Many of us are familiar with an otolaryngologist who treats diseases of the mucous membranes of the throat and nose, as well as pathologies associated with the ears. ENT is a general specialist. In the same area, but in a narrower profile, there is another doctor who deals with hearing pathologies - an audiologist. Every person experiencing a decrease in hearing acuity or complete loss of hearing needs to immediately visit a doctor of this profile, carry out full diagnostic hearing tests and begin timely treatment.
Demand for an audiologist
The human body is designed in such a way that it receives basic information about the world around us through sight and sounds. Currently, there is a noticeable deterioration in hearing in people not only in old age, but also in active age. This situation is associated with technical progress, which is accompanied by constant acoustic load. This is especially true for residents of large cities. For this reason, an audiologist today is a highly sought-after specialist.
The World Health Organization estimates that 360 million people worldwide (5% of the population) have disabling hearing loss, of whom 32 million are children.
Audiology is a relatively young medical field (this specialty appeared in our country in the 90s of the last century). Therefore, not every medical institution is staffed with such a specialist. Audiologists practice in large public and private medical centers. If it is not possible to immediately get an appointment with this doctor, it is advisable to begin solving hearing problems with a consultation with an otolaryngologist.
Science of audiology
Audiology is a branch of science that deals with hearing and the hearing organs, that is, the ears.
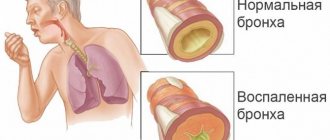
Unlike an otolaryngologist, this specialist deals with problems of the middle and inner ear, that is, deeper hearing damage than the well-known ENT specialist. It is the otolaryngologist who most often gives the patient a referral to an audiologist.
Typical patients of an audiologist are people who have lost their hearing. These are deaf and dumb. Naturally, in this case, treatment is impossible, so the specialist will select a suitable hearing aid that will improve the patient’s condition. In some cases, amplifiers allow the patient to receive at least some percentage of the sounds of the outside world.
According to statistics, many people do not even realize that they have hearing problems, which can only be determined by diagnostics. The human brain is designed in such a way that some hearing problems are compensated for by the brain's reserves. Meanwhile, 10% of all people have various hearing impairments, which are aggravated by listening to music on headphones, staying in noisy places, head injuries, and severe otitis media. In fact, there are many such reasons. This is what an audiologist does.
Only this specialist can tell with maximum accuracy how much hearing loss the patient has, for which the audiometry method is used - this is the main diagnosis.
An audiologist is a doctor in the field of otolaryngology. Only an audiologist treats more specific ear problems, which may include congenital and acquired diseases of the hearing organs. The otolaryngologist, in turn, deals with inflammation inside the ear. An audiologist does not treat external ear diseases.
An audiologist has a whole range of tools in his arsenal, with which he diagnoses pathologies and, after identifying them, carries out treatment. This specialist works closely with other specialists, such as a surgeon. However, often the doctor who specializes in audiology is himself a surgeon, so he can perform operations. The modern level of development of medicine even makes it possible to restore ear cartilage from the body’s own resources.
An audiologist is a specialist, so not everyone can get an appointment with him. You won’t find this specialist in the district clinic. Each regional clinic probably has at least 1 such audiologist. This means that finding a qualified audiologist is not at all easy.
It is quite possible to contact this specialist on your own if you often ask again and again in a conversation with your interlocutor, constantly do not hear enough, or increase the volume of the TV or receiver. This applies to adults.
Audiologist and ENT doctor - what is the difference?
An audiologist is an otolaryngologist (ENT doctor) with extensive knowledge in the field of hearing pathologies, so his medical specialization is narrower. Unlike an otolaryngologist, his area of expertise does not include inflammatory pathologies of the ear. An audiologist deals with pathologies associated with disorders of the main function of this organ – hearing.
An ENT doctor can refer a patient for a consultation with an audiologist if, during the treatment of an acute illness, a persistent impairment of auditory perception occurs in a person.
Preventing ear problems
Like any other disease, ailments affecting the ears are easier to prevent than to treat. In order to maintain a sufficiently high level of hearing, it is necessary to avoid constant negative influences. In this regard, so-called industrial noise is especially dangerous. It leads to a gradual decrease in the elasticity of the eardrum.
Nowadays, many people use cotton swabs to clean earwax from their ear canals. In fact, this approach is unacceptable. The fact is that these devices are absolutely not intended for such events. Moreover, such manipulations can lead to serious damage to the eardrum.
It is very important to quickly and fully treat any acute diseases associated with the ears. If you do not do this, then in the very near future you may encounter even greater hearing problems. So, speaking about what an audiologist does, we should never forget about prevention.
What does an audiologist treat?
Unlike an ENT specialist, who deals with the elimination of acute pathology, an audiologist specializes in chronic hearing impairment, which can be either congenital or acquired. Such diseases include:
- Deafness. One of the most pressing problems of modern audiology. The disease is characterized by profound hearing loss, up to a complete lack of perception of human speech. Deafness can develop as a result of damage to the auditory nerve, or as a result of a disturbance in the conduction of sound to the inner ear. The audiologist must accurately determine the cause of the hearing loss, since the treatment process may depend on this.
- Otosclerosis. With this disease, the metabolism of bone tissue is disrupted, which leads to its pathological growth. Changes occur in the middle ear, where the most important elements necessary for the perception of sound waves are located. Early diagnosis of otosclerosis by an audiologist will help avoid severe hearing loss.
- Hearing loss. Characterized by hearing loss of varying degrees. The disease can be congenital, or it develops as a result of an acquired pathology, for example, sulfur plugs. In the latter case, an audiologist will help quickly resolve the problem.
Specialists in the field of audiology diagnose and treat many other diseases, including acoustic neuroma, Meniere's disease, tinnitus, etc.
Senile hearing loss (presbycusis)
Senile hearing loss is a pathological process of age-related death of hair cells of the inner ear, which are responsible for the perception and transformation of mechanical vibrations of the endolymph into electrical impulses, which are subsequently transmitted to the auditory analyzer of the brain. This process can be either hereditary or caused by the influence of unfavorable environmental factors, the main of which is prolonged exposure to high noise conditions. Clinically, senile hearing loss is manifested by a bilateral gradual decrease in hearing up to complete deafness. Once deafness is achieved, the pathological process does not stop. In the absence of irritation of the auditory nerve, its gradual atrophy occurs, which results in the complete impossibility of hearing restoration even with the use of a cochlear implant.
Otosclerosis
Otosclerosis is a disease in which an increase in the size of the auditory ossicles of the middle ear occurs due to their fibrosis and subsequent ossification (ossification). Another manifestation of this disease is the fusion of the stapes and the oval window - the site of transmission of mechanical vibrations amplified by the auditory ossicles to the endolymph located in the lumen of the membranous labyrinth. The causes of the disease have not been definitively established, but it is assumed that there are several of them. First of all, hereditary predisposition is considered. In addition, there is a connection with hormonal changes in the body, since the disease more often manifests itself in women during the onset of menstruation and menopause. Another predisposing factor is chronic inflammation of the middle ear. Symptoms of otosclerosis appear gradually, starting with hearing loss on one side. Later, hearing loss becomes bilateral. In some cases, the disease debuts in infancy due to congenital developmental abnormalities or hereditary diseases associated with metabolic disorders in cartilage and bone tissue.
Tympanosclerosis
Tympanosclerosis is a disease of the middle ear in which connective tissue grows in its cavity, blocking the normal functioning of the sound-conducting apparatus and thus leading to the development of conductive hearing loss. The cause of this disease most often lies in frequent otitis media - inflammatory diseases of the middle ear. However, there are cases of tympanosclerosis without previous otitis, which indicates some hereditary predisposition to this disease. Deformation and rupture of the eardrum leads to significant progression of hearing loss. Clinically, tympanosclerosis is manifested by a gradual deterioration of hearing on one side. However, thanks to the compensatory capabilities of the brain, this symptom is recognized when the function of the hearing organ on the affected side is 30–50% of normal, which is quite deplorable. Bilateral tympanosclerosis is much less common.
Traumatic hearing loss
Traumatic hearing loss is often a unilateral deterioration in auditory perception due to trauma. Speaking about injury, it should be mentioned that this concept includes both a banal mechanical blow and a sudden impact of intense sound or high pressure. In peacetime, traumatic hearing loss can be a consequence of injuries to the temporal bone, in which there is a violation of the tightness and integrity of the tympanic cavity and the structures of the inner ear, as well as the auditory nerve itself. Thus, the localization of the anatomical site where the transmission of sound vibrations is interrupted may be different. The reversibility of hearing impairment depends on the severity of internal damage and is individual for each specific case. In wartime, the percentage of injuries increases significantly, as do the ways in which injuries occur. One of the most common causes of hearing loss and deafness is contusion of the brain when exposed to a blast wave. In this case, the integrity of all parts of the auditory analyzer is violated. First of all, the eardrums rupture, the auditory ossicles are damaged and most of the receptors in the cochlea and labyrinth (the organ of balance) die off. In addition, a sharp change in the position of the head upon contact with a blast wave leads to a direct blow to the brain substance and to a stronger counter-attack from the opposite side. If these effects are exerted on the temporal areas where the hearing analyzers are located, then a sudden loss of hearing occurs, which, however, is gradually restored, but rarely in full. We should also not forget about the possibility of forming a subdural hematoma, which puts pressure on the brain substance. Finally, the possibility of penetrating injury to the tympanic cavity should not be overlooked. Such injuries are usually caused by cutting, piercing or firearms. Their severity depends on the depth of penetration and whether the bony part of the external auditory canal is affected or not. A feature of such wounds is the almost absolute likelihood of infection. Infection, in turn, leads to swelling and increased damage if the necessary treatment is not prescribed as soon as possible. In the case of deep penetration of the traumatic agent, there is a high probability of damage to large blood vessels, nerves and liquor pathways. In all three cases, the prognosis is extremely unfavorable due to the risks of massive bleeding, meningitis, a sharp decrease in intracranial pressure with the development of brain herniation, etc.
Drug-induced hearing loss
Any medicine is a biologically active substance that helps change metabolism in tissues in such a way as to improve the state of health in diseased tissues. However, we should not forget that in addition to the desired effect, medicinal substances have an effect on the tissues of the entire body (when used systemically), and this effect is not always positive. In particular, a temporary or permanent decrease in auditory perception can develop under the influence of a large number of drugs from different groups. The mechanism of their pathogenic influence is not always known, but in this case such information is more scientific than practical. Antibiotics from the group of aminoglycosides (streptomycin, gentamicin, amikacin, etc.) have the most powerful ototoxic (violating the integrity of ear tissues) effect. If used unwisely in adults, these drugs lead to hearing loss; in children they can lead to almost complete deafness. The use of these antibiotics during pregnancy, even in therapeutic doses, contributes to the development of congenital hearing defects in the unborn child. Non-steroidal anti-inflammatory drugs (diclofenac, aspirin, nimesulide, indomethacin, etc.), combined oral contraceptives (femoston, triziston, etc.), psychotropic drugs (amitriptyline, carbamazepine, oxazepam, etc.), representatives of other groups of antibiotics have a less pronounced ototoxic effect. (vancomycin, ristomycin, polymyxin, etc.). Many anticancer drugs (cisplatin, cyclophosphamide, methotrexate, etc.) also have a wide range of side effects, including ototoxicity. The list of drugs with weak and moderate ototoxic effects is even more impressive.
Meniere's disease
Meniere's disease is a fairly rare disease in which there is an increase in endolymph pressure inside the membranous labyrinth of the inner ear. The causes of the disease are numerous, which means that there is no certainty regarding its etiology. Among the most likely causes are chronic inflammatory processes, a genetic predisposition to an imbalance between the formation and utilization of endolymph (fluid circulating in the inner ear), etc. Clinically, the disease is manifested by progressive hearing impairment, first on one side, and then on the other, attacks of loss of coordination and tinnitus. In some cases, autonomic disorders associated with imbalance (hot flashes, nausea, dry mouth, headaches, etc.) appear.
Anomalies in the development of the hearing organ
Congenital abnormalities of the hearing organ can cause hearing loss and deafness. The reason for their formation may be various chromosomal aberrations (errors, disorders) that appear as a result of a certain incompatibility of the genomes of partners or the influence of external factors (taking ototoxic medications, ionizing radiation, etc.). Some of these anomalies can be corrected, while others cannot yet be corrected. The following abnormalities in the development of the hearing organ can lead to hearing loss and deafness:
- agenesis (underdevelopment) of the external auditory canal;
- atresia of the external auditory canal (blindly ending external auditory canal);
- agenesis of the auditory ossicles;
- cochlear agenesis;
- fusion of the oval window, etc.
Pediatric audiologist
This is a doctor whose competence includes identifying ailments and correcting hearing in children from birth.
During diagnosis, techniques are used that involve monitoring and studying reflexes or reactions. In addition, the clinician will:
- measurement of pressure in the middle ear area;
- assessment of eardrum activity;
- fixation of acoustic resistance in the external auditory canal.
Parents should pay attention to hearing problems in children, especially schoolchildren and newborn babies. Timely seeking help from such a clinician will allow you to avoid the development of serious complications, diagnose the disease in the early stages and begin therapy as early as possible.
How does an appointment with an audiologist go?
At the first visit, the doctor should do the following:
- study of medical history;
- survey;
- hearing acuity test;
- examination of the ear canal.
Based on the information received, the appointment with the audiologist continues with the appointment of therapy or additional tests. It can be:
- tympanometry – assessment of hearing at different frequencies and the condition of the auditory tube;
- electrocochleography – used in case of ear congestion, dizziness;
- otomicroscopy;
- reflexometry;
- audiometry.
The doctor may advise the patient to consult with specialists in other fields - a neurologist, pediatrician, surgeon, cardiologist. This is required to exclude diseases whose symptoms include hearing disorders. A common indication for such a recommendation is the presence of tinnitus; this sign may indicate problems with the spine or blood vessels.
How does an audiologist test your hearing?
For a long time, there was only one way to determine the quality of hearing - the doctor whispered a word and asked the patient to repeat it. Now the method is also used, you can even see how an audiologist tests a child’s hearing using it, but there are also alternative approaches. They are used for repeated examinations and for diagnosing the hearing of young children. In the latter case, measures are taken to:
- studying reflexes;
- measuring middle ear pressure;
- determination of acoustic resistance in the external auditory canal;
- analysis of eardrum activity.
To avoid having to find out who the audiologist is and make an appointment with him, you need to take precautions. Even if there are no hearing problems, there is no need to test the limits of your own endurance. It is also undesirable to neglect regular examinations; an audiologist-otolaryngologist can restore hearing or significantly improve the quality of life, but it is better not to give him unnecessary reasons to work.
How to preserve your hearing?
An audiologist will not only help you eliminate any problems that have arisen and select the appropriate hearing aid, but will also tell you how to maintain your hearing into old age.
- Treatment.
A common runny nose can result in complications of the throat and ear, and if not given enough attention, it can lead to hearing impairment. - Medicines.
Some drugs, especially antibiotics, can worsen the condition of the hearing organs if used uncontrolled. It is better to consult a specialist before taking such drugs. - Protection.
When visiting a swimming pool or living by the sea, it is advisable to protect your ears from water. Earplugs or cotton swabs soaked in Vaseline or vegetable oil will do. - Noise.
Noise over 80 decibels is dangerous; if you are constantly in places where the threshold is exceeded, you need to use special means. - Pressure.
On an airplane, during landing and takeoff, you need to open your mouth to equalize the pressure, and after the flight, a short stay in silence will be useful. If you are interested in diving, you should not neglect the basic rules so as not to get barotrauma. - Sulfur plugs.
It is better to entrust their removal to a specialist. - No overload.
The hearing organs are able to adapt to external conditions; if you are constantly in an area of increased noise, the sensitivity of the auditory analyzer will decrease.
Several specialists are involved in the diagnosis and treatment of pathologies related to the hearing organs. One of them is an otolaryngologist (ENT), a general practitioner. If a patient has problems with hearing loss, he should consult a more specialized specialist. Audiologist - who is he, what does he treat? This doctor has professional knowledge regarding the physiology of the hearing organs and their work.
When to see an audiologist
The reasons for contacting an audiologist may be:
- signs of hearing loss - the need to turn up the volume of the TV, the presence of ringing in the ears, loud speech (according to the comments of others), the need to strain and ask again during a conversation;
- noise in ears;
- dizziness, problems with coordination and balance;
- the presence of chronic otitis (an audiologist treats this pathology in remission, and in case of exacerbation of otitis, you need to contact an ENT specialist).
A hearing test is also recommended for people who:
- have experienced vibration and hearing stress (from 85 dB) in connection with their professional activities for more than 5 years;
- suffered barotrauma, traumatic brain and acoustic injuries;
- suffer from cerebrovascular accidents;
- have a hereditary tendency to deafness and hearing loss.
For early detection of deafness in many countries of the world, newborns are screened using special equipment on the 1st or 2nd day of life.
If screening has not been carried out, parents should pay attention to whether the child has a reaction to loud sounds.
Children born to women who had influenza or rubella during pregnancy, took certain medications, or were exposed to chemical factors require special attention.
You should contact a pediatric audiologist for a hearing test if your child:
- suffered hypoxia during fetal development;
- suffers from hemolytic disease of the newborn;
- suffered an infectious disease in the first year of life, since during this period of development nervous tissue is susceptible to the effects of viruses;
- does not make any sounds (no cooing, babbling at 3-4 months, etc.).
Children with abnormalities in the structure of the temporal bone may suffer from congenital deafness.
Risk factors for hearing loss include frequent exposure to noise (listening to music on headphones, etc.), head injuries, severe otitis media, abuse of antibiotics that negatively affect the nervous system, and diabetes.
What symptoms should you consult an audiologist for?
Regular preventive examinations by an audiologist are necessary for people who work in high-noise environments. Most often these are employees of industrial enterprises. Fans of loud music with headphones and patients who have already suffered from inflammation of the hearing organs should also regularly visit a specialist.
It is these groups of people who are at risk of decreased hearing acuity, and timely consultation with a doctor will help to notice and prevent complications in time.
Hearing pathologies can develop after diabetes mellitus, metabolic disorders, cardiovascular diseases, mechanical injuries to the head, or the prescription of a course of antibiotics. Attend comprehensive examinations at least 1-2 times a year to fully control your own body.
What symptoms should you see a doctor for? Any changes in hearing are a serious reason to visit a specialist. If you begin to have difficulty hearing others, TV, doorbells or telephone calls, immediately contact an audiologist. If you have to lean/turn towards your interlocutor to better hear the dialogue, it means that a pathological process has started in the organ of hearing, which affects the quality of life.
Ear congestion that does not go away on its own should also raise suspicion and lead to consultation. Do not delay going to the doctor, as the condition may worsen.
At best, the patient will feel like there is a plug stuck in the ear, which has little effect on hearing; at worst, the person will experience hellish pain in the ear, which cannot always be relieved with medication.
A doctor not only for adults
As for children, they should be contacted by an audiologist if speech impairment or partial hearing impairment is observed. Constant discharge from the auricle is also a reason to contact an audiologist. Diagnosis for the youngest patients is the same as for adults.
An appointment with any audiologist begins with a conversation, when the doctor asks questions. After this, the ear is examined from the outside and inside. This is followed by audiometry, the results of which are the basis for prescribing medication or surgical treatment. Often, an audiologist, in addition to medications, uses physical therapy for treatment.
The audiologist treats patients with Meniere's disease (inflammation of the middle ear), otometry, acoustic neuroma, and senile hearing loss. These are very serious diseases that require mandatory treatment. This is what the doctor treats.
Remember that timely consultation with a doctor is the key to preserving your hearing in the future. You need to understand that the ears are one of the main organs. With the help of ear analyzers, a person receives most of the information about the outside world. Significant hearing impairment can cause significant discomfort to any person, so this issue should be taken as seriously as possible. That's who this narrow specialist is.
Medical specialties are diverse, so not everyone can tell you what an audiologist does, who he is, and in what situations you should contact him. This doctor is not available in every clinic, so you often find out about the need to visit him by accident.
Diagnostic methods and treatment features
During the first examination, the audiologist examines the clinical picture of the disease and the general condition of the patient. After this, the doctor begins diagnostics. He determines hearing acuity, examines the ear canal and conducts a detailed survey regarding the current state of health. Additionally, audiometry or tympanometry may be prescribed.
Audiometry – determination of auditory sensitivity to sound waves of various frequencies. Tympanometry - air pressure on the ear canal to study the function of the middle ear, the degree of mobility of the eardrum and the conductivity of the auditory ossicles.
In more advanced or severe cases, the doctor selects specific diagnostic methods - electrocochleography, otomicroscopy, reflexometry.
Based on the information received, the audiologist prescribes therapy. For some patients, a week of medication treatment will be enough, while others will need surgery and the selection of a hearing aid. The main thing is not to self-medicate, trust your doctor and strictly follow his recommendations.
Preventive measures
To avoid the development of diseases or complications, audiologists recommend undergoing diagnostic tests 1-2 times a year. For congenital or past diseases, the number of visits is varied by the doctor on an individual basis. Particular attention should be paid to newborn children and schoolchildren.
Delayed speech development, lack of response to certain sounds, and frequent tears of a child for no apparent reason may indicate problems with the hearing aid.
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Be sure to take your baby to the doctors and do not delay the appointment. The sooner a specialist identifies the problem, the faster and more effectively it will be possible to get rid of it.
If you live in a noisy environment, try to eliminate it as much as possible. Install soundproof windows, rarely open them, or find a place to live in a quieter area. Remember that excessive noise will definitely affect not only the hearing aid, but also the psyche.
Audiologists highlight one important rule - never tolerate pain. The body clearly makes it clear to you that pathological processes are occurring inside and they urgently need to be stopped. Don't assume that the pain is temporary and that after a few hours or days the body will deal with the infection on its own. Such carelessness can cause irreversible consequences for the body, complete or partial hearing loss. Modern medicine can correct any hearing impairment and bring quality of life to a new level. Trust your doctors and stay healthy.
How is rehabilitation carried out?
In cases where the hearing loss is incomplete, it is possible to compensate for it using special technical devices. We are talking about hearing aids. It is the audiologist's #1 tool for compensating for hearing loss. In this case, the doctor of this specialty not only makes the appropriate prescription, but also helps the patient choose a suitable hearing aid. In addition, the doctor is able to provide assistance not only in installing such a device, but also in setting it up.
When deafness is congenital or irreversible, there is no point in using any technical devices. In this case, the audiologist’s main tool is lip reading and sign language. Possession of these skills allows patients with complete hearing loss to communicate normally at least with those people who also possess them. In addition, lip reading helps deaf people understand what a healthy person is saying.
What problems can an otolaryngologist handle on his own?
Currently, doctors in this specialty have every opportunity to avoid distracting audiologists with relatively mild hearing-related pathologies. First of all, we are talking about various types of otitis media. Its simplest form, which not only an otolaryngologist, but also an ordinary general practitioner should be able to cope with, is catarrhal. It will require the use of special drops for the ears and vasoconstrictors for the nose.
Another problem that any otolaryngologist can handle is cerumen plugs. Moreover, the procedure for removing them will take no more than a few minutes. An ENT specialist can also help a person get rid of a foreign body that has entered the ear canal.
These pathologies are the most common causes of hearing loss. It is because of them that many people visit a specialist such as an audiologist. Who he is is usually known only to those who really have serious hearing problems.
Hearing care in the West
In developed countries (USA, Canada, Western European countries), staffing for hearing care is carried out by a whole group of specialists competent in various fields of medical knowledge. There are several options for naming specialties related to the correction of natural and acquired hearing impairments:
- Hearing aid dispensers.
- Hearing aid practitioners.
- Audiologists.
- Audiologists.
- Otolaryngologists, etc.
The profession of “Hearing Aid Dispenser” as a full-fledged specialty appeared in the West in the early 80s of the last century, when the number of people in need of hearing correction began to far exceed the number of doctors with the required specialization.
Over the past three decades, qualification requirements for these specialists have been developed and put into practice, and methods for their training have been developed and unified.
Audiologists are highly specialized doctors. Their area of responsibility is diagnosing and determining an effective method of treating pathologies of the auditory organs (this means not only the ear, but the entire hearing system as a whole). Reasons for contacting an audiologist may be:
- Hearing loss in one or both ears.
- Noise in the ear.
- Problems with identifying the direction of sound.
- Deterioration of speech intelligibility of interlocutors in noisy environments.
- Any other “oddities” or inconveniences associated with hearing
The following specialties are subject to compulsory licensing in developed countries:
- Hearing aid dispenser.
- Audiologist-rehabilitation specialist (his duties include teaching the patient to live with a hearing aid).
- Assistant audiometrist.
Thus, the high quality standards of hearing care in Western countries are determined not only by generous material equipment, as we are accustomed to thinking, but also by a thoughtful approach to personnel training.
The content of the activities of “their” specialists provides for the mandatory, not “for registration”, mastering of:
- Anatomical and physiological aspects.
- Fundamentals of acoustics and psychoacoustics.
- Psychology.
- Information technologies.
- As well as legal aspects of hearing care.
Another important point: due to the dynamic development of the hearing aid industry, generations of hearing aids from leading manufacturers change every 1-2 years.
This forces specialists to constantly update their knowledge, skills and abilities to navigate the increasingly technically complex and progressively developing range of hearing aids.
Obviously, the high level of professional training of Western specialists is explained by a clear understanding on the part of the governing health authorities of the “borderline” nature of hearing care, which is a branch not only of medicine, but of a number of disciplines:
- Psychology.
- Psychotherapy.
- Pedagogy.
- Physicists.
- Microelectronics.
- Chemistry.
- Programming.
- Marketing, etc.
Hearing care in Russia
In our country, hearing aids are provided to all those in need, both in the public and private healthcare systems, by specialists with higher medical education in the specialty of audiology-otolaryngology.
Today, there is no doubt that neither educational programs in this area nor the organization of training in this specialty can provide the training of specialists who, taking into account modern requirements for hearing care, could be called highly qualified.
In Russia, the competence of an audiologist includes the diagnosis and treatment of the following pathological conditions:
- Tubootites
- Otosclerosis
- General hearing loss
- Noise in ears
- Sensorineural hearing loss of various types
- Meniere's disease and other types of labyrinthopathy
- Acute and chronic otitis media
- Labyrinthitis
- Acoustic neuroma.
Moreover: Russian legislation and hearing aid manufacturing companies do not put forward any qualification or other requirements for specialists involved in hearing care.
Here again it is appropriate to cite the example of developed countries, where the option of supplying hearing aids and accessories to them to companies that do not have a license to carry out these works and services is, in principle, impossible.
In our country, hearing care is carried out by audiologists, whose qualifications often do not meet modern requirements. This is not their fault, but an objective fact related to the nature of their professional training
Therefore, many audiologists try to improve their qualifications as much as possible through courses, trainings, attending presentations and specialized classes, which are often conducted in branches of world-famous hearing aid manufacturers. However, many doctors from government institutions do not have the opportunity to attend such events for several reasons:
- Lack of free time.
- Inability to arrive at the location of the training or presentation due to its remoteness.
- Financial difficulties.
- Reluctance to improve your skills.
The consequence of this is a highly ineffective expenditure of budget funds allocated from the federal and regional budgets for the purchase of hearing aids under various preferential programs. The lion's share of such devices is simply given to patients either without any selection at all (not to mention a trial period), or through unqualified selection.
Unprofessional use of hearing aids, even with all their high quality today (which, by the way, is confirmed, among other things, by their price), creates in users a feeling of discomfort and dissatisfaction with the level of quality of the service provided to them
In developed countries (in this case, unfortunately, we are forced to leave Russia out of the equation), the provision of hearing aids to those in need is strictly controlled by the state through a harmoniously functioning system of public-private partnerships. The system of education and targeted training, sales and service of hearing aids are the prerogative of several professional associations. In turn, the issues of issuing licenses for relevant types of activities, as well as multi-stage quality control of the work performed and services provided in the field of hearing care are the exclusive domain of the state. What do we have? The imperfection of the regulatory framework (including the lack of clear professional standards), which results in an acute problem of staffing this important social service, puts our citizens suffering from hearing loss in a worse position in comparison with their colleagues in misfortune from developed countries.
I am glad that there is still a way out of the situation. Many private clinics and hearing centers (YU-MED among them) began to cooperate directly with representatives of leading hearing aid manufacturing companies. Thus, audiologists receive:
- Up-to-date information about the possibilities of new technologies in the field of hearing aids.
- Opportunity to exchange experience with foreign experts.
- Attend professional trainings and other events aimed at increasing the qualification level.
Only the organization of additional periodic retraining of audiologists can ensure the training of specialists who, taking into account modern requirements for hearing care, could be called highly qualified.
Recommendations from audiologists
Audiologists recommend their patients and all people who do not have hearing problems to follow simple rules:
- avoid exceeding the hearing threshold;
- Do not under any circumstances ignore the first symptoms of hearing loss, which are noise and ringing in the ears;
- contact specialists in cases of delayed speech development of a child;
- undergo regular preventive examinations not only with an otolaryngologist, but also with clinicians of other specializations.
Only early detection of pathology will help to avoid complete hearing loss and the use of a hearing aid.
When is specialist consultation necessary?
It is necessary to visit a clinic where an audiologist-otolaryngologist works if the following phenomena occur:
- hearing loss;
- difficulty in determining the direction of sound;
- difficulty understanding speech;
- constant questioning of the interlocutor;
- poor understanding of words during a telephone conversation;
- tension during a conversation;
- the need to increase the volume of the TV or radio.
The progressive hospital uses modern diagnostic methods (audio and tympanometry), guaranteeing painless and effective procedures. An audiologist-otolaryngologist often advises seeking advice from other specialists (surgeon, cardiologist, pediatrician) to identify diseases that provoke hearing problems.