Oral contraceptives are birth control pills taken orally to prevent pregnancy.
They contain synthetic analogues of two hormones produced in the body, and are called COCs (combined oral contraceptives). Estrogen and progestin (gestagen) regulate a woman’s menstrual cycle, so taking them in the required dosages on a specific schedule is an effective method of preventing pregnancy. Research shows that less than 1% of women taking oral contraceptives become pregnant within the first year of using them. That is, the efficiency of the PDA is more than 99%. Recommended reading:
Birth control pills come in a wide range of estrogen and progestin combinations. The drugs used today contain lower doses of estrogen than were available in the past, greatly reducing the likelihood of serious side effects.
The essence of birth control pills and the mechanism of action of PDAs
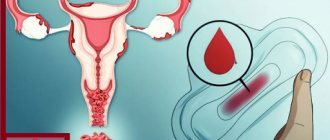
For conception to occur, the egg must mature in the ovary and move into the fallopian tube. When the sperm reaches the fallopian tubes, fertilization of the egg occurs. The fertilized egg then passes into the uterus, where the embryo develops. Oral contraceptives do not allow the egg to mature completely: the progestins contained in the tablets block the release of statins (releasing factors), the secretion of gonadoliberin is inhibited, which inhibits. An unripe egg cannot be fertilized. In addition, birth control pills thicken the mucus in the cervical canal, preventing sperm from passing through. Oral contraceptives also change the structure of the endometrium, which prevents the fertilized egg from attaching to the uterine wall and developing. The estrogenic component of the PDA stabilizes the menstrual cycle.
How do birth control pills work?
The composition of birth control pills consists of sex hormones created artificially (analogs of estrogen, progesterone).
They weaken the activity and maturation of eggs. There are contraceptives that contain only estrogen. Combination pills include both hormones. The medication must be taken daily at the same time.
Classification of combined oral contraceptives
According to dosage regimen, oral contraceptives are divided into:
- monophasic,
- two-phase,
- three-phase.
Monophasic ones (non-ovlon, rigevidon, ovidone) include estrogen and gestagen in certain quantities. Dosage regimen: daily for 21 days.
Two- and three-phase (anteovin, triziston, tri-regol, triquilar) are taken according to the same scheme, but they are produced in sets/containers, which include tablets with different concentrations of estrogen and gestagen, corresponding to the physiological cycle. This packaging helps a woman “track” her daily intake of birth control pills. The tablets have different colors, indicating the amount of hormones contained.
Some drugs are produced with additional dummy tablets (without active substance). They are designed to develop a “conditioned reflex” - the habit of taking a contraceptive every day, and not just on certain days of the menstrual cycle. Since the amount of hormones in two- and three-phase preparations is smaller, they have a weaker effect on metabolic processes without reducing the contraceptive effect.
Based on the estrogen component, COCs are divided into: ethinyl estradiol-containing and NOC (natural oral contraceptives) based on estradiol valerate . Ethinyl estradiol (EE)-containing COCs are divided into:
- High-dose doses - 50 mcg of EE (anteovin, non-ovlon) - are not currently used due to the high risk of side effects.
- Low-dose - 30–35 mcg EE (Yarina, Marvelon, Zhanin, Diane-35) with high contraceptive reliability.
- Microdosed – 15–20 mcg EE (Jess, Mercilon, Logest).
A drug based on estradiol valerate (EV) – claira. EV is chemically identical to the natural hormone of the female body, so it has a milder effect than EE, hence the name - NOC.
There is no clear division according to the gestagenic component. First, testosterone derivatives with residual androgenic activity were used as progestins. Next came drugs containing levonorgestrel, desogestrel, and gestodene. Then progestins with antiandrogenic action were created: dienogest, drospirenone, cyproterone acetate.
Contraception for women
In ancient times, contraceptives were made using traditional methods. Nowadays there are many different effective drugs.
Hormonal contraceptive pills are widely used. They create an obstacle to the process of the egg leaving the ovary, thereby preventing pregnancy. Hormonal products are also available in capsules. Barrier-type methods are quite popular: diaphragms, caps, reusable rings.
Chemical contraceptives include various ointments, suppositories, tablets containing special active substances that kill sperm (they are not highly effective).
Until now, the most recognized method to prevent pregnancy is a condom. One of the new generation methods for preventing pregnancy can be considered sterilization (artificial closure of the fallopian tubes).
Birth control pills
Contraceptive drugs, in addition to the function of preventing pregnancy, act as drugs that treat women's diseases. They have virtually no contraindications based on age; they are often prescribed even to girls who are not yet sexually active as a therapeutic agent. There is practically no limit on their use.
What are the advantages of birth control pills:
- prevent pregnancy in 99% of 100%;
- balance hormones in the body;
- allow you to avoid unwanted painful manifestations during menstruation;
- treat mastopathy, reduce the risk of malignant tumors;
- after completing the course, the possibility of getting pregnant increases;
- skin improves, hair and nails become stronger.
The advantages of birth control pills are quite high, but serious attention should also be paid to the disadvantages:
- Guaranteed protection against pregnancy is often not justified (this happens if you violate the order of taking the medication);
- It is not recommended to take the drug simultaneously with a course of antibiotics (the effect of the drug is reduced);
- in the first days of taking the tablets, a small amount of blood discharge is noticed;
- after completing the course, some women experience a disturbance in their menstrual cycle;
- the need for food increases (while taking contraceptive medications, it is advisable to adhere to a special diet and be more active).
Vaginal contraceptive pills
Vaginal contraceptive pills are included in the category of substances that weaken sperm activity (spermicides), which are a type of barrier chemical contraceptives.
A fairly simple, affordable method of protection against pregnancy. They are inserted into the vagina, forming a thin film, creating a thick cervical discharge that serves as a barrier to active sperm. Mainly used by women who are not recommended for other productive means—hormonal medications, IUDs.
Advantages of vaginal contraceptives:
- there are practically no side effects;
- reduces the likelihood of sexually transmitted diseases;
- no need for daily intake;
- allowed to be used for women's diseases;
- low price.
There are not many disadvantages to vaginal birth control pills:
- low efficiency (up to 70%);
- It is not recommended to use the drug every day;
- causes dysbacteriosis;
- irritates the vaginal mucosa;
- cannot be used for certain gynecological diseases;
- danger of an allergic reaction.
Contraceptive patch
Modern medical technologies are constantly moving forward, creating new, more effective medicines. The contraceptive patch is part of a group of new generation drugs. At first glance, it is practically no different from an ordinary adhesive plaster. The size of the contraceptive is approximately 20 cm2.
Stick on the buttocks, shoulders, abdomen on the first day of the menstrual cycle. The drug is changed to a new one at the beginning of each subsequent week. There is no need to apply a patch in the fourth week, since it marks the end of the menstrual period.
According to doctors, the contraceptive patch is 95-100% effective, which has recently become a reason for great popularity.
The big advantage of contraception is the absence of restrictions in a woman’s sexual life. The patch does not require time restrictions. The drug is also convenient because it can be easily removed if necessary.
One of the disadvantages is that it belongs to hormonal drugs. Another drawback is the inconvenience when bathing (the patch comes off due to moisture) . We have to somehow protect it from contact with water. The contraceptive is not recommended for women with sensitive skin.
Contraceptive spiral
The two main categories of contraceptive IUDs are metal-containing and hormone-containing. The drug reduces sperm activity by turning cervical mucus into an impassable mass. The most famous types of contraceptives are “Multiload Cu-250 and Cu-375” and “Copper T”, “Nova T” .
Copper ions do not allow sperm to actively act and achieve their goal. The disadvantage of the copper coil is oxidation when combined with the contents of the uterus. For this reason, the copper spiral can be used for no more than 3 years.
A copper-silver spiral is considered more effective. The principle of action is the same as that of the copper preparation, but the period of use is longer—up to 7 years, since oxidation practically does not occur due to the presence of silver.
The most productive of metal-containing contraceptives is the gold coil. It is the safest, most effective, and most hygienic. The gold spiral comes in three sizes: standard, short, mini.
Mirena is a hormonal IUD, a combined hormonal and intrauterine contraceptive. Doctors recommend using a hormone-containing IUD for women suffering from uterine fibroids. In addition to contraceptive properties, the drug has healing properties.
The effectiveness of any type of spirals is 80-90%.
Contraceptive ring
The contraceptive drug NuvaRing is a smooth ring inserted into the vagina for a three-week period. Because of its softness, it adapts to the body type. The flexibility of the ring provides comfort, allowing a woman to lead an active life and freely engage in sports.
In the vagina, the ring acquires body temperature, the membrane secretes hormones, which are enough to prevent the maturation of the egg.
Advantages of the contraceptive:
- reliability;
- ease of use;
- no effect on body weight;
- no pain during menstruation.
Flaws:
- unfamiliarity with use (for some women);
- no guarantee of protection against sexually transmitted diseases.
The ring is inserted during the menstrual cycle (days 1-5) independently. Using two clenched fingers, the flexible medication is inserted deeply into the vagina. The ring takes the desired position. After 3 weeks it must be removed. After 7 days, the procedure can be repeated.
Contraceptive implant
A capsule 4 cm long, 2.5 mm thick is inserted subcutaneously through a hollow needle into previously anesthetized parts of the body on 7 days of menstruation. Hormones are released from the walls of the implant. Once in the bloodstream, they have a contraceptive effect, delaying the maturation of the egg. The contraceptive is introduced for 4-5 years. Guaranteed efficiency - 95-100%.
Birth control pills, which are currently available in modern medicine, have not received as much attention as the new generation method—the introduction of a contraceptive hormonal implant.
A single administration of the drug is a great advantage. The contraceptive does not require constant monitoring of hormone levels, does not affect metabolism, does not disrupt the function of the liver or intestines, since hormones are distributed directly in the blood. With a vaginal implant, it is not prohibited to drink alcohol or smoke.
Disadvantages of the contraceptive are possible disruption of menstruation. During the first period of administration, headaches, nausea, weakness, and a strong need for food are not excluded.
Before the drug administration procedure, it is recommended to undergo a general medical examination.
Contraceptive cream
Quite a productive product. Recently it has become very popular. Ease of use, high guarantee creates comfort in using the drug. Using a special syringe, the contraceptive is inserted into the vagina and instantly distributed over its walls.
The duration of action is limited to 60 minutes. The cream contains antibacterial substances that protect against a number of infectious diseases. The drug is absolutely harmless for nursing mothers - it does not penetrate into the blood, and, therefore, does not harm the baby.
The disadvantage of the contraceptive is the fear of direct contact with water. The cream instantly loses its properties. It is not recommended to use the product more than once a week.
Contraceptive cream Benatex and Pharmatex are in great demand.
Contraceptive injections for women
For certain reasons, some women cannot use birth control pills. It is described above what other substitutes there are. Another one of them is injections.
The injectable drug can be used once every three months. The contraceptive Depo-Provera, made in the USA, is in great demand. The action of the contraceptive injection is identical to the action of all other contraceptives.
The injection guarantees 99% protection, is administered to women at any age, and does not cause infertility. After the injection, it is not prohibited to smoke or drink alcohol (possible in very small quantities).
The downside of injections is the ability to get pregnant only 12-14 months after using a contraceptive.
Other disadvantages of contraceptive injections include: the inability to protect against infections, menstrual irregularities, and the development of certain types of cancer.
Women using contraceptive injections should be examined by a gynecologist at least 2 times a year.
Advantages of a PDA
In addition to the 99% effectiveness of drugs containing progestin and estrogen, they have the following advantages:
- reduction of symptoms of dysmenorrhea, menorrhagia;
- reliability, reversibility of action;
- reducing the incidence of unpleasant nagging premenstrual pain;
- “safety net” against the occurrence of benign neoplasms of the mammary glands;
- reducing the risk of inflammatory processes in the pelvis (as opposed to the use of intrauterine devices);
- reducing the risk of endometrial cancer (by 50%), ovarian cancer (by 80%).
Method of use of COCs
Important:
The dosage regimen depends on the type of oral contraceptives. For a 21-day schedule: take one tablet daily for 21 days, then skip 7 days and repeat the cycle. For a 28-day schedule: take one tablet for 28 days, then repeat the cycle. Carefully studying the instructions included with the drug will help you avoid mistakes.
Missing a dose by more than 24 hours increases not only the risk of conception, but also the likelihood of side effects. It is advisable to take PDA at the same time “automatically”, then a habit will appear: we don’t forget to brush our teeth. If a dose is missed, follow the instructions in the instructions or consult the doctor who prescribed the medicine for recommendations. It is better to take birth control pills with food or before bed. This will help prevent nausea that sometimes occurs during the first few weeks.
Leading manufacturing companies
The most popular and effective products from the following manufacturers:
- Gideon Richter. This is a Hungarian company that produces not only tablets, but also candles. They are effective in protecting against unwanted conception and against inflammatory processes.
- Innotec International. One of the oldest companies producing hormonal and non-hormonal contraceptives. They produce safe drugs that help fight inflammation of the reproductive system.
- Merc. Manufacturer with head office in Germany. It produces not only tablets, but also a vaginal ring. The quality of contraceptives always remains at the highest level and has withstood competition for many years.
- Bayer Pharma Ag. One of the main competitors. The main office is also located in Germany.
Side effects of hormonal contraception
Serious side effects are more likely to occur in women over 35 who smoke and in patients with specific health problems (hypertension, diabetes, a history of breast or uterine cancer). All risks and benefits of this type of contraception should be discussed with a gynecologist, taking into account your health condition.
Side effects are rare in healthy women, but it is still better to be aware of them. Oral contraceptives may cause:
- liver tumors, including malignant ones;
- increased blood pressure;
- stroke;
- nausea/vomiting;
- cramping abdominal pain;
- chest pain;
- swelling of the legs (ankles);
- fatigue;
- acne;
- menstrual changes, including mid-cycle bleeding;
- headache;
- vaginal infections;
- itching/irritation of the external genitalia;
- heaviness in the chest;
- change in libido;
- venous thromboembolism;
- depression;
- skin reactions;
- fluid retention, weight gain;
- increased blood sugar levels.
Birth control pills cause photosensitivity - sensitivity to sunlight, so you should avoid prolonged exposure to the sun and avoid tanning beds. Sometimes age spots appear, disappearing a few months after the COC is discontinued. Oral contraceptives can cause bleeding gums and irritation of the cornea when wearing contact lenses.
The side effects of oral contraceptives are described in more detail in the video review:
Tablet selection criteria
When choosing birth control pills, you should pay attention to the following criteria:
- woman's age;
- absence or presence of abortions and pregnancies;
- severity of PMS;
- intensity of discharge during menstruation;
- diseases of the reproductive system (this could be fibroids or cysts);
- sexual activity;
- frequency, duration and pain of inflammatory processes.
In addition, in order to eliminate various risks of developing pathologies, it is necessary to consult a doctor and conduct the following examinations:
- submit smears for oncocytology from the cervix;
- do an ultrasound of the pelvic organs and mammary glands;
- donate blood for general and biochemical analysis.
Remember that only a doctor should prescribe birth control pills. Choosing contraceptives on your own can lead to health problems. Most often, the doctor prescribes a number of similar drugs with the same effect. And the woman herself chooses the right one for herself.
Mini-pill – progestogen contraception
Mini-pills are oral contraceptives that contain only the hormone progesterone (without estrogen). Mini-pills (Exluton, Microlut, Ovrette) are prescribed to women who cannot use COCs: over 35 years old, suffering from hypertension, with a tendency to thrombosis, and overweight.
Mini-pills can be used:
- for heart disease;
- liver diseases;
- breast cancer;
- vaginal bleeding of unknown etiology;
- ovarian cyst.
The tablets are safe to take while breastfeeding: a small amount of gestagen may pass into breast milk, but this is not harmful to the baby.
The minipills are generally well tolerated and side effects are rare. The first few months may include:
- acne;
- soreness, swelling of the breast;
- increased/decreased sexual desire;
- mood changes;
- headache/migraine;
- nausea, vomiting;
- small ovarian cysts (disappear without treatment);
- stomach upset;
- weight gain.
Oral contraceptives: pros and cons
COCs have been used for 55 years. The “horror stories” associated with the side effects of the “pioneers” of hormonal contraception are gradually being forgotten: “a mustache will grow,” “you will get fat,” and others. Birth control pills not only help women control their reproductive function, they are prescribed for hormonal imbalances, hirsutism, acne, dysmenorrhea, and PMS. But we must not forget that these are still hormonal drugs that have a number of contraindications, so they must be prescribed by a doctor.
You will receive more useful information about the advantages and disadvantages of oral contraceptives by watching the video.
“ Graviora
quae dam sunt remedia periculis ” (“Some medicines are worse than the disease”, Latin)
Hormonal contraception is currently one of the most common methods of family planning throughout the world. Millions of women have been using these “peace pills” very successfully for a long time - convenient, reliable, practically safe when used correctly. However, against the background of long-term (months and years) hormonal contraception, quite often there is a need to use (for a variety of indications) medications of many pharmacological groups. This is where certain difficulties often arise: issues of compatibility, pharmacological interactions, complications, side effects, etc. are, in many ways, terra incognita. Therefore, we have made a modest attempt to “dispel the fog.”
As is known, hormonal contraceptive drugs most often have a combined composition (estrogens, mainly represented by ethinyl estradiol (EES), and gestagens of various generations and chemical modifications) and are called COCs. A variety of medications prescribed concomitantly with COCs can alter their contraceptive activity. COCs, in turn, quite often significantly affect the pharmacodynamics, bioavailability and other important aspects of the action of many drugs. In the processes of interaction of COCs, their estrogenic component plays a special role. Previously, it was believed that the progestogen component in drug interactions was not significant. However, according to Shenfield (1993), relatively recently developed gestagens of the third generation, in particular desogestrel, also undergo sulfate conjugation in the gastrointestinal tract, resulting in the potential for their interaction with many drugs.
The metabolism of exogenous ethinyl estradiol is as follows. 65% of the dose of EES taken orally undergoes conjugation in the intestinal wall, 29% is hydroxylated in the liver with the participation of the microsomal enzymatic system; the remaining 6% forms glucuronic and sulfate conjugates in the liver. Conjugated EES derivatives are excreted in the bile and enter the intestine, where they are exposed to bacteria to produce active hormone, which is then reabsorbed (so-called hepatoenteric recirculation). COCs have an effect on the microsomal enzyme system of the liver, as a result of which the hydroxylation activity of these enzymes decreases, metabolism slows down and the concentration increases
in the plasma of some concomitantly taken drugs.
Therefore, the therapeutic dose of these drugs must be reduced
to avoid complications of drug therapy.
With an increase in the degree of glucuronide conjugation, an inducing effect is observed, and therefore an increase in
the therapeutic dose is indicated to prevent a decrease in the effectiveness of treatment (see Table 1). One of the mechanisms of pharmacological interaction is a possible induced increase in globulin that binds sex hormones in plasma, and a decrease in connection with this amount of biologically active free steroids.
Table 1. Interaction of COCs with other drugs
| rises (the therapeutic dose | The concentration of the drug in plasma decreases (the therapeutic dose must |
| Chlordiazepoxide (Elenium, Librium, Clozepid) | Acetylsalicylic acid |
| Diazepam (Relanium, Seduxen, Sibazon, Valium, Apaurin) | Acetamifene (paracetamol) and its analogues |
| Nitrazepam (eunoctine, radedorm, reladorm) | Narcotic analgesics (promedol, morphine) |
| Beta blockers | Lorazepam, oxazepam, temazepam (signopam) |
| Corticosteroids | Difenin |
| MAO inhibitors and tricyclic antidepressants (imipramine, melipramine, amitriptyline) | Adrenergic agonists |
| Purine derivatives (caffeine, theophylline, aminophylline) | Clofibrate |
| Ethyl alcohol | Thyroid hormones |
| Ascorbic acid (vitamin C) | Indirect anticoagulants |
| Retinol (vitamin A) | Sugar-lowering (hypoglycemic) drugs: (insulin, butamide, chlorpropamide, etc.) |
| Neuroleptics - phenothiazine derivatives (aminazine) | Folic acid |
| Pyridoxine (vitamin B 6) |
Due to frequently occurring side effects and complications, the simultaneous use of COCs and bromocriptine (parlodel), ergot alkaloids (ergotamine), dopegite (methyldopa, aldomet), antipyrine, ketoconazole (orally only) is not recommended. In addition to the possible influence of COCs on the effectiveness of various concomitantly taken medications, one should definitely take into account the effect of various drugs on the main and main property of COCs - contraceptive activity.
This data is constantly being supplemented, modified and improved, but it has now been established that the effectiveness of hormonal contraceptives
is significantly reduced by:
- Antacids containing magnesium;
- Anticonvulsants and antiepileptic drugs (hexamidine, carbamazepine, tegretol, diphenin, ethosuximide, etc.);
- Barbiturates (in particular phenobarbital);
- Meprobamate (meprotan, andaxin);
- Nitrofurans (furadonin);
- Imidazoles (metronidazole, flagyl, Klion, trichopolum, tinidazole, etc.);
- Sulfonamides and trimethoprim (in particular, their combination - Biseptol, Bactrim);
- Some anti-tuberculosis drugs (in particular, isoniazid);
- Phenylbutazone (butadione), indomethacin;
- Butamide.
Particular caution must be observed when prescribing COCs and antibiotics
, in particular, having an effect on the intestinal microflora, since the latter can reduce the absorption of estrogens from the intestine, preventing them from achieving their effective concentrations in the blood. There is a rather original recommendation (Boroyan R. G., 1999) to increase the dose of COCs for the entire period of taking antibiotics and for two weeks after the end of the course of therapy. Antibiotics that significantly reduce the contraceptive effectiveness of COCs include: rifampicin and its analogues, penicillin and semisynthetic penicillins ( phenoxymethylpenicillin, ampicillin, amoxicillin, augmentin, etc.), griseofulvin, the entire tetracycline group (doxycycline, vibramycin, metacycline), chloramphenicol (chloramphenicol). To a lesser extent, the contraceptive effectiveness of COCs is affected by cephalexin and other cephalosporins, clindamycin (Dalacin), macrolide antibiotics (in particular, erythromycin), neomycin and its analogues. The occurrence of intermenstrual bleeding observed during the simultaneous use of COCs and other drugs may actually reflect a decrease contraceptive activity
Remembering the well-known saying about “God-protected” and “the frightened crow that is afraid of the bush” (in our context - pregnancy), in our practical activities we are guided by the principle set out in the above sayings, recommending the so-called “safety net contraception”. Its meaning is that the patient taking any drug (except for one-time use, for example, paracetamol for headaches) simultaneously with a COC must be accompanied by an indispensable
using barrier (condom, cap, diaphragm), spermicidal or even usually not recommended (coitus interruptus) methods of contraception until the end of a given menstrual cycle. This recommendation is especially relevant due to the current availability of a myriad of drugs from new pharmacological groups, their synonyms, analogues, etc., the interaction of which with COCs has not yet been sufficiently studied or is completely unknown...
Issues of drug interactions are very relevant, but, unfortunately, have not been sufficiently studied and covered in the medical literature. We absolutely agree with the opinion of S. N. Panchuk and N. I. Yabluchansky (2002) that “the key link in ensuring drug safety is the practicing physician. His awareness of these issues, concern and active life position are important components of safe pharmacotherapy.”
LITERATURE
- Bagdan Sh. Modern pregnancy prevention and family planning, trans. from Hungarian, Graphite Pensil, Budapest, 1998.
- Boroyan R. G. Clinical pharmacology for obstetricians and gynecologists, Medical Information Agency, Moscow. 1999.
- Derimedved L.V., Pertsev I.M., Shuvanova E.V., Zupanets I.A., Khomenko V.N.. Interaction of drugs and the effectiveness of pharmacotherapy, Kharkov, Megapolis, 2002.
- Mayorov M.V. Some aspects of hormonal contraception // Pharmacist, 2002, No. 1, January, p. 43-44.
- Mayorov M.V. Contraception: modern principles, methods, drugs // Medicine and..., 1999, No. 2 (5), p. 8-14.
- Panchuk S.N., Yabluchansky N.I., Drug safety // Medicus Amicus, 2002, No. 6, p. 12-13.
- Guide to contraception / Russian international publication, Bridging The Gap Communications. Inc. Decatur, Georgia, USA, 1994.
- Darcy PF Drug interactions with oral contraceptives // Drug. Intel. Clin. Pharm., 1986, 20:353-62.
- Miller D. M, Helms S. E, Brodell RT A practical approach to antibiotic treatment in women taking oral contraceptives // J. Am. Acad. Dermatol 1998, 30:1008-11.
- 10. Shenfield GM Drug interacts with oral contraceptive preparations // Med. J Aust. 1986, 144:205-211.
- 11. Shenfield GM Oral Contraceptives. Are drug interactions of clinical significance? //Drug. Safety, 1998, 9(1):21-37.
Oral contraception in its modern understanding arose already in the second half of the last century and came into use only a few decades ago, having made, albeit a quiet, but almost revolutionary revolution in the life of the female population of the planet. The ability to control one’s reproductive function reliably and without compromising one’s personal life has made life much easier for millions of women, giving them additional opportunities to plan their destiny and family, build a career, and develop spiritually and intellectually. Therefore, it is so important to know how to choose oral contraceptives, their names, as well as when and how to use them.
The most obvious advantage of oral contraceptives is that their use is practically invisible to others or to a sexual partner. By taking the drug in accordance with the instructions (usually once a day, every day, except during menstruation), a woman has a fairly high level of protection against unwanted pregnancy.
Rating of the best birth control pills
Novinet
A combined oral contraceptive drug, the main contraceptive effect of which is to inhibit gonadotropins and suppress ovulation. In addition, by increasing the viscosity of the cervical fluid, the movement of sperm through the cervical canal slows down, and changes in the condition of the endometrium prevent the implantation of a fertilized egg.
Ethinyl estradiol is a synthetic analogue of endogenous estradiol.
Desogestrel has a pronounced gestagenic and antiestrogenic effect, similar to endogenous progesterone, and weak androgenic and anabolic activity.
Novinet has a beneficial effect on lipid metabolism: it increases the concentration of HDL in the blood plasma without affecting the content of LDL.
With the use of the drug, there is a significant decrease in the amount of monthly blood lost (with initial menorrhagia), the menstrual cycle is normalized, and a beneficial effect on the skin is noted (especially in the presence of acne vulgaris).
Advantages:
- Improves the condition of the skin (it becomes even more pleasant to the touch);
- Helps control the cycle;
- Does not cause nausea;
- During menstruation, pain disappears;
- Price - from 450 rub.
Flaws:
- You can get better from them;
- If you don’t gain weight, it will be difficult to lose weight;
- Your chest may begin to hurt;
- Possible heartburn and heaviness in the stomach;
- Some people lose libido (desire).
Charosetta
Charozetta® is a gestagen-containing oral contraceptive containing the gestagen desogestrel. Like other progestogen-containing oral contraceptives (“mini-pills”), Charozetta® is best suited for use during breastfeeding and for women who are contraindicated or who do not want to take estrogens. Unlike the “mini-pill,” the contraceptive effect of Charozetta® is achieved mainly by suppressing ovulation. Other effects include an increase in the viscosity of cervical mucus.
The package contains 28 tablets, the blister indicates the order of taking the drug. The drug should be taken following this order, one tablet per day, preferably at the same time. Take the tablet with a small amount of water. The next package begins to be taken without interruption as soon as the previous one is finished.
You should start taking it from the top of the package, so you won’t get confused and can always check whether you missed taking any pills. If bleeding occurs, do not stop taking the drug. If you want to stop taking the drug, you need to remember that its contraceptive effect will end on the day you stop taking it.
Advantages:
- The days of the week are marked on the packaging;
- Compatible with lactation;
- The missed pill rule is 12 hours.
Flaws:
- If you don't start taking pills on Monday, you might get confused;
- The need for an adaptation period;
- Frequently recurring menstruation;
- Price - 1297 - 1339 rubles.
Diana-35
Diane-35 is a low-dose monophasic oral combined estrogen-antiandrogen contraceptive drug.
The contraceptive effect of Diane-35 is carried out through complementary mechanisms, the most important of which include suppression of ovulation and changes in the properties of cervical secretion, as a result of which it becomes impenetrable to sperm.
In women taking combined oral contraceptives, the menstrual cycle becomes more regular, painful menstruation is less frequent, and the intensity of bleeding decreases, resulting in a reduced risk of iron deficiency anemia. In addition, there is evidence that the risk of developing endometrial and ovarian cancer is reduced.
While taking Diane-35, the increased activity of the sebaceous glands, which plays an important role in the occurrence of acne and seborrhea, decreases. After 3-4 months of therapy, this usually leads to the disappearance of the existing rash. Excessive oiliness in hair and skin disappears even earlier. Hair loss, which often accompanies seborrhea, is also reduced.
Therapy with Diane-35 in women of reproductive age reduces the clinical manifestations of mild forms of hirsutism (in particular, increased growth of facial hair); however, the effect of treatment should be expected only after several months of use. Along with the above-described antiandrogenic effect, cyproterone acetate also has a pronounced gestagenic effect.
Advantages:
- Weight does not change;
- Restore the cycle;
- Skin is clean;
- Critical days on time;
- Reliable;
- No pain during menstruation;
- Breasts are growing;
- Improves hair condition.
Flaws:
- Possibly the strongest side effects;
- High price;
- Increased emotionality;
- Helps with PCOS (polycystic ovary syndrome) only for the duration of use;
- Price - from 1000 rubles.
Chloe
Combined low-dose monophasic oral contraceptive drug with antiandrogenic activity. The mechanism of action is due to the antiandrogenic steroid drug it contains - cyproterone acetate and oral estrogen - ethinyl estradiol.
Advantages:
- The monthly cycle is normalized;
- No weight gain;
- Breast enlargement;
- Gives the ovaries a rest;
- Reducing pain during menstruation;
- Cosmetic effect on skin and hair.
Flaws:
- Loss of libido;
- Irritability;
- An allergic reaction is possible at the beginning of use;
- Depression before menstruation;
- Headache;
- Price - 730 - 2130 rub.
Gynepristone
Gynepristone is a synthetic steroidal antigestagenic drug - it has the property of blocking the action of progesterone at the receptor level. Its action stimulates an increase in the contractility of the myometrium, promotes the release of substances that increase the sensitivity of the myometrium to certain types of hormones.
Depending on what phase of the menstrual cycle the drug was taken, it can inhibit ovulation, promote changes in the endometrium, and also prevent the implantation of an already fertilized egg.
Advantages:
- Minimum side effects;
- Does not cause serious side effects;
- One tablet per package;
- Non-hormonal drug;
- Has a gentle effect on the body;
- Helps effectively;
- Price - from 372 rub.
Flaws:
- Possible hormonal imbalance;
- Delay;
- Possible individual intolerance
Rigevidon
Combined monophasic oral estrogen-progestin contraceptive drug.
When taken orally, it inhibits the pituitary secretion of gonadotropic hormones. The contraceptive effect is associated with several mechanisms. As a gestagenic component (progestin), it contains a derivative of 19-nortestosterone - levonorgestrel, which is more active than the corpus luteum hormone progesterone (and a synthetic analogue of the latter - pregnin), acts at the receptor level without preliminary metabolic transformations. The estrogenic component is ethinyl estradiol.
Under the influence of levonorgestrel, the release of releasing hormones (LH and FSH) from the hypothalamus is blocked, the secretion of gonadotropic hormones by the pituitary gland is inhibited, which leads to inhibition of the maturation and release of an egg ready for fertilization (ovulation). The contraceptive effect is enhanced by ethinyl estradiol. Maintains high viscosity of cervical mucus (makes it difficult for sperm to enter the uterine cavity). Along with the contraceptive effect, when taken regularly, it normalizes the menstrual cycle and helps prevent the development of a number of gynecological diseases, incl. tumor nature.
Advantages:
- Good condition of skin, hair and nails;
- Reliable contraception;
- Normalizes the menstrual cycle;
- No intermediate bleeding;
- Smooth cycle;
- The chest is not heavy;
- Stable weight;
- Eliminates PMS;
- Price - 244 - 546 rubles.
Flaws:
- If you drink for a long time without breaks, you will experience terrible tearfulness;
- The duration of menstruation increases (individually);
- Noticeably reduces libido;
- Bad mood;
- Causes unmotivated aggression.
Tri-mercy
A combined contraceptive drug containing estrogen and gestagen.
The contraceptive effect of the drug, like other combined oral contraceptives, is based primarily on the ability to suppress ovulation and increase the secretion of cervical mucus.
Desogestrel suppresses the synthesis of gonadotropic hormones, mostly LH, thus preventing follicle maturation (blocks ovulation).
Ethinyl estradiol is a synthetic analogue of the follicular hormone estradiol, together with the corpus luteum hormone, regulates the menstrual cycle.
Along with these central and peripheral mechanisms that prevent the maturation of an egg capable of fertilization, the contraceptive effect is due to an increase in the viscosity of the mucus in the cervix, which makes it difficult for sperm to penetrate into the uterine cavity.
In addition to contraceptive properties, the drug has a number of effects that can be taken into account when choosing a contraceptive method. Menstrual-like reactions become more regular, are less painful and are accompanied by less severe bleeding. The latter circumstance leads to a decrease in the frequency of concomitant iron deficiency anemia.
Taking contraceptives with a high content of ethinyl estradiol (50 mcg) reduces the risk of developing ovarian and endometrial cancer. There are no data to support this pharmacological effect for contraceptives with lower ethinyl estradiol content.
Advantages:
- Great mood;
- Increased libido;
- Normalizes menstruation;
- Suitable for young girls;
- Good hair grows;
- Removes acne;
- The breasts are enlarged.
Flaws:
- Possible weight gain;
- Temporary acne after withdrawal;
- Unnatural interference in women's cycles;
- Price - from 800 rub.
Tri-Regol
Combined (three-phase) oral contraceptive estrogen-progestogen drug. Inhibits the pituitary secretion of gonadotropic hormones. Sequential administration of tablets containing varying amounts of progestin (levonorgestrel) and estrogen (ethinyl estradiol) provides concentrations of these hormones in the blood close to their concentrations during the normal menstrual cycle and promotes secretory transformation of the endometrium.
The contraceptive effect is associated with several mechanisms. Under the influence of levonorgestrel, the release of releasing factors (LH and FSH) of the hypothalamus is blocked, the secretion of gonadotropic hormones by the pituitary gland is inhibited, which leads to inhibition of the maturation and release of an egg ready for fertilization (ovulation). Ethinyl estradiol maintains the high viscosity of cervical mucus (it makes it difficult for sperm to enter the uterine cavity). Along with the contraceptive effect, the menstrual cycle is normalized by replenishing the level of endogenous hormones with the hormonal components of Tri-Regol tablets. In 7-day periods, when the next break in taking the drug follows, uterine bleeding occurs.
Advantages:
- Reliable;
- No side effects;
- Close to the hormonal background of a woman;
- Clean skin;
- Price - from 350 rub.
Flaws:
- There are age restrictions;
- Take strictly by the hour.
Silhouette
Siluet® is an oral combination drug with an antiandrogenic effect, containing ethinyl estradiol (EE) as an estrogen and dienogest (DNG) as a progestogen.
The contraceptive effect of the drug Siluet® is due to various factors, the most important among them are inhibition of ovulation, increased viscosity of cervical mucus, changes in peristalsis of the fallopian tubes and endometrial structure.
The antiandrogenic effect of the combination of EE and DNG is based on a decrease in the concentration of androgens in plasma.
Repeated studies have shown that taking a combination of EE with DNG led to the elimination of symptoms of mild to moderate acne and had a positive result in patients with seborrhea.
DNG is a derivative of norethisterone, which has a 10-30 times lower affinity for progesterone receptors in vitro compared to other synthetic progesterones. DNG has no significant androgenic, mineralocorticoid, or glucocorticoid effects in vivo.
When administered alone at a dose of 1 mg/day, DNG inhibits ovulation.
Advantages:
- Painless menstruation;
- Does not affect weight;
- Helps with endometriosis;
- Inhibits the development of adenomyosis;
- No heavy discharge;
- Contraceptive effect;
- Breast enlargement
- Skin improves, acne disappears;
- Regular cycle;
- Price - from 560 rub.
Flaws:
- Difficult period of adjustment;
- Sexual desire decreases.
Lindinet 20
Monophasic oral contraceptive. Inhibits the secretion of gonadotropic hormones of the pituitary gland. The contraceptive effect of the drug is associated with several mechanisms. The estrogenic component of the drug is ethinyl estradiol, a synthetic analogue of the follicular hormone estradiol, which participates together with the corpus luteum hormone in the regulation of the menstrual cycle. The gestagenic component is a derivative of 19-nortestosterone - gestodene, which is superior in strength and selectivity to not only the natural hormone of the corpus luteum progesterone, but also other synthetic gestagens (for example, levonorgestrel). Due to its high activity, gestodene is used in low dosages, in which it does not exhibit androgenic properties and has virtually no effect on lipid and carbohydrate metabolism.
Along with the indicated central and peripheral mechanisms that prevent the maturation of an egg capable of fertilization, the contraceptive effect is due to a decrease in the susceptibility of the endometrium to the blastocyst, as well as an increase in the viscosity of the mucus located in the cervix, which makes it relatively impenetrable for sperm.
In addition to the contraceptive effect, the drug, when taken regularly, also has a therapeutic effect, normalizing the menstrual cycle and helping to prevent the development of a number of gynecological diseases, incl. tumor nature.
Advantages:
- Menstruation is painless;
- Reliable protection against pregnancy;
- Does not cause nausea;
- Does not reduce libido;
- Smooth emotional background;
- Good skin;
- Breast enlargement;
- Good mood;
- Price - from 460 rub.
Flaws:
- Chest pain;
- Veins pop out;
- Slight weight gain;
- Varicose veins get worse.
Midiana
Combined oral contraceptive containing ethinyl estradiol and drospirenone. The contraceptive effect is based on the interaction of various factors, the most important of which are inhibition of ovulation and changes in the endometrium.
At a therapeutic dose, drospirenone also has antiandrogenic and weak antimineralocorticoid properties. Does not have estrogenic, glucocorticoid and antiglucocorticoid activity. This provides drospirenone with a pharmacological profile similar to natural progesterone.
There is evidence of a reduced risk of developing endometrial and ovarian cancer when using combined oral contraceptives.
Advantages:
- Painless menstruation;
- Reliability;
- Cosmetic effect;
- Therapeutic effect;
- You don't gain weight;
- Low hormone levels;
- Breasts are growing;
- Protects against pregnancy;
- Regulates hormonal levels.
Flaws:
- Possible decrease in libido;
- By-effect;
- Price - from 650 rub.
Marvelon
A combined contraceptive drug containing estrogen and gestagen.
The contraceptive effect of the drug, like other combined oral contraceptives, is based primarily on the ability to suppress ovulation and increase the secretion of cervical mucus.
Desogestrel suppresses the synthesis of gonadotropic hormones, mostly LH, thus preventing follicle maturation (blocks ovulation).
Ethinyl estradiol is a synthetic analogue of the follicular hormone estradiol, together with the corpus luteum hormone, regulates the menstrual cycle.
Along with these central and peripheral mechanisms that prevent the maturation of an egg capable of fertilization, the contraceptive effect is due to an increase in the viscosity of the mucus in the cervix, which makes it difficult for sperm to penetrate into the uterine cavity.
In addition to contraceptive properties, the drug has a number of effects that can be taken into account when choosing a contraceptive method. Menstrual-like reactions become more regular, are less painful and are accompanied by less severe bleeding. The latter circumstance leads to a decrease in the frequency of concomitant iron deficiency anemia.
Taking contraceptives with a high content of ethinyl estradiol (50 mcg) reduces the risk of developing ovarian and endometrial cancer. There are no data to support this pharmacological effect for contraceptives with lower ethinyl estradiol content.
Advantages:
- Reliable;
- Doesn't gain weight;
- Increases libido;
- No PMS;
- Indicated for mastopathy;
- No headache;
- Prevents cysts;
- Has almost no contraindications;
- Great skin.
Flaws:
- Mild nausea is possible;
- Sensitive breasts;
- Not suitable for everyone;
- Occasionally headache;
- Price - from 1250 rub.
Janine
Zhanine is a low-dose monophasic oral combined estrogen-progestogen contraceptive drug.
The contraceptive effect of Janine is carried out through complementary mechanisms, the most important of which include suppression of ovulation and a change in the viscosity of cervical mucus, as a result of which it becomes impermeable to sperm.
When used correctly, the Pearl index (an indicator reflecting the number of pregnancies in 100 women taking a contraceptive during the year) is less than 1. If pills are missed or used incorrectly, the Pearl index may increase.
The progestin component of Janine, dienogest, has antiandrogenic activity, which is confirmed by the results of a number of clinical studies. In addition, dienogest improves the blood lipid profile (increases the amount of high-density lipoproteins).
In women taking combined oral contraceptives, the menstrual cycle becomes more regular, painful menstruation is less frequent, the intensity and duration of bleeding decreases, resulting in a reduced risk of iron deficiency anemia. In addition, there is evidence of a reduced risk of endometrial and ovarian cancer.
Advantages:
- Painless CD;
- Critical days are shortened;
- Prevention of cystic processes;
- Clean skin;
- Hair becomes less greasy;
- Does not cause weight gain;
- Protects against unwanted pregnancy;
- The breasts are enlarged.
Flaws:
- Mood swings;
- Side effects;
- Reduces libido;
- Price - 991 - 2536 rubles.
Lactinet
Lactinet-Richter is a gestagen-containing contraceptive for oral use, the active ingredient of which is desogestrel.
Like other gestagen-containing oral contraceptives (mini-pills), Lactinet-Richter is best suited for use during breastfeeding and for women who are contraindicated or who do not want to take estrogens. Unlike the mini-pill, the contraceptive effect of Laktinet-Richter is achieved mainly by suppressing ovulation. Other effects include an increase in the viscosity of cervical mucus.
When using the drug Lactinet-Richter in the first 56 days, the frequency of ovulation does not exceed 1%; after stopping the 56-day drug intake, ovulation occurs after 7-30 days (on average after 17 days).
In a comparative effectiveness study (in which missed pills were allowed to be taken within a maximum of 3 hours), the overall Pearl index (an indicator reflecting the pregnancy rate in 100 women during a year of contraceptive use) of desogestrel was 0.4 in the group of all patients included in the study.
The Pearl index of Lactinet-Richter is comparable to the Pearl index of combined oral contraceptives (COCs) in the general population of women taking oral contraceptives. Taking the drug Lactinet-Richter leads to a decrease in the concentration of estradiol in the blood plasma to values characteristic of the early follicular phase. At the same time, no clinically significant changes were detected in carbohydrate, lipid metabolism and hemostasis parameters.
Advantages:
- Easy to carry;
- Safe for baby
- Suitable for nursing mothers, Does not affect lactation;
- Stops the growth of fibroids;
- No external side effects;
- Do not depend on the cycle;
- Modern drug.
Flaws:
- Side effects;
- Price - 756 - 810 rub.
Jess
The drug Jess is a combined hormonal contraceptive with antimineralocorticoid and antiandrogenic effects.
The contraceptive effect of combined oral contraceptives is based on the interaction of various factors, the most important of which include suppression of ovulation and changes in the properties of cervical secretion, as a result of which it becomes less permeable to sperm.
When used correctly, the Pearl index (the number of pregnancies per 100 women per year) is less than 1. If pills are missed or used incorrectly, the Pearl index may increase.
In women taking combined oral contraceptives, the menstrual cycle becomes more regular, painful menstruation is less common, and the intensity of bleeding decreases, which reduces the risk of anemia. In addition, according to epidemiological studies, the use of combined oral contraceptives reduces the risk of developing endometrial and ovarian cancer.
Advantages:
- Hair does not fall out;
- Cosmetic effect;
- Reduces PMS;
- Breast enlargement;
- Clean face.
Flaws:
- Risk of developing thrombosis;
- Price - 1041 - 3189 rub.
Flaws
- A constant desire to protect yourself from pregnancy and daily use is required.
After discontinuation of use, there may be some delay in the restoration of fertility.
Violation of the medication regimen significantly increases the risk of pregnancy.
When taking certain medications simultaneously (for example, anticonvulsants, antituberculosis drugs), the effectiveness of contraception may be reduced.
It is necessary to have the ability to constantly replenish the supply of the drug.
Some nausea, dizziness, slight tenderness of the mammary glands, headaches, and slight spotting are possible.
Short-term changes in the psycho-emotional background (mood, libido) are possible.
There may be a slight change in body weight.
In rare cases, serious complications such as stroke, blood clots in the lungs, etc. are possible.
This method of contraception does not protect or reduce the risk of developing sexually transmitted diseases.
Categories of women who are not recommended to use combined oral contraceptives
- Pregnant women (with established or suspected pregnancy).
Women who are breastfeeding.
Women who have unexplained vaginal bleeding (until the cause is determined).
Women with active liver disease (viral hepatitis).
Smoking women over 35 years of age.
Women with a history of high blood pressure (>180/110 mm Hg) and/or stroke, heart attack.
Women with a history of blood coagulation disorders.
Women with a history of complicated diabetes mellitus.
Women with breast cancer (past or current).
Women suffering from migraines and having focal neurological symptoms.
Women taking anticonvulsant and/or antituberculosis drugs.
Criteria for selecting combined oral contraceptives
The basic principle of choosing a drug when prescribing hormonal contraception is to use the smallest dose of steroids that would be sufficient to provide reliable protection against unwanted pregnancy. It is especially important to observe this principle when using hormonal contraception for the first time in early reproductive age. According to modern views, it is recommended to give preference to drugs in which the dose of estrogens does not exceed 30-35 mcg, and the dose of progestins should not be higher than the equivalent of 150 mcg of levonorgestrel or 1 mg of norethisterone. When choosing a drug, you should take into account the constitutional type of the woman, medical history, gynecological and endocrinological examination.
Preparations containing a high dose of estrogen (more than 50 mcg) are still produced and available in pharmacies. However, these drugs are currently used primarily for therapeutic purposes.
- With heavy and long menstruation, drugs with an enhanced gestagen component are more likely to be better tolerated; with short and scanty menstruation, drugs with an enhanced estrogen component are more likely to be tolerated.
For women with increased sensitivity to estrogens (nausea, vomiting, headache, tension in the mammary glands, increased vaginal mucus formation, hypermenorrhea, cholestasis, varicose veins), it is advisable to prescribe combined oral contraceptives with a pronounced gestagenic component (ovidone, continuin, ovrette, cilest, trinovum, microgynon ).
For women with increased sensitivity to gestagens (fatigue, depression, decreased libido, hypomenorrhea, amenorrhea, seborrhea, acne, hirsutism), the drugs of choice are combined oral contraceptives with a pronounced estrogenic component (anteovin, non-ovlon, marvelon, etc.).
In women under the age of 18 and after 40 years, preference should be given to drugs with a minimal content of estrogens and gestagens.
Teenagers should not use long-acting medications, as they contain high doses of steroid hormones (estrogens and gestagens) and are poorly tolerated.
Oral contraceptives (OCs) are highly effective modern contraceptives used by women all over the world.
Oral contraception as a way to prevent unwanted pregnancy has been practiced since the 50s of the last century.
Since then, this method of contraception has allowed doctors to accumulate impressive experience in its use. Oral contraceptives themselves have also undergone evolution, becoming more advanced in their composition and producing fewer side effects.
Contraceptives by age
Contraceptives should be chosen according to age characteristics.
From 20 to 30 years
During this period, the girl’s body was already fully formed. Any type of contraceptive is suitable. However, it is recommended to give preference to products with a high content of hormones.
Low dosage drugs are recommended for those girls who have high levels of progesterone in the body.
After 30 years
Women who have already given birth are advised to choose drugs with a low dosage of hormones. In addition, by this period, doctors advise purchasing single-phase drugs.
After 35 years
During this period, women's hormonal levels decrease, so hormonal disruptions are more common. In addition, after 35 years, women often no longer plan pregnancy. It is for this reason that it is recommended to choose products with a microdose or mini-pill.
After 45 years
In this age period, contraception is simply necessary for women. This is due to the fact that after 45 years of age, the risk of fetal developmental abnormalities, as well as other complications during pregnancy, increases.
Most often, women at this age choose single-component products. They guarantee maximum protection and at the same time have a minimal list of side effects.
What are oral contraceptives made of?
Conventionally, all oral contraceptives are divided into two groups: combined oral contraceptives (COCs) and progestogen-only contraceptive pills (POPs).
COCs are tablets containing two female sex hormones, estrogen and progestogen, obtained synthetically. Based on the ratio of these hormones, there are monophasic, biphasic and multiphasic COCs. There are also differences regarding the dose of estrogen, which are divided into high-dose, low-dose and micro-dose preparations.
Gynecologists often prescribe pills with minimal estrogen content.
Types of contraceptive COCs. How do hormonal differ from non-hormonal?
Non-hormonal drugs are intended to be inserted directly into the vagina. Such means of protection against unwanted pregnancy are considered one of the safest. This is explained by the fact that the tablets do not contain hormones; in addition, the products have a bactericidal effect and protect the genitals from the development of infection.
Preparations containing hormones are called oral contraceptives (OCs). They are distinguished by the highest degree of protection and reliability. Note that hormonal pills not only protect against unwanted pregnancy, but also increase the level of hormones when they are deficient in the female body.
Hormonal drugs are divided into two types: combined oral contraceptives and mini-pills.
Combination drugs include 2 types of hormones:
- progesterone, which is essential for the ovulation process;
- synthetic analogue of estrogen.
COCs come in different hormone dosage options: low-, micro-, and high-dose.
How do oral contraceptives work?
The use of oral contraceptives leads to the following processes:
- The absence of ovulation underlies the main contraceptive effect. No ovulation - no pregnancy.
- Increased thickness of cervical mucus. Thus, the barrier ability of cervical mucus increases, and this prevents sperm from penetrating into the uterine cavity.
- Changes in the endometrium of the uterus. The nature of the changes in the endometrium prevents the attachment of the fertilized egg if fertilization does occur.
- Influences the motility of sperm in the fallopian tubes, which contributes to the prevention of fertilization.
Why is the use of oral contraceptives so popular?
- Firstly, the efficiency of the method is very high. According to studies, out of 100 women using birth control pills, only three become pregnant.
- Secondly, the contraceptive effect begins from the moment you take the first pill. Before starting to use the method, you do not need to be specifically examined by a gynecologist. And if suddenly you want a child, you can simply stop taking the pills, and pregnancy will come very soon.
- Thirdly, you can derive a number of benefits from the non-contraceptive effects of birth control pills, namely: menstruation will become regular, painless, and the amount of blood lost will decrease. The use of oral contraceptives significantly reduces the likelihood of cancer of the ovaries, uterus, breast, rectum, inflammation of the pelvic organs, has a positive effect on the condition of the skin and in 90% of cases reduces the risk of ectopic pregnancy.
The benefits of taking oral contraceptives
- A high level of protection against unplanned conception and peace of mind without the fear of becoming pregnant.
- While taking contraceptives, the menstrual cycle becomes regular, pain and signs of PMS disappear.
- With the correct selection of contraceptives, hormone levels are normalized, which leads to an improvement in the condition of the skin and hair, and the disappearance of acne. Products with an antiandrogynous effect based on drospirenone (Jess, Yarina, etc.) have a positive cosmetic effect.
- During the period of taking hormonal contraceptives, the ovaries “rest”, which contributes to the rapid return of fertility and the onset of a planned pregnancy. There is also an opinion that such ovarian rest has a therapeutic effect and reduces the risk of cancer of the female reproductive system, and also stops the development of endometriosis, but there is no medical evidence for this fact.
- Some COCs are used as medications in the treatment of hormone-dependent gynecological diseases and some forms of infertility.
What side effects may oral contraceptives have?
The most common side effects are nausea, dizziness, mood changes, heaviness in the mammary glands, slight weight gain (2-3 kg), spotting from the vagina, changes in libido. These effects are not symptoms of any disease, and often disappear after 2-3 cycles of taking the pills.
Attention! Oral contraceptives do not protect against sexually transmitted infections and HIV.
The use of St. John's wort-based antidepressants, drugs against tuberculosis and seizures may reduce the effectiveness of PC. Be sure to tell your doctor if you use any of these products!
New generation birth control pills
When comparing new generation contraceptives with drugs from an earlier period, it turns out that birth control pills, as they are in modern medicine, are superior to their ancestors in all respects.
All contraceptive medications are equally effective and ideal in quality. Contraindications mainly depend on the individual body of the woman. New generation drugs, in addition to their contraceptive function, also treat some female diseases and infectious diseases.
Many women avoid hormonal contraceptives, preferring non-hormonal drugs: suppositories, ointments, gels. It should be borne in mind that non-hormonal contraceptives are made on a chemical basis, therefore, they are not suitable for those who have the slightest female problems.
Of the five generations of birth control drugs, doctors prefer the last three.
Who are contraindicated for PCs?
Should not be used by women who have the following conditions:
- Suspected or established pregnancy.
- Lactation. The ban applies to COCs, but does not apply to PTPs, which are allowed during breastfeeding.
- Severe diseases of the liver and gall bladder.
- Already existing diseases of the cardiovascular system (thrombosis, strokes, coronary heart disease), or if they existed before.
- High blood pressure from 140/90 mm Hg. Art. and higher.
- Blood clotting disorders.
- Migraine.
- Breast cancer.
- Diabetes mellitus with complications.
- Smoking, age over 35 years (contraindication applies only to COCs).