clear images, a contrast agent is injected into a vein. The procedure does not require any special preliminary preparation, but it is not recommended to eat before it (bouts of nausea are possible).
Spirography.
A diagnostic method that allows you to evaluate the functions of external respiration. Based on spirography data, the specialist makes a conclusion about the dynamics of changes in the lungs during treatment, assesses the degree of pulmonary insufficiency, and makes a prognosis about the progression of the disease. Spirometry is also used for differential diagnosis between lung and heart failure.
Study of the diffusion capacity of the lungs.
Some respiratory diseases cause changes in the alveolar volume of the lungs (emphysema). This diagnostic method makes it possible to determine their degree.
Sputum analysis.
This type of research is very important, since the contents of sputum can indicate specific processes occurring in the lungs, including cancer.
Exercise tests.
Used for bronchial asthma to select the most effective drug. The tests are based on the fact that physical activity is the trigger for bronchospasms.
What does a pulmonologist treat?
To begin with, we note that the separation of pulmonology into an independent section of medicine, or rather into the internal section of medicine, occurred due to the concentration of a large amount of information on pathologies of the respiratory system of the human body. There are classifications of diseases according to etiology:
- Infectious, including viral and bacterial infections;
- Allergic;
- Hereditary pathologies;
- Traumatic (for example, due to fractured ribs, injury from ionizing radiation, etc.);
- Against the background of exposure to harmful factors in the process of professional activity;
- Diseases of unknown etiology;
All of the above is within the competence of a pulmonologist. What a pulmonologist treats in adults:
- Lung abscess is a purulent-destructive process of organic origin that occurs due to the active activity of harmful microorganisms (usually Staphylococcus aureus). Characterized by the formation of purulent cavities in the pulmonary parenchyma;
- AAA (allergic bronchopulmonary aspergillosis) is a disease that develops against the background of bronchial asthma or cystic fibrosis (in fact, against the background of weakened immunity), with the active development of a colony of soil fungi (aspirgillus);
- Bronchial asthma is a chronic inflammatory disease of the respiratory tract, occurring with the active participation of various cellular elements. As a rule, it occurs against the background of increased sensitivity to allergens and allergies, which are caused by nonspecific immunological processes that provoke partial/complete obstruction of the respiratory tract;
- Hemothorax. Occurs against the background of bleeding from the pulmonary vessels, against which there is an accumulation of blood in the pleural cavity;
- Pulmonary alveolar microlithiasis is a disease of unknown origin, characterized by the accumulation of minerals and proteins inside the alveoli. It is believed that this pathology is of hereditary origin or due to the influence of harmful production factors;
- Pulmonary infarction is a pathology that develops against the background of thrombosis or embolism of the branches of the pulmonary arteries/arteries;
- Psittacosis is an infectious disease that occurs due to the activity of protozoan parasites (bacteria) of the genus Chlamydia. As a rule, parasites initially enter the lungs, where they begin to actively multiply and develop;
- PH (pulmonary hypertension) - diseases (group) that occur against the background of increased pulmonary vascular resistance, causing premature death;
- Hamman-Rich syndrome is a rare disease that is characterized by diffuse damage to the pulmonary interstitium, provoking the development of respiratory failure, pneumosclerosis and other pathological processes;
- Lung cancer (diagnosis only). Treatment of cancer of the respiratory system is carried out by a pulmonologist-oncologist;
- Chronic/acute bronchitis. This disease occurs quite often and is an inflammatory process affecting the bronchi. It can develop against the background of prolonged exposure to external irritants (for example, dust) or due to an infectious lesion (viruses, bacteria);
- Pneumonia – inflammation of the lungs;
- COPD (chronic obstructive pulmonary disease) is a disease in which there is an irreversible disruption of the oxygen flow in the hollow respiratory organs, which occurs against the background of a pathological reaction of the tissues of the paired respiratory organ to the influence of external irritants (gases, pathogenic particles).
In addition to the above, a pulmonologist treats sarcoidosis, emphysema, cystic fibrosis, hemosiderosis, pulmonary fibrosis, tuberculosis and much more.
Chronical bronchitis
Chronic bronchitis is an inflammation of the bronchial mucosa, which is manifested by a constant cough and sputum production for at least 3 months a year for 2 or more years. The causes of chronic bronchitis are:
- smoking;
- occupational hazards (dust, gases);
- air pollution;
- previous acute bronchitis (chronic infection contributes to a long course of the disease).
Chronic bronchitis is fundamentally different from acute bronchitis not only in the reasons for its development, but also in the changes that occur in the bronchi. Chronic bronchitis is characterized by the release of large amounts of viscous mucus, which clogs the small bronchi. Acute bronchitis is one of the manifestations (or complications) of acute respiratory diseases (ARI), that is, it occurs due to a viral or bacterial infection. Chronic bronchitis has the following two forms:
- chronic simple bronchitis - damage to large and medium-sized bronchi without blockage of their lumen;
- chronic obstructive bronchitis (obstruction - blockage, obstruction) - profound changes occur not only in large and medium, but also small bronchi (bronchioles), while cough and sputum are accompanied by shortness of breath.
Bronchial asthma
Bronchial asthma is an allergic disease of the bronchi, which is manifested by attacks of suffocation that occur as a result of an increased reaction of the bronchi to allergens (substances that cause an allergic reaction). Bronchial asthma usually develops in the presence of a hereditary predisposition to allergic diseases (atopy). An allergic reaction of the bronchi to an allergen manifests itself:
- bronchospasm;
- production of large amounts of viscous mucus in the bronchi (edema of the mucous membrane).
These two processes lead to a rapid and almost complete closure of the lumen of the bronchi (mostly small ones), as a result of which air not only cannot enter the lungs, but also cannot escape from there. Patients often describe an attack of bronchial asthma as sudden suffocation and the inability to exhale.
Pneumonia
Pneumonia is the term used to refer to inflammation of the lungs. Pneumonia refers to an infectious lesion of the lung tissue. The cause of infection can be viruses, bacteria, fungi, mycoplasma, chlamydia and other microorganisms. In the classical presentation, pneumonia has the following stages:
- flushing stage (initial stage) – the appearance of exudate (inflammatory fluid) in the lungs (lasts up to 3 days);
- stage of red hepatization - the lung tissue loses its airiness and resembles liver tissue, due to the accumulation of exudate rich in red blood cells (lasts up to 3 days), while “rusty” colored sputum is released;
- stage of gray hepatization - red blood cells are destroyed, and in their place come leukocytes, which destroy microbes, forming pus, and purulent sputum is released (lasts up to 8 days);
- resolution stage – inflammation resolves and the airiness of the lungs is restored (lasts up to 12 days).
Pneumonia can be acute and protracted (lasts more than one month, but usually ends with recovery). Pneumonia has a different course and characteristics, depending on the pathogen, so doctors often classify pneumonia by the name of the microorganism, for example, adenoviral pneumonia or mycoplasma pneumonia. The transition of inflammation from the bronchi to the lungs is called bronchopneumonia.
Abscess and gangrene of the lungs
Abscess and gangrene of the lungs are purulent diseases of the lungs, in which there is destruction (melting) of the lung tissue under the influence of infection. These two conditions are often called destructive pneumonitis. Pneumonitis is all cases of inflammation of the lung tissue that do not fall under the description of classic pneumonia. An abscess, unlike gangrene, is limited from healthy tissue by a membrane that covers the area of necrosis (destruction, necrosis), and a cavity filled with pus is formed. Gangrene, on the other hand, does not have clear boundaries, so it is prone to quickly engulfing new tissue (the areas of decomposition are located next to healthy tissue). A lung abscess can occur against the background of pneumonia, and it takes 10 to 12 days to form.
Pleurisy
Pleurisy is inflammation of the pleura, or outer lining of the lungs. The pleura consists of two sheets, and between them there is normally a little fluid, which is necessary for the painless sliding of these sheets during breathing. Pleurisy can be:
- dry (fibrinous) - occurs if the inflammatory fluid quickly resolves, but fibrin (dense particles of inflammatory fluid) remains on the pleural leaves, and friction of the leaves against each other (during breathing) causes severe chest pain;
- effusion (exudative) - occurs if a lot of inflammatory fluid accumulates in the pleural cavity, while the process of straightening the lungs is disrupted, but there is no pain.
Pleurisy occurs in the following cases:
- infection – bacteria, viruses, fungi, protozoa, parasites (echinococcosis);
- non-infectious causes - malignant tumors, allergic and autoimmune diseases (for example, systemic lupus erythematosus, pleurisy after myocardial infarction), chest trauma, chronic renal failure, pulmonary infarction, and pleural effusion due to pancreatitis (inflammation of the pancreas).
Special conditions of the pleura include:
- pleural empyema – purulent pleurisy (empyema is an accumulation of pus in a natural cavity);
- hydrothorax (hydro - water, thorax - chest) - accumulation of non-inflammatory (edematous) fluid in the pleural cavity, which is especially characteristic of heart failure;
- hemothorax - accumulation of blood in the pleural cavity (heme - blood).
If inflammation of the lungs spreads to the pleura, then this condition is called pleuropneumonia.
Bronchiectasis
Bronchiectasis is a chronic disease of the bronchi, in which their expansion (ectasia) and purulent inflammation (purulent endobronchitis) are observed. The causes of bronchiectasis are:
- weakness of the bronchial wall (genetically determined underdevelopment of the bronchial muscles);
- frequent infectious and inflammatory diseases of the bronchi and lungs in childhood (can cause dilatation of the bronchi in the presence of a hereditary predisposition);
- congenital bronchiectasis (account for 6% of cases).
With this pathology, mainly the bronchi in the lower parts of the lungs are affected, so in such patients bronchopneumonia is observed, often in the same place (which is confirmed by x-ray).
Emphysema
Emphysema is an increase in the airiness of the lungs that occurs due to the expansion of the alveoli (the small bubbles that make up the lungs and in which gas exchange occurs). Emphysema can be:
- an independent disease - occurs due to a lack of alpha-1-antitrypsin, which maintains the elasticity of the lung tissue (observed in children, is a hereditary disease);
- a consequence of other diseases - formed with long-term obstructive bronchitis (especially in smokers).
Chronic obstructive pulmonary diseases
Chronic obstructive pulmonary diseases (COPD) are diseases of the lungs and bronchi, which are united by a common development mechanism, namely, obstruction of the bronchial tubes (obstruction). Chronic obstructive pulmonary diseases include:
- chronic obstructive bronchitis;
- bronchiolitis obliterans (a disease of the small bronchi that leads to their blockage);
- bronchial asthma;
- emphysema.
The disease can occur in two forms:
- bronchitis - cough with sputum prevails over shortness of breath;
- emphysematous - shortness of breath comes to the fore, the cough is less pronounced, little sputum is produced.
Advantages of the pulmonology center "SM-Clinic"
- High professionalism and competence of pulmonologists.
- Modern diagnostic equipment.
- Wide range of laboratory research opportunities.
- Possibility of a complete examination of the respiratory system and assessment of its condition.
- Patient management from the moment of treatment until complete recovery with constant monitoring of changes.
- Comfortable conditions, visiting at a convenient time, attentive and friendly staff.
Contact the pulmonology department of our clinic in St. Petersburg for any problems with the respiratory system. We do everything possible to ensure that each of our patients can breathe freely and fully.
What is pulmonology, who is a pulmonologist: explanation
A pulmonologist is a doctor who treats the respiratory system. The answer to the question, what is pulmonology , is encrypted in the term itself, which comes from the Latin word “ pulmones” - lungs, and the ancient Greek word “λόγος” , which means “science” or “teaching”.
However, not all diseases that affect the respiratory system fall within the competence of a pulmonologist. A pulmonologist can more accurately diagnose problems, but sometimes he refers the patient to more specialized specialists. So, what is pulmonology and what diseases and conditions does a pulmonologist not deal with :
- Tuberculosis. A pulmonologist can diagnose it, but treatment is carried out by a highly specialized TB .
- Surgical operations on the chest organs are the area of expertise of a thoracic surgeon .
- Life-threatening conditions undoubtedly require the intervention of a resuscitator .
- Diseases of the upper respiratory tract are often treated by ENT . Although a pulmonologist also often deals with them, since problems in the lower respiratory tract are sometimes associated with problems in the upper respiratory tract.
Respiratory diseases are treated by pulmonologists and doctors of other specializations
Puncture of the pleural cavity
To diagnose diseases of the pleura and lungs, pleural puncture may be prescribed. It is also called thoracentesis or thoracentesis. A puncture of the outer (parietal) pleural membrane is performed for diagnostics (examination of the pleural cavity, collection of accumulated fluid for examination in the laboratory) or for therapeutic purposes (freeing the cavity from effusion).
Our specialists
The success of treatment depends 90% on the experience and qualifications of the doctor. Our specialists, being scientific employees of the Federal State Institution Research Institute of Pulmonology of the Federal Medical and Biological Agency of Russia, supervise entire areas in pulmonology of the Russian Federation.
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist of the highest category, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Samoilenko Viktor Alexandrovich
Candidate of Medical Sciences, pulmonologist of the highest category. Nominee of the National Award “Best Doctors of Russia” “Calling”.
30 years of experience
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
I. General provisions
1. A person with a higher education - a specialty in the specialty "General Medicine" or "Pediatrics" and residency training in the specialty "Pulmonology" or higher education - a specialty in the specialty "General Medicine" or "Pediatrics" - is appointed to the position of a pulmonologist. training in internship and (or) residency in one of the specialties: “General medical practice (family medicine)”, “Pediatrics”, “Therapy”, “Phthisiology”, “Thoracic surgery”, “Allergology and immunology” and additional professional education in professional retraining program in the specialty “Pulmonology”.
2. There are no requirements for practical work experience.
3. Additional requirements for permission to work:
— specialist certificate or certificate of accreditation of a specialist in the specialty “Pulmonology”;
— undergoing mandatory preliminary (upon employment) and periodic medical examinations (examinations), as well as extraordinary medical examinations (examinations) in the manner established by the legislation of the Russian Federation;
— no restrictions on engaging in professional activities established by the legislation of the Russian Federation.
4. Appointment to the position of a pulmonologist, as well as dismissal from it, is made by order of the head of the organization.
5. A pulmonologist should know:
5.1. The procedure for providing medical care to the population in the field of pulmonology
5.2. Standards of medical care for diseases of the bronchopulmonary system
5.3. Clinical recommendations (treatment protocols) for the provision of medical care, taking into account the standards of medical care
5.4. Methods of laboratory and instrumental studies in patients with diseases of the bronchopulmonary system
5.5. ICD
5.6. Classification of functional disorders and complications in diseases of the bronchopulmonary system
5.7. Clinical and radiological semiotics of diseases of the bronchopulmonary system
5.8. Complications of diseases of the bronchopulmonary system and measures to prevent them
5.9. Features of the course of diseases of the bronchopulmonary system against the background of concomitant diseases
5.10. Features of the clinical manifestation and course of diseases of the bronchopulmonary system, their detection and prevention in patients under 18 years of age with diseases of the bronchopulmonary system or suspected diseases of the bronchopulmonary system
5.11. Features of the clinical manifestation and course of extrapulmonary diseases of the bronchopulmonary system
5.12. Principles of diagnosis, differential diagnosis of conditions requiring emergency medical care for diseases of the bronchopulmonary system
5.13. Symptoms and syndromes of complications, side effects, undesirable reactions, including unexpected ones, resulting from laboratory and instrumental studies in patients with suspected diseases of the bronchopulmonary system
5.14. Principles of organizing medical triage, the procedure for providing specialized medical care to the population in emergency situations, during terrorist attacks and military conflicts at the stages of medical evacuation
5.15. The procedure for organizing medical evacuation in emergency situations, during terrorist attacks and military conflicts
5.16. Medical indications and medical contraindications for the prescription of drugs, medical devices and nutritional therapy in patients with diseases of the bronchopulmonary system
5.17. Mechanism of action of drugs, medical devices and medical nutrition used in patients with diseases of the bronchopulmonary system
5.18. Medical indications and medical contraindications for surgical treatment of patients with diseases of the bronchopulmonary system
5.19. Principles and methods of providing emergency medical care to patients with diseases of the bronchopulmonary system in accordance with the current procedures for the provision of medical care, clinical recommendations (treatment protocols) for the provision of medical care, taking into account the standards of medical care
5.20. The procedure for organizing medical rehabilitation and the procedure for organizing sanatorium-resort treatment
5.21. Fundamentals and methods of medical rehabilitation of patients with diseases of the bronchopulmonary system
5.22. Side effects and possible complications of medical rehabilitation of patients with diseases of the bronchopulmonary system and methods for their prevention
5.23. Medical indications and medical contraindications for rehabilitation measures for patients with diseases of the bronchopulmonary system
5.24. Medical indications and medical contraindications for spa treatment of patients with diseases of the bronchopulmonary system
5.25. The mechanism of the impact of rehabilitation measures on the body of patients with diseases of the bronchopulmonary system
5.26. Medical indications for referring patients with diseases of the bronchopulmonary system to medical specialists for prescribing medical rehabilitation measures, including the implementation of an individual rehabilitation program or habilitation for people with disabilities, and sanatorium-resort treatment
5.27. Legislation of the Russian Federation in the field of protecting the health of citizens, regulatory legal acts regulating the activities of medical organizations and medical workers, including in the field of prescribing, prescribing and storing narcotic drugs and psychotropic substances
5.28. Procedures for providing palliative care to adults and children
5.29. Classifications, symptoms and syndromes of incurable progressive diseases and conditions
5.30. Methods for clinical diagnosis of incurable progressive diseases and conditions
5.31. Rules for carrying out and stopping resuscitation measures for patients against the background of progression of reliably established incurable diseases
5.32. Principles of providing psychological support to patients and their legal representatives, taking into account the individual characteristics of the behavior of a terminally ill patient
5.33. The procedure for issuing certificates of temporary incapacity for work
5.34. Medical indications and procedure for referring patients with diseases of the bronchopulmonary system for medical and social examination
5.35. The procedure for conducting medical examinations
5.36. Requirements for the preparation of medical documentation for referral for medical and social examination of patients with diseases of the bronchopulmonary system in federal state institutions of medical and social examination
5.37. Regulatory legal acts regulating the procedures for dispensary observation of patients with diseases of the bronchopulmonary system
5.38. Forms and methods of sanitary and hygienic education, work on the formation of elements of a healthy lifestyle, including programs to reduce tobacco consumption, prevent and combat non-medical use of narcotic drugs and psychotropic substances
5.39. Basics of a healthy lifestyle, methods of its formation
5.40. Forms and methods of sanitary and hygienic education among patients (their legal representatives), medical workers on the prevention of diseases of the bronchopulmonary system
5.41. Principles and features of preventing the occurrence or progression of diseases of the bronchopulmonary system and their consequences
5.42. Medical indications and medical contraindications for the use of methods for the prevention of diseases of the bronchopulmonary system in patients in accordance with the current procedures for the provision of medical care, clinical recommendations (treatment protocols) for the provision of medical care, taking into account the standards of medical care
5.43. Principles and features of health-improving activities among patients with chronic diseases and consequences of diseases of the bronchopulmonary system
5.44. Rules for the preparation of medical documentation in medical organizations providing medical care in the field of pulmonology, including in the form of an electronic document
5.45. Rules for working in information systems in the field of healthcare and the information and telecommunications network “Internet”
5.46. Fire safety requirements, labor protection, basics of personal safety and conflict management, internal labor regulations
5.47. Requirements for ensuring internal quality control and safety of medical activities
5.48. Job responsibilities of medical workers in medical organizations providing medical care in the field of pulmonology
5.49. _____________________________________________________________________
6. A pulmonologist reports directly to __________________________.
7. During the absence of a pulmonologist (vacation, illness, etc.), his duties are performed by a person appointed in the prescribed manner. This person acquires the corresponding rights and is responsible for their proper execution.
8. The pulmonologist must comply with:
- medical confidentiality, doctor’s oath;
— principles of medical ethics and deontology in working with patients, their legal representatives and colleagues;
— legislation of the Russian Federation in the field of health care, regulations and other documents regulating the activities of medical organizations and medical workers;
— programs of state guarantees for the provision of free medical care to citizens.
9. ________________________________________________________________