Paroxysmal tachycardia
(Greek paroxysmos irritation, excitement; tachycardia) - a paroxysmal increase in the number of heart contractions caused by pathological circulation of extrasystolic excitation or pathologically high activity of the focus of heterotopic automatism in the heart. Heart contractions during Paroxysmal tachycardia are strictly rhythmic, their frequency usually ranges from 120 to 220 per 1 minute, in children it can reach 260 per 1 minute, the duration of the attack is from several seconds to several days, and sometimes weeks, and the frequency of contractions is not is changing.
The clinical picture of Paroxysmal tachycardia was described in detail by Bouveret (L. Bouveret, 1899) and Hoffmann (J. Hoffmann, 1900), and therefore this syndrome was previously called Bouveret-Hoffmann disease.
Based on the location of the ectopic focus of automatism, which is the pacemaker during paroxysmal tachycardia, its three forms are distinguished: atrial, atrioventricular junction and ventricular. The first two forms are called supraventricular paroxysmal tachycardia. Most cardiologists do not recognize the occurrence of Paroxysmal tachycardia under the influence of impulses emanating from the sinus node (sinus Paroxysmal tachycardia), although there is evidence of the possible localization of the source of impulses in the tissues directly adjacent to this node.
The boundary between group extrasystole and short attack of P. t. is drawn conditionally. It is generally accepted that if the number of ectopic contractions following each other in a rapid rhythm is more than three, then we should no longer speak of a group extrasystole, but of a short paroxysm of tachycardia. Some cardiologists consider paroxysm of tachycardia to be a series of a larger number of ectopic contractions.
In some cases, short attacks of P. t., consisting of 3-6 ectopic contractions, alternate with sinus rhythm, sometimes almost constantly, for several months and even years. Such cases are usually called the recurring form of P. t. Sometimes ectopic tachycardia becomes permanent; in these cases it is usually interrupted by short periods of sinus rhythm (so-called persistent tachycardia).
Causes of paroxysmal tachycardia, mechanism of development
Etiology and pathogenesis
Paroxysmal tachycardia, especially at a young age, is often functional in nature. The immediate cause of attacks is usually stress reactions - mental or physical.
It is known that stress reactions are accompanied by an increase in the content of adrenaline and norepinephrine in the blood. According to A.
P. Golikova et al., during an attack of paroxysmal tachycardia or shortly before it, the content of catecholamines in the blood increases significantly; during the interictal period this indicator normalizes.
The authors believe that an increase in the content of catecholamines in the blood, along with the increased individual sensitivity of ectopic pacemakers to them, is one of the pathogenetic mechanisms of paroxysmal tachycardia.
Causes and mechanisms of occurrence
In most cases, paroxysmal tachycardia is a consequence of heart pathology.
Paroxysmal tachycardia, like other rhythm disturbances, can be associated with heart disease, non-cardiac pathology and any external influences. The most common causes of their occurrence are:
- structural and metabolic changes in the myocardium (coronary heart disease, cardiomyopathies, myocarditis, heart defects, arterial hypertension, tumors and heart injuries, chronic cor pulmonale, amyloidosis);
- diseases of other organs and systems (gastrointestinal disorders, endocrine pathology, damage to the central nervous system);
- physical and chemical influences that disrupt cardiac activity (hypoxia, irradiation, exposure to low and high temperatures, arrhythmogenic effects of certain drugs);
- intoxication;
- increased sensitivity to alcohol, nicotine, caffeine, etc.
Each type of paroxysmal tachycardia has its own development mechanisms. Among them there are 2 main ones:
- repeated course of the excitation wave (re-entry);
- increased automaticity of cells of 2nd and 3rd order ectopic centers.
Definition and types
The term "tachycardia" indicates an increased heart rate, which corresponds to 100 beats per minute or more.
In this regard, the definition of paroxysmal tachycardia is a sudden attack of rapid heart rate from 100 to 250 beats per minute, without loss of regularity. In this situation, it is very important to know how to help the patient.
This disease is listed in ICD 10 - the International Classification of Diseases, 10th revision and has code I00-I99 / I30-I52 / I47.
An attack of paroxysmal tachycardia can last from several minutes to a couple of days.
At the same time, the rhythm is maintained throughout the entire duration of the attack, which is the main sign of this condition.
Doctors distinguish several types of this arrhythmia:
- Supraventricular (supraventricular) tachycardia
There is also a classification here:
- Atrial paroxysmal tachycardia. The ectopic (additional) focus of excitation is located in the atria.
- Atrioventricular. The ectopic node is located in the area of the atrioventricular junction.
The ectopic focus is localized in the tissues of the ventricles. It also happens:
- Persistent ventricular tachycardia. During the period of taking an ECG, its duration is recorded at 30 seconds or longer.
- Unstable. On the ECG its duration is less than half a minute.
It is ventricular paroxysmal tachycardia that is considered the most dangerous, since it can cause complete cardiac arrest. Depending on the course, the following types of pathology are distinguished:
- acute form;
- constantly returnable;
- continuously relapsing.
The danger of recurrent and recurrent forms is that frequently repeated attacks cause myocardial depletion and the formation of heart failure.
Paroxysmal ventricular tachycardia and its features
Paroxysmal tachycardia is a sudden attack of rapid heartbeat. It may not last long, just a few seconds.
In some cases, the illness drags on for a couple of days. This type of arrhythmia is characterized by a heart rate of up to 220 beats per minute.
- Types of paroxysmal tachycardia
- Paroxysmal ventricular tachycardia
- Classification of ventricular paroxysmal tachycardia
- Causes of the disease
- Symptoms of the disease
- Emergency relief of an attack
- Diagnosis of ventricular paroxysmal tachycardia
- Complex therapy
- Disease prognosis
- Preventive measures
In some cases, the illness drags on for a couple of days. This type of arrhythmia is characterized by a heart rate of up to 220 beats per minute.
Reasons for development
The pathogenesis of the disease has not been reliably elucidated. The main reasons causing paroxysm of tachycardia include:
Enter your pressure
Move the sliders
- increased tone of the sympathetic part of the NS (nervous system);
- prolonged stress;
- disturbances in the functioning of organs and their systems;
- osteochondrosis;
- neurosis;
- dystrophy of the heart muscle (heart disease, cardiosclerosis, infectious diseases, etc.);
- severe alcohol intoxication;
- negative impact of toxic substances;
- congenital and acquired cardiac anomalies;
- narcotic substances;
- excessive physical activity;
- smoking;
- high blood pressure.
The reasons why paroxysmal tachycardia appears are:
- myocardial pathology;
- diseases of internal organs;
- psycho-emotional factors;
- idiopathic - without identified causes.
Heart disease usually accompanies attacks of tachycardia and is characteristic of the following diseases:
- ischemia;
- hypertension;
- heart defects;
- heart attack.
Inflammatory, necrotic phenomena in the myocardium, congenital disorders, for example the bundle of Kent, can also cause paroxysmal tachycardia.
Kent's bundle - additional muscle fibers running between the atrium and ventricle or near the cardiac septum. The cardiac impulse can pass through them in a pathological manner, causing changes in the conduction system.
The cause of the disease lies in ectopic excitation of the ventricular parts of the conduction system of the heart. This defect can develop under the influence of external influences or as a hereditary factor.
At an early and young age, attacks can be caused by stress, physical and emotional stress. In old age, the disease is caused by multiple damage to the heart muscle, previous heart attacks, and coronary heart disease.
And although supraventricular (supraventricular) paroxysmal tachycardia is sometimes not a consequence of organic heart damage, it is still considered a deviation from the norm. That is why there are always reasons that caused such a violation of heart rate.
Advice! After the first attack of paroxysmal tachycardia, a full medical examination is prescribed. This allows us to identify the causes of pathology.
The main reasons include:
- The presence of several paths for conducting an impulse. This can be a congenital pathology, as well as acquired.
- Overdose of cardiac glycosides (digoxin, strophanthin, corglycone). An attack can also be caused by taking certain antiarrhythmics, such as quinidine or propafenone.
- Frequent stress, as well as neurasthenia and neuroses.
- Taking alcohol and drugs.
- Diseases that do not affect the functioning of the cardiovascular system: stomach diseases (ulcers and gastritis), cholecystitis, liver and kidney failure.
- Excessive content of cardiotropic hormones. The cause may be hyperthyroidism (increased total amount of triiodothyronine), as well as in phaechromacytoma (increased content of stress hormones - norepinephrine and adrenaline).
Paroxysmal ventricular (ventricular) tachycardia
Here, organic damage to the heart is always diagnosed, which becomes the cause of the attack:
Content
Paroxysmal tachycardia: causes
Every person has experienced the feeling of a racing heart throughout their life. This also occurs in healthy people during physical activity, emotional stress, and increased body temperature. Such tachycardia is always sinus and stops on its own.
Treatment tactics for paroxysmal ventricular tachycardia
Ventricular paroxysmal tachycardia is an attack of increased contractions of the ventricles of the heart, which begins and ends suddenly in most cases. At the same time, the rhythm remains correct, sinus, therefore such tachycardia is sinus tachycardia of the heart.
Tachycardia develops for many reasons, some of which are a normal physiological reaction and should not cause concern. For example, increased heart rate within reasonable limits after physical activity or during emotional stress, when the heart rate quickly returns to normal after the effects of these factors are eliminated.
Tachycardia is also usually observed when the temperature rises due to colds and some other diseases. There is even a pattern - with an increase in body temperature by 1 degree, the pulse, depending on the constitution and age of the patient, increases by 6-10 beats. The cause for concern is, first of all, cases when tachycardia appears at rest. In such cases, to decide how to get rid of tachycardia, a full examination is necessary.
Ventricular paroxysmal tachycardia is the most unfavorable among all life-threatening arrhythmias (which include both other ventricular and paroxysmal supraventricular tachycardia).
Ventricular paroxysmal tachycardia is the most unfavorable among all life-threatening arrhythmias (which include both other ventricular and paroxysmal supraventricular tachycardia).
Causes and mechanism of development of tachycardia
The reasons why rhythmic disturbances in the functioning of the heart muscle can occur under certain conditions are:
- serious diseases or pathologies of organ development;
- side effects of medications;
- repeated emotional experiences;
- leading an unhealthy lifestyle;
- illnesses that caused complications.
Contributing factors also include cardiovascular surgery, electrolyte disturbances and genetic diseases.
Several mechanisms can take part in the development of ventricular arrhythmia.
- Repeated input of an excitation wave, it is localized in the working muscle layer of the ventricles or conduction system.
- An additional source of excitation of increased automaticity.
- Source of electrical impulses of trigger activity.
Sometimes the conduction system also participates in the formation of the re-entry loop. This form is called fascicular. In most cases, it is diagnosed in boys and young men and is classified as idiopathic.
All types of arrhythmic conditions manifest themselves in basically the same way. The disorder is diagnosed primarily through an electrocardiogram. Symptoms of paroxysmal ventricular tachycardia determine the direction of treatment. Most often their role is played by:
Mechanism of development of ventricular tachycardia
Science knows three mechanisms for the development of ventricular paroxysms:
- Re-entry mechanism. This is the most common variant of rhythm disturbance. It is based on the re-entry of the excitation wave of a region of the myocardium.
- Pathological focus of increased activity (automatism). In a certain area of the heart muscle, under the influence of various internal and external factors, an ectopic source of rhythm is formed, causing tachycardia. In this case, we are talking about the location of such a focus in the ventricular myocardium.
- Trigger mechanism. With it, myocardial cells are excited earlier, which contributes to the emergence of a new impulse “before the due date.”
In order to determine the type of paroxysmal tachycardia and make sure that it is the ventricular form, several diagnostic methods are sufficient. The main one is electrocardiography (ECG).
Classification
Among ventricular paroxysmal tachycardias, unstable and stable forms are distinguished. Unstable are characterized by the presence of three or more ectopic QRS complexes in a row, recorded within a period of no more than 30 seconds. Such paroxysms have no effect on hemodynamics, but increase the risk of ventricular fibrillation and sudden cardiac arrest. Sustained ones last more than 30 seconds and are accompanied by hemodynamic changes up to arrhythmogenic shock and acute left ventricular failure, resulting in a high risk of sudden death. Such tachycardia at low pressure is even more dangerous, since the human body tries to compensate for this condition with a more rapid pulse, which increases the likelihood of developing heart failure.
The treatment tactics for tachycardia, as well as one of its forms (paroxysmal tachycardia), depend on the presence or absence of heart failure.
Diagnostics
A cardiologist deals with heart diseases. However, the doctor may refer the patient to other specialists. The choice depends on the cause of GPT.
In order to prescribe adequate treatment, it is important to identify the main cause of tachycardia. To do this, the most comprehensive examination is carried out:
- Initially, the doctor collects anamnesis and examines the patient. The patient should talk about the frequency of tachycardic attacks and other symptoms that appear. To identify risk factors, the patient is asked about bad habits and lifestyle. The history of previous diseases and the presence of chronic pathologies and hereditary factors must be studied. The cardiologist measures blood pressure, examines the patient’s skin, and listens to the rhythm of the heartbeat.
- Collection of urine and blood for general and biochemical analysis. The level of substances in the body is analyzed.
- Holter monitoring. The device is attached to the patient's body for 24 hours. During this time, the heart rate is recorded.
- Electrocardiogram and echocardiography. The structural state of the heart, conductivity, and contractility are studied.
- To identify IHD, stress tests are performed.
- Electrophysiological examination evaluates the mechanism of tachycardia.
- To detect the affected area, a radionuclide study is carried out.
- To assess the condition of the circulatory system, angiography or coronary angiography is performed.
Conservative measures. For successful treatment of ventricular paroxysmal tachycardia, the patient must change his lifestyle. First of all, bad habits are eliminated. The doctor will prescribe a set of therapeutic exercises and develop an individual diet. A person should avoid stressful situations and other factors that can trigger a tachycardia attack.
Symptoms and signs
Trembling in the arms and legs is one of the symptoms of the disease.
In the intervals between paroxysmal attacks, the patient feels completely healthy. The description of the chronic course of the disease will be symptoms depending on the type and form of the pathology. Paroxysmal tachycardia has the following symptomatic features:
- trembling in the arms and legs;
- sudden loss of body weight;
- increased irritability;
- fragility and hair loss.
If the cause of paroxysmal tachycardia is a congenital or acquired heart defect, or chronic heart failure, the following symptoms appear:
- severe shortness of breath;
- increased fatigue;
- noise in ears;
- attacks of nausea;
- flatulence;
- increased sweating;
- fainting;
- heart pain.
The attack is characterized by tremors in the chest and subsequent palpitations. Patients feel physically how their heart is pounding.
In this case, severe weakness and shortness of breath are felt, vision and speech may be impaired, and sensitivity in the limbs may be lost. Paroxysmal ventricular tachycardia can cause loss of consciousness.
Clinical death may occur, in which there is no pulse and breathing.
Paroxysmal tachycardia emergency care
Providing emergency care involves quickly establishing, at least approximately, the cause of paroxysmal tachycardia. Moreover, this is very important during the first attack of tachycardia paroxysm in the patient’s life. Based on the medical history, examination of its status, ECG study, a verdict is made about the presence of diseases that provoked the attack, or their absence, and psycho-emotional stress is not excluded.
First of all, antiarrhythmic therapy is carried out with mandatory monitoring of cardiohemodynamics. If the antiarrhythmic drug is ineffective, repeated administration can be performed only after thirty minutes. If this antiarrhythmic method of administering up to three drugs does not bring positive results, then electrodefibrillation of the heart is started to prevent a progressive increase in heart failure or coronary heart failure, as a result of a sharp drop in blood pressure.
With supraventricular paroxysmal tachycardia, at the very beginning they try to provide emergency assistance using basic “vagal” tests. However, this method cannot be used for older people or those with high carotid sinus syndrome. In this case, perform a sequential massage of this sinus for no more than 15 seconds, first on the right and then on the left. In this case, it is necessary to monitor the work of the heart to exclude asystole.
To perform the Valsalva maneuver, the patient must inhale as much air as possible and then exhale forcefully while closing the mouth and nose and keeping the abdominals tense. It is advisable to repeat this up to three times.
In addition, you can try pressing on your closed eyes for eight seconds, however, this method should be excluded when helping children to prevent retinal detachment.
In some cases, you can artificially induce vomiting. But if all these manipulations are ineffective, Verapamil is administered intravenously. If the attack does not stop, this drug is re-administered after five minutes.
If patients took adrenergic blockers during a daily attack, then Verapamil is not used, since a sudden stop of blood circulation is possible.
Further emergency care consists of the patient taking Obzidan under the tongue thirty minutes after the previous drug has failed. If necessary, Obzidan is taken after two hours.
This technique is a basic one, giving a positive result in 80% of cases.
Symptoms
The main difference between an attack of paroxysmal tachycardia is its sudden and acute onset. The duration of the attack ranges from several minutes to several days.
Sometimes before an attack, Fr. A person anticipates the onset of an attack - dizziness, weakness.
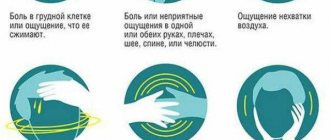
During it, the patient experiences the following symptoms:
The disease begins to manifest itself with the following signs:
- first, the patient experiences a sharp painful jolt in the chest area;
- after a short pause, the number and speed of shocks begin to increase;
- if there is a correct heart rhythm, the heart rate begins to increase rapidly, exceeding the number of 140 beats;
- taking into account the complexity of the attack, the number of blows can be more than 220;
- At the same time, the patient feels severe dizziness and there is noise in the ears;
- Quite often, patients note a strong contraction of the heart muscle;
- in rare cases, symptoms such as aphasia and hemiparesis appeared;
- sometimes during an attack such unpleasant symptoms appear as severe sweating, a feeling of nausea, active release of gases and a slight increase in body temperature;
- As soon as the attack is stopped, the patient notes the release of a significant amount of clear urine.
Possible symptoms of tachycardia
Attention! This pathology always begins and ends completely unexpectedly, and the attack can last from a couple of seconds to several days.
Once the attack becomes prolonged, patients may also experience fainting and a significant drop in blood pressure. But conditions in which the number of heart beats exceeds 180 beats per minute are especially dangerous.
With this type of paroxysmal tachycardia, ventricular fibrillation may begin.
Also, in severe conditions, patients experience swelling of the lungs, cardiogenic shock, poor nutrition of the heart muscle, which leads to the development of angina pectoris and myocardial infarction.
Attention! If patients have cardiac pathologies, emergency medical care is required. In such patients, the attack is always of a complicated type, which can cause rapid death.
Physiology of tachycardia
The main symptoms indicating PT are related to the functioning of the heart. The attack begins suddenly and ends just as unexpectedly.
The patient initially feels a shock in the heart area, after which the rhythm begins to increase.
The frequency can vary from 100 to 250 beats per minute, while the heartbeat is rhythmic.
In addition, symptoms of disturbances in the functioning of the nervous system may be observed.
The patient may suffer from dizziness, excessive agitation, darkening of the eyes, trembling movements in the hands and convulsions.
Symptoms of neurological disorders may also appear. Patients often experience increased sweating, flatulence, nausea (vomiting), and increased peristalsis.
Pallor of the skin, swelling of the jugular veins, and rapid breathing may be noted. One of the important signs is frequent urination.
After a couple of hours it stops. The color of urine is unsaturated, and its density is very low. Prolonged paroxysmal tachycardia can lead to weakness, fainting, and decreased blood pressure.
Before the end of the attack, a “freezing” occurs in the heart area, the condition returns to normal, breathing and heartbeat are leveled out.
Patients who have heart pathologies suffer attacks much more severely.
An attack of paroxysmal tachycardia is characterized by an acceleration of heart rate to 120-250 beats per minute. The duration of the attack ranges from a couple of seconds to several hours and days. Depending on the clinical manifestations, two types of paroxysms are distinguished:
- essential;
- extrasystolic.
Prognosis and Prevention
The prognosis depends on the form of P. t., on the underlying disease against which it arose, and the duration of the attack. The prognosis for atrial P. t. is most favorable in cases where heart disease is not detected. The most severe prognosis is for cases of ventricular P. t. in patients with coronary heart disease, especially myocardial infarction. The prognosis is also unfavorable for long-term P. t. If the attack cannot be stopped within ten days or is possible, but only for a short period, then death is possible.
Prevention. Prevention of relapses of P. t. is carried out taking into account its form, causes of occurrence and frequency of relapses. In case of rare paroxysms (one in a few months or years), their drug prevention is inappropriate, but the patient is given recommendations regarding lifestyle, employment (if necessary); Smoking and alcohol abuse are excluded. When P. t. associated with heart disease, therapy and prevention of exacerbations of the underlying disease are carried out. With frequent relapses of P. t., there is a need to use sedatives and antiarrhythmic drugs: propranolol 20-40 mg 4 times a day, cordarone - 7 days at 0.6 g per day, then 7 days at 0.4 g, after that for a long time, 0.2 g per day in one dose (patients weighing less than 70 kg need to take a break from taking the drug 1 - 2 times a week); quinidine 0.2-0.4 g 4 times a day (or quinidine-durules 0.25-0.5 g 3 times a day) or aminoquinoline drugs - quingamin 0.25 g or plaquenil a 0. 2 g, the first 10 days 3 times a day, and then 1 time, preferably at night. In some cases, especially in patients receiving diuretics, it is advisable to use potassium preparations (potassium chloride, panangin).
In some patients, including those with the ventricular form of paroxysmal tachycardia, its prevention is achieved by using ajmaline (see) and drugs containing it.
Bibliography:
Sumarokov A.V. and Mikhailov A.A. Cardiac arrhythmias, p. 35, M., 1976; Chazov E.I. and Bogolyubov V.M. Cardiac arrhythmia, p. 143, M., 1972; Chernogorov I. A. Heart rhythm disturbances, M., 1962; Bellet S. Clinical disorders of the heart beat, Philadelphia, 1971.
A. V. Sumarokov, V. A. Bogoslovsky.
Diagnosis and treatment
To confirm the diagnosis:
- 24-hour electrocardiogram (ECG) monitoring;
- They do an ECG during an attack, an ultrasound of the heart.
Usually making a diagnosis is not difficult. The disease is determined based on the suddenness of the onset and end of an attack of tachycardia. Determining the heart rate is of great importance: if it exceeds 150, then sinus tachycardia is excluded.
Taking an anamnesis is very important for the doctor.
Diagnostically significant are:
- occupation of a person during an episode of tachycardia;
- is there a feeling of sudden cardiac arrest;
- whether there is darkening in the eyes or dizziness;
- is there pain in the heart area?
- how quickly the attack ended;
- whether the patient was conscious.
The following diagnostic methods are used.
- Physical examination. The most informative is pressing on the receptors of the vagus nerve. It is necessary to carry out tests very carefully, because they can cause complications.
- Electrocardiogram. Provides the most accurate data regarding the work of the heart and its rhythm. With paroxysmal tachycardia, there is a change in the P waves while the QRS is preserved.
- Holter monitoring. It allows you to register even the shortest episodes of tachycardia that are not felt by the patient.
- Stress electrocardiographic tests.
- Echocardiography.
- Transesophageal stimulation of cardiac activity.
- Electrophysiological examination. To do this, a special electrode is carefully inserted into the heart to study its operation in more detail.
- Magnetic resonance imaging. It allows you to confirm or exclude organic or congenital cardiac pathology.
- Multislice computed tomography.
- Radionuclide scanning.
In some doubtful cases, additional diagnostics may be required.
Paroxysmal tachycardia - symptoms, treatment
5
(100%)
6
votes
The determination of PT and its type is based on what symptoms were observed in the patient during the attack and ECG readings.
Remember that an accurate description of how you feel before, during and after an attack will allow your doctor to make the correct diagnosis and prescribe adequate treatment for you.
To do this, answer the following questions:
Diagnosing the pathology does not cause any difficulties and is confirmed during an ECG study performed during an attack. In this case, certain deviations are visible on the ECG.
In addition to performing a standard ECG study, the following procedures may be additionally prescribed:
- ECG monitoring according to Holter;
- ultrasound examination of the heart;
- electrophysiological study through the esophagus (to confirm supraventricular tachycardia);
- MRI;
- Coronography.
The algorithm for identifying paroxysmal tachycardia includes visiting a cardiologist and conducting standard examinations such as auscultation, hematological tests and urinalysis.
A specific method for confirming the disease is an electrocardiogram. Tachycardia on the ECG is manifested by deformation of the ventricular contraction complexes, a change in their frequency, as well as abnormal location and appearance of the wave, reflecting the depolarization of the atria.
The cardiogram should be deciphered by an experienced doctor specializing in functional diagnostics. To exclude organic damage to the heart, ventricular dilatation, and valve defects, an ultrasound examination is required.
A cardiologist can refer a patient to specialized specialists if he suspects the development of concomitant ailments.
The treatment regimen depends on the etiology of the disease, the severity of its course and the individual characteristics of the patient. In most cases, conservative methods are used.
Surgical intervention is necessary in the presence of heart defects or other organic damage that led to the development of the disease.
Drug treatment of paroxysmal tachycardia is reduced to the use of antiarrhythmic drugs, the effect of which is possible due to their influence on the links of the pathogenetic chain.
Cardiac glycosides are used to maintain normal myocardial function. You can take folk remedies on the recommendation of your doctor.
The use of herbal preparations, the effect of which is similar to medications, can rarely completely replace their use. However, in many cases, the use of decoctions and infusions of herbs has a beneficial effect on the health of patients.
Relief of acute attacks of tachycardia is possible at home only in case of mild manifestations. For this, vagal techniques are used that affect the function of the vagus nerve.
Straining, strong coughing and several other movements can activate reflex mechanisms. The vagus has an inhibitory effect on the heart, which reduces the heart rate and helps control an attack of tachycardia.
Instructions with photos and videos of the necessary techniques are widely distributed on the Internet.
If the disease is severe or complicated by pathologies of other organs, treatment should be carried out in medical institutions. Since paroxysm can lead to ventricular fibrillation and cardiac arrest in old age, people over 50 years of age are not recommended to self-medicate or try to fight the attack on their own.
Diagnostic principles
Diagnosis of paroxysmal tachycardias is based on assessing the severity of symptoms, identifying its connection with the arrhythmia, and recording the arrhythmia itself on the electrocardiogram. At the same time, a standard ECG is not always informative. In order to record an attack of arrhythmia, Holter monitoring is usually used. For relatively rare episodes of arrhythmia, it is advisable to use multi-day monitoring with the inclusion of ECG registration according to indications.
At the next stage, to identify organic heart damage and assess the functional state of the myocardium, the patient is prescribed echocardiography.
In order to clarify the mechanism of supraventricular paroxysmal tachycardia, such patients undergo an electrophysiological study.
Treatment
Ventricular tachycardia is an indication for hospitalization. An examination is prescribed if attacks occur more often than twice a month.
There are ways to reduce the intensity of symptoms on your own. The patient can take the medicine prescribed by the doctor; in case of a supraventricular attack, you can try to mechanically influence the vagus nerve, for this you need:
- close your eyes and press on the inner corners of your eyeballs;
- throw back your head;
- close your mouth and nostrils and try to exhale vigorously;
- tense your abs, hold your breath.
The last method is a variant of the Valsalva maneuver. This method is used to relieve an attack of tachycardia. The technique is for a patient with a paroxysm of tachycardia to try to tense the abs and limbs for 15 seconds, then relax it for 1-2 minutes, then tense the muscles again.
Another way to help cope with an attack of paroxysmal tachycardia is the Chermik-Goering test. It consists of massaging the branch point of the carotid artery alternately on the right and left. Massaging time on one side is 15 seconds, the interval between massaging is 1-2 minutes.
These methods are not used in weakened patients. It is more suitable for young people without significant health problems. If the patient cannot control the attack on his own, then drug treatment for paroxysmal tachycardia is prescribed.
Drug therapy
To prevent or stop an attack, antiarrhythmic drugs are prescribed. Corvalol, Valocordin, Relanium will help cope with mild attacks.
To relieve prolonged severe attacks, tablets, solutions, dragees Anaprilin, Finoptin, Verapamil, Obzidan, Sotalex, Procainamide, Propranolol, Esmolol, Amiodarone are used. Ventricular tachycardia is treated with intravenous, intramuscular administration of Lidocaine, and Rytmilen is prescribed.
Antiarrhythmic drugs are prescribed with cardiac glycosides and beta-blockers. The latter slow down the frequency and force of contractions of the heart muscle, and prevent the effect of catecholamines on the functioning of the heart.
In cases where it is not possible to cope with the paroxysm of tachycardia using medicinal methods, electric pulse and surgical treatment are used.
Surgical intervention
Treatment tactics are determined:
- type of tachycardia (atrial, nodal, ventricular, unspecified);
- etiology;
- frequency and duration of attacks;
- presence/absence of complications, etc.
If ventricular paroxysmal tachycardia is diagnosed, the patient must be hospitalized.
Of course, there are options when the symptoms quickly stop, and the patient’s condition subsequently improves. However, given the possible consequences and complications, it is better to be safe.
In the case when supraventricular AT (atrial or nodal) is diagnosed, the patient is referred to the cardiology department if signs indicating heart failure are diagnosed.
If there are systematic attacks at least twice a month, planned hospitalization and treatment are recommended.
In case of tachycardia, a person should receive immediate medical assistance and call a cardiac emergency team.
Treatment of patients is based on the use of antiarrhythmic drugs. The diagram is signed by a cardiologist who observes the patient on an outpatient basis.
For frequent and severe attacks, the doctor prescribes anti-relapse treatment. In cases where attacks are infrequent and short-lived, it is possible to use vagal maneuvers without anti-relapse therapy.
Long-term treatment aimed at preventing relapses includes the use of antiarrhythmic drugs and cardiac glycosides.
Ventricular paroxysmal tachycardia can develop into ventricular fibrillation, so its treatment may require the use of beta-blockers.
If it is not possible to normalize the heart rhythm with medications, then the doctor may prescribe electrical pulse therapy, intracardiac or transesophageal electrical stimulation of the heart.
In very severe cases, surgery may be necessary.
Indications for it may be:
- ventricular fibrillation;
- attacks of PT that are not eliminated with medication;
- the presence of anomalies and malformations of the heart;
- recurrent attacks of PT at a young age, which have a strong impact on physical and psycho-emotional development.
The operation itself can be performed on both an open and closed heart, which is determined by the type of paroxysmal tachycardia.
Treatment of the disease is aimed, first of all, at preventing the formation of an attack of paroxysms. It is also necessary to treat the underlying disease that caused the appearance of paroxysmal tachycardia. In addition, treatment also involves eliminating the rapid heartbeat that has begun.
Treatment of paroxysmal tachycardia should be carried out inpatiently. The exception is idiopathic attacks with the possibility of rapid relief.
Advice! Treatment of paroxysmal tachycardia is carried out in the cardiology department.
Planned hospitalization is prescribed in cases where paroxysms are recorded at least twice within a month. Treatment in this case is prescribed after a full examination. In some cases, surgical treatment may even be prescribed.
The main method of treating paroxysmal tachycardia is taking medications. When paroxysm begins, treatment is carried out with universal antiarrhythmics. Prolonged attacks of ventricular tachycardia require the use of electrical impulse therapy.
Outpatient treatment is prescribed by a cardiologist according to a specific scheme individual for each patient. Therapy involves taking antiarrhythmics.
If supraventricular paroxysmal tachycardia is diagnosed (if the attack can be stopped on its own), anti-relapse therapy is not prescribed. Treatment in this case is also selected on an individual basis. ECG monitoring is mandatory. Additionally, the following drugs may be prescribed:
- β-blockers, which reduce the likelihood of ventricular atrial fibrillation;
- cardiac glycosides to prevent recurrent attacks and reduce heart rate.
Advice! The greatest effect in the treatment of pathology is obtained by combining β-blockers with antiarrhythmic drugs.
Surgery
Invasive treatment for this pathology is recommended only in exceptional cases, when drug therapy is ineffective. The following techniques may be recommended to the patient:
- radiofrequency ablation;
- implantation of an electric defibrillator.
Do not forget that paroxysmal tachycardia is one of the most serious pathologies that requires adequate treatment. After all, a prolonged attack can cause fibrillation and ventricular fibrillation. The worst prognosis is death.
Paroxysmal ventricular tachycardia
Paroxysmal ventricular tachycardia is a type of heart rhythm disorder, which is manifested by its increase in frequency to 130-220 beats per minute. This type of arrhythmia is episodic. Paroxysms occur suddenly, which threatens the life of a sick person. According to medical statistics, gastrointestinal tract develops mainly in older people who are prone to myocardial dystrophy or sclerosis. Today, the disease occurs in every fortieth resident of our state, occupying not the least place among the causes of mortality.
With ventricular tachycardia, the ventricle of the heart generates ectopic frequent electrical impulses, which lead to disruption of the heart rhythm. Such disorders can provoke ventricular fibrillation with the absence of the main phases of systole and diastole. Heart function is impaired, resulting in heart failure, shock, pulmonary edema and other emergency conditions, which cause mortality in patients.
With ventricular tachycardia, the ventricle of the heart generates ectopic frequent electrical impulses, which lead to disruption of the heart rhythm. Such disorders can provoke ventricular fibrillation with the absence of the main phases of systole and diastole. Heart function is impaired, resulting in heart failure, shock, pulmonary edema and other emergency conditions, which cause mortality in patients.
Treatment of ventricular paroxysmal tachycardia
Reflex methods for paroxysmal VT are ineffective. Such paroxysm must be stopped with medication. Drugs used to interrupt an attack of ventricular PT include lidocaine, procainamide, cordarone, mexiletine and some other drugs.
If medications are ineffective, electrical defibrillation is performed. This method can be used immediately after the onset of an attack, without using medications, if the paroxysm is accompanied by acute left ventricular failure, collapse, or acute coronary failure. Electric current discharges are used to suppress the activity of the tachycardia focus and restore normal rhythm.
If electrical defibrillation is ineffective, cardiac pacing is performed, that is, imposing a slower rhythm on the heart.
With frequent paroxysms of ventricular AT, installation of a cardioverter-defibrillator is indicated. This is a miniature device that is implanted into the patient's chest. When an attack of tachycardia develops, it performs electrical defibrillation and restores sinus rhythm. To prevent repeated paroxysms of VT, antiarrhythmic drugs are prescribed: procainamide, cordarone, rhythmilene and others.
If drug treatment fails, surgery may be performed to mechanically remove the area of increased electrical activity.
The examination includes a 12-lead electrocardiogram, 24-hour electrocardiogram monitoring, and a transesophageal electrophysiological study. Additionally, an ultrasound examination of the heart, clinical blood and urine tests, electrolytes are prescribed, and, if necessary, the thyroid gland is examined.
Causes of paroxysmal tachycardia
Supraventricular paroxysmal tachycardia occurs as a result of increased activation of the sympathetic nervous system. Ventricular is a consequence of necrotic, inflammatory, sclerotic or dystrophic damage to the heart muscle.
In the ventricular form, the focus of ectopic excitation is located in the His bundle, its legs and Purkinje fibers, that is, in the ventricular sections of the conductive nervous system. Most often, the pathology is diagnosed in elderly men who have suffered a myocardial infarction, coronary heart disease, or suffer from hypertension, myocarditis, or heart defects.
The main causes of the development of paroxysmal tachycardia also include:
1. The presence of additional innate impulse pathways in the myocardium. That is:
- Kent's bundle between the atria and ventricles, bypassing the atrioventricular node;
- Macheim fibers between the atrioventricular node and the ventricles.
2. The presence in the myocardium of additional impulse pathways resulting from myocardial damage (infarction, myocarditis, cardiomyopathy).
3. Additional pathways cause pathological movement of excitation throughout the myocardium.
Cardiology knows cases when longitudinal dissociation appears in the atrioventricular node, causing uncoordinated functioning of the fibers of the atrioventricular connection. Then some of the fibers function normally, while the other, on the contrary, conducts excitation in the retrograde (opposite) direction and acts as the basis for the circular circulation of impulses from the atria to the ventricles and along the opposite fibers back to the atria.
In young children, essential (idiopathic) paroxysmal tachycardia of unknown etiology is sometimes diagnosed.
1. The presence of additional innate impulse pathways in the myocardium. That is:
What is paroxysmal tachycardia
A type of arrhythmia caused by the activation of frequent electrical impulses in the ventricles or interventricular septa is called Bouveret's disease or ventricular paroxysmal tachycardia (VPT).
In various forms, pathology is diagnosed in 20-30% of patients of all ages. In older people, it is caused by organic changes in the myocardium; in young people, tachycardia is functional in nature. GPT occurs more often in men.
Due to the change in wave duration, the repeated impulse appears too early, a process of repolarization occurs - the work of the ventricles and atrium becomes uncoordinated (dissociated). The paroxysm begins and ends suddenly.
Treatment and rehabilitation
Treatment of gastrointestinal tract is carried out on an individual basis, depending on the patient’s condition and the cause of the pathology.
Electrical pulse treatment (restoration of heart rhythm using electric current pulses) is mainly used as therapeutic measures
Conservative (drug) therapy for gastrointestinal tract includes the use of the following drugs:
- Antiarrhythmic drugs that restore and maintain heart rhythm;
- Beta-adrenergic blockers - reduce heart rate and lower blood pressure;
- Calcium channel blockers - restore normal heart rhythm, dilate blood vessels, reduce blood pressure;
- Omega 3 fatty acids lower cholesterol levels in the blood, prevent the formation of blood clots and have an anti-inflammatory effect.
Surgical treatment is performed if the following indications exist:
- History of ventricular fibrillation;
- Serious changes in hemodynamics in patients with post-infarction GVT;
- Persistent extrasystolic allorhythmia;
- Frequent, recurrent attacks of tachycardia in patients who have had myocardial infarction;
- Disorders, pathologies and diseases resistant to drug therapy, as well as the inability to use other treatment methods.
Surgical treatment methods include implantation of electrical defibrillators and pacemakers , as well as destruction of the source of arrhythmia using a radiofrequency pulse.
During the rehabilitation period, patients who have suffered an attack of gastrointestinal tract disease are advised to adhere to a diet, eliminate physical and psycho-emotional stress, regularly spend time in the fresh air and follow all doctor’s instructions.
This video highlights new research and treatment options for this disease:
- Hemodynamic disorders (congestive circulatory failure, etc.);
- Ventricular fibrillation and fibrillation;
- Development of heart failure.
Causes
PT can be caused by reflex irritation of the autonomic nerves during swallowing, constipation, sharp turning, irritation of sensitive trigger points, and osteochondrosis of the thoracic region in the T4-5 segment.
The main causes of paroxysmal tachycardia are:
- heart disease; ventricular hypertrophy;
- ischemic disease;
- heart disease;
- cardiomyopathy;
- myocarditis;
- surgical intervention;
- pulmonary heart;
- diabetes;
- lack of potassium;
- medicinal lesions - taking cardiac glycosides, theophylline, sympathomimetics, antiarrhythmics;
It is not always possible to establish the cause that triggered the attack of paroxysmal tachycardia, and then they speak of idiopathic (essential) tachycardia of unknown origin. This type of rhythm disturbance often occurs in adolescence.
The course of PNT may be complicated by the appearance of additional atypical foci of excitation or conduction disturbances between the centers of cardiac automaticity.
Paroxysmal tachycardias that occur when the centers of automatism lying above the site of division of the His bundle are excited are called supraventricular, which can be provoked by excitation:
- sinus node;
- AV node;
- foci at the mouths of the vena cava and pulmonary veins;
- circulation of the impulse between the atrium and ventricle.
- pale skin;
- fear of death, panic;
- thread-like weak pulse;
- fainting;
- drop in blood pressure;
- collapse.
First aid
If you or someone around you experiences an attack of tachycardia (nodal or another type), you should do the following:
- Calm down, relax, take a lying position (especially if you feel weak and dizzy).
- Provide fresh air, which may involve removing suffocating clothing (unbuttoning it) or opening a window.
- If you have the knowledge and ability to perform vagal tests, do them.
- If the condition only worsens over time, then you should call an ambulance or ask someone nearby about it.
- You should not take untested medications or those not prescribed by your doctor. They may make your condition worse.
Types of disease
The disease is classified according to the location of the paroxysms that occur.
Tachycardia occurs:
- Atrial;
- Ventricular;
- Atrioventricular;
- Sinus;
- Nodal;
Treatment of each form of the disease includes a special approach.
Supraventricular (paroxysmal supraventricular) tachycardia can be atrial and atrioventricular (atrioventricular).
According to the nature and duration of the flow, they are distinguished:
- Spicy;
- Chronic;
- Constantly relapsing form.
The development mechanism includes:
- Focal;
- Multifocal;
- Reciprocal form of the disease.
Depending on the course and location of the lesions, comprehensive measures are prescribed to eliminate the root cause, symptoms and consequences of the disease.
Treatment of atrial form
It involves intravenous administration of beta blockers or calcium channel blockers to reduce the ventricular rate. If there is no positive dynamics, antiarrhythmic drugs are administered.
According to statistics, rhythm blockers help only 60% of patients. If the reaction is negative and there is no positive dynamics from the drugs, electrical stimulation is performed.
The disease is prone to regular relapses, so an effective method is the implantation of pacemakers that control the heart rate.
Sinus therapy
It is amenable to comprehensive drug treatment. For this purpose, combinations of beta blockers, calcium channel blockers and cardiac glycosides are used.
Prolonged attacks are blocked with vagal tests, and if there is no effect, electrical stimulation is performed. Radical methods of treating the sinus form include catheter modification of the sinus node.
Ventricular form of the disease
Medicines can only relieve a short-term attack. Electrical pulse therapy is more effective for paroxysmal ventricular tachycardia.
In severe cases, a surgical solution to the problem is used.
Complications
With frequent attacks, deterioration of myocardial contractile function and heart failure may occur. In such conditions, coronary blood flow decreases, oxygen starvation of the myocardium develops, which threatens necrosis and infarction.
A dangerous complication of atrial tachycardia can be ventricular fibrillation - a chaotic contraction of muscle fibers that can cause blockage of the atria due to the proximity in time of contraction of the atrium to the ventricle, the coincidence of the onset of atrial contraction with ventricular systole.
This causes blockage of the atria, leading to the formation of a blood clot. At the end of the attack, when the main center of automaticity restores its influence on the myocardium, these blood clots can cause blockage of the pulmonary artery.
A dangerous side effect of ventricular tachycardia is ventricular fibrillation. It is a symptom of a heart attack, accompanied by characteristic ECG readings during an attack:
- there is a negative position for the T peak;
- the QT segment increases;
- The ST segment shifts.
Symptoms and diagnosis of the disease in adults, children and infants
to contents
If we consider the situation in general, then attacks of paroxysmal tachycardia can occur at any age (even in young children). At the same time, a child aged 5 years and older is already able to determine the beginning and end of an attack by his feelings. This can be done when a short pause appears. First, a person feels unusual contractions of the heart, then devastation and normalization of the heart rhythm. Attacks of paroxysmal tachycardia are often accompanied by a strong feeling of fear (especially in children). Often there are unpleasant sensations in the stomach, stabbing pain in the heart muscle, nausea, and fatigue. At the same time, during an attack of tachycardia paroxysm, consciousness remains clear.
Long-term rhythm disturbance, regardless of which disease is diagnosed (paroxysmal or non-paroxysmal tachycardia), leads to a general circulatory disorder, and subsequently to even more serious consequences - a disorder of consciousness due to an acute lack of oxygen in the brain. With paroxysmal tachycardia, the total number of ROE and leukocytes may remain unchanged and be maintained at a normal level. The x-ray taken does not show any special deviations - the shape of the heart and its size remain unchanged. If the attack was prolonged, then the heart muscle may be slightly enlarged. The most difficult thing to diagnose is tachycardia paroxysm in very young children.
Diagnosis is further complicated by the fact that the baby's pulse rate (compared to an older child) is much higher. In this case, minor crying or worry can already cause serious tachycardia. Paroxysm of tachycardia in a very young child can be diagnosed by measuring the pulse at normal body temperature, when the person has no reason to worry (for example, immediately after feeding or at the moment of falling asleep). The problem can be accurately diagnosed only after examination, ECG, listening, and so on. Subsequently, treatment and medications are prescribed (if necessary). At the same time, parents must promptly recognize the onset of an attack. As a rule, it is expressed in the appearance of pallor of the body, decreased appetite, the appearance of gag reflexes, increased heart rate, and weakness in breastfeeding. During this period, a significant decrease in blood pressure and low amplitude are possible. The child's vision becomes clouded, the neck veins fill with blood, and blood pressure rises. However, the temperature may remain at normal levels.
Often, with paroxysmal tachycardia, it is not always possible to determine the problem using an ECG. The reason is the unpredictability of the phenomenon - it can appear and disappear at any moment. The worst thing is that it is not always possible to find out the causes and prescribe the correct treatment. In this case, there is a high risk that the tachycardia will return. Paroxysm of tachycardia, as we have already mentioned, is not fatal. But its consequences in children can be no less dangerous than in adults. Shorter diastoles lead to worse filling of the ventricles of the heart. As a result, systolic volume decreases sharply. The result is poor filling of the coronary vessels and a short-term lack of oxygen in the myocardium. Further processes lead to deterioration of blood circulation in the tissues.
But that's not all. Paroxysm of tachycardia and shortening of the diastole of the right ventricle of the heart muscle prevents the required volume of blood from being sent to all organs. As a result, there is a high risk of venous stagnation, which can lead to the so-called arterial plug.
Types of disease
Paroxysmal tachycardia is a general diagnosis, but with an in-depth medical examination it allows us to identify a more precise disease. This type of tachycardia is divided into two groups:
- supraventricular (atrial);
- ventricular
The first group of diseases is characterized by the following symptoms:
- the focus of excitation is located in the atrium;
- the focus of excitation is the AV node.
Paroxysmal atrial tachycardia is much easier to tolerate when compared with the second form of the painful condition.
Ventricular tachycardia is much less common in medical practice. According to statistics, it accounts for only 20% of all cases. With this form of tachycardia, as the name implies, the source of the abnormal heart rhythm is in the ventricle. Only an experienced doctor can distinguish between the types of tachycardia.
Such abnormalities are very rare in individuals who have not previously suffered from various heart lesions. Almost always, ventricular tachycardia is recorded in patients with ischemic disease and other damage to the heart muscle.
Paroxysmal sinus tachycardia is caused by impulses from the sinus node. This place in the human body is responsible for impulses for normal contraction of the heart muscle. In medicine, the normal heart rate is considered to be from 60 to 90 beats. Accordingly, sinus tachycardia is a condition when the pulse exceeds 100 beats per minute, but the impulses emanating from the sinus node are normal.
Sinus tachycardia can occur in humans as an adequate response to physical activity or hormonal changes.
Features of the nature of the course of the disease
An attack of paroxysmal tachycardia can occur suddenly at any time of the day. Before this, you can observe paleness of the skin, increased breathing and pulsation in the superficial veins. If you measure your blood pressure at this moment, you can take the necessary medications and prevent an attack from occurring.
The disease can be acute, chronic or often recurrent. Sometimes it takes a doctor a day to make an accurate diagnosis, because attacks can be replaced by a calm heartbeat.
Signs of paroxysmal tachycardia begin with a strong shock in the chest, after which the heart begins to pound vigorously, as if after a fright. If this condition lasts for a long time, the patient may lose consciousness.
If such an attack occurs, it is necessary to check the heart. Usually such conditions do not arise on their own; there is probably a cardiac pathology.
Pathology is diagnosed based on electrocardiogram readings
How is the disease treated?
Treatment of paroxysmal tachycardia does not have one proven method that is suitable for all patients. A full medical examination is required so that the attending physician chooses the necessary tactics to combat the painful manifestations of tachycardia.
It is important to understand that paroxysmal tachycardia is not an independent disease, but is only a pronounced manifestation of one of the diseases. Often, with tachycardia, nervous system disorders are treated and various forms of arrhythmia are combated.
The prescribed treatment will depend on a combination of factors:
- patient's age;
- forms of arrhythmia;
- frequency of attacks and their severity;
- presence of any heart disease.
In most cases, doctors are able to stop the attack at home. If the heart rate remains elevated for a long time, the patient is taken to the hospital.
To maintain the correct rhythm and reduce the risk of recurrent attacks, patients are prescribed a course of antiarrhythmic drugs. Their main purpose is to reduce the effect of stress on the body. The most famous remedies:
- Concor;
- Anaprilin;
- Atenolol;
- Ritmilen;
- Ethazicin.
First aid for an attack of tachycardia
It is important to understand that any attack of tachycardia, characterized by a high pulse, requires an immediate call to the doctor. Before the ambulance arrives, you can try to relieve an attack of paroxysmal tachycardia by following these steps:
- put the patient to bed. If it is impossible for him to take a lying position, then he must be seated in a chair;
- ensure the flow of oxygen (ventilate the room if it is not possible to go outside);
- take nitroglycerin to reduce the risk of heart attack;
- try to influence the vagus nerve.
The vagus nerve can be affected in several ways. Most often they try to force the patient to strain while taking a deep breath. The tension of the expiratory muscles in this case contributes to a strong increase in intrathoracic pressure. If done correctly, blood flow to both atria will decrease.
The second method is to massage the carotid arteries on both sides. The main thing is not to use force, but to perform progressive light movements, trying to calm the patient. Usually, without medical education, it is very difficult to find the right place. The attending physician must teach the patient to use this method independently during attacks. If the patient does not know where to massage, then you should try to massage the artery immediately under the jaw.
Another effective first aid method is gentle pressure on the eyeballs. Here it is very important to correctly calculate the force in order to avoid negative consequences.
Clinical manifestations
Symptoms of paroxysmal tachycardia of any form are expressed in rapid heartbeat, sometimes reaching up to 300 beats per minute. In addition, patients complain of the following symptoms:
- Discomfort in the chest in the area of the heart.
- It makes you feel hot and then chills.
- The body sweats a lot, even at rest.
- Feeling of weakness, the patient is unable to do any work because he gets tired very quickly.
- He becomes nervous, irritable, and loses sleep.
With the ventricular form of the disease, these symptoms are not observed. There may be heart pain, increased blood pressure and swelling of the legs. Due to circulatory failure, the respiratory system also suffers; patients complain of lack of air and shortness of breath.
Etiology of the disease
Pathology develops for various reasons. Paroxysmal supraventricular tachycardia can occur as a result of stressful situations, since these parts of the heart are connected to the nervous system.
The ventricular form of the disease develops as a result of inflammatory processes of an infectious nature that affect the heart muscle, as well as necrotic changes in cardiac tissue or sclerotic deposits.
The occurrence of paroxysmal ventricular tachycardia may be preceded by hypertension, heart attack, and heart defects. This form is most common in men over 50.
Often the causes of pathology are congenital defects; they are detected at an early age and require surgical intervention. Paroxysmal tachycardia of the idiopathic form occurs in children and adolescents, the causes of which are still unclear.
Heavy physical activity can trigger an attack
There are certain factors that can trigger an attack. These include:
- Sudden movements that put stress on the heart.
- Heavy physical activity requiring the use of force.
- Overeating and poor nutrition.
- Sudden temperature changes, hypothermia or overheating.
- Stressful situations and negative emotional experiences.
- Taking certain medications.
- Surgical operations on the heart muscle.
- Chemical poisoning.
- Abuse of alcohol and coffee, smoking.
- Endocrine changes in the body.
- Hereditary predisposition.
- Inattention to your heart.
If you experience discomfort in the chest area on the left side, you should contact a cardiologist and undergo an electrocardiogram. This will help prevent the severe consequences of paroxysmal tachycardia.