| Pulmonary embolism | |
| CT picture of thromboembolism of the main pulmonary arteries during CT angiopulmonography. | |
| ICD-10 | 26. |
| ICD-9 | 415.1415.1 |
| DiseasesDB | 10956 |
| MedlinePlus | 000132 |
| eMedicine | med/1958 emerg/490emerg/490 radio/582radio/582 |
| MeSH | D011655 |
Pulmonary embolism
(PE) is a blockage of the pulmonary artery or its branches by blood clots, which often form in the large veins of the lower extremities or pelvis (embolism).
In foreign literature, a broader concept is widespread: pulmonary embolism
, which also includes rare air emboli, fat embolism, embolism with amniotic fluid, foreign bodies, and tumor cells.
Content
- 1 Epidemiology
- 2 Causes and risk factors
- 3 Pathogenesis
- 4 Classification
- 5 Clinical picture
- 6 Diagnostics 6.1 Laboratory diagnostic methods 6.1.1 Determination of d-dimer levels
- 6.2.1 Electrocardiography
- 7.1 Correction of hemodynamics and hypoxia
Pulmonary embolism: treatment
Stabilization of the patient's condition
- Until the diagnosis of PE is excluded, a patient suspected of having this disease should be treated according to the principles of PE therapy.
- Check heart rate, pulse, blood pressure, respiratory rate every 15 minutes against the background of constant monitoring of pulse oximetry and cardiac activity. You should ensure that you have all the necessary equipment for mechanical ventilation.
- Provide venous access and begin intravenous infusion (crystaploid or colloid solutions).
- Provide the maximum possible concentration of oxygen inhaled through a mask to eliminate hypoxia. Mechanical ventilation is indicated when the patient experiences fatigue of the respiratory muscles (one should beware of collapse when administering sedatives before tracheal intubation).
- LMWH or UFH is prescribed to all patients with a high and moderate risk of PE even before the diagnosis is confirmed. A meta-analysis of multicenter studies showed advantages of LMWH over UFH in terms of mortality and bleeding rates. For heparin dosage, please refer to the specific hospital protocol.
- In case of hemodynamic instability (hypotension, signs of right ventricular failure) or cardiac arrest, improvement is achieved by thrombolysis with recombinant tissue plasminogen activator or streptokinase [at the same dose as in the treatment of ST-segment elevation AMI].
Anesthesia
- NSAIDs may be effective.
- Narcotic analgesics should be prescribed with caution. The vasodilation they cause may potentiate or aggravate hypotension. 1-2 mg of diamorphine is administered slowly. For hypotension, intravenous administration of colloidal infusion solutions is effective.
- Avoid intramuscular injections (dangerous during anticoagulant and thrombolytic therapy).
Anticoagulant therapy
- Once the diagnosis is confirmed, the patient should be prescribed warfarin. It must be administered concomitantly with LMWH (UFH) for several days until MHO reaches therapeutic levels. In most cases, the target MHO is 2-3.
- The standard duration of anticoagulant therapy is:
- 4-6 weeks in the presence of temporary risk factors;
- 3 months for the first idiopathic case;
- at least 6 months in other cases;
- in case of repeated cases or the presence of factors predisposing to thromboembolism, lifelong use of anticoagulants may be required.
Heart failure
- Massive pulmonary embolism may manifest as cardiac arrest secondary to electromechanical dissociation. Other causes of electromechanical dissociation should be excluded.
- Carrying out chest compressions can lead to the splitting of the blood clot and its advancement into more distal branches of the pulmonary artery, which to some extent helps restore cardiac activity.
- If there is a high probability of PE and there are no absolute contraindications for thrombolysis, recombinant tissue plasminogen activator is prescribed [at the same dose as for ST-segment elevation AMI, maximum 50 mg followed by heparin].
- When restoring cardiac output, the issue of angiography of the pulmonary vessels or catheterization of the pulmonary artery is decided for the purpose of mechanical destruction of the thrombus.
Hypotension
- An acute increase in vascular resistance in the lungs leads to dilatation of the right ventricle and pressure overload, which makes it difficult to fill the left ventricle and leads to disruption of its function. These patients require higher right heart filling pressures, but their condition may worsen due to fluid overload.
- For hypotension, colloidal infusion solutions (500 ml of hydroxyethyl starch) are prescribed.
- If hypotension persists, invasive monitoring and inotropic therapy may be required. In such cases, jugular venous pressure is a poor indicator of right heart filling pressure. Among inotropic drugs, epinephrine is the most preferred.
- Femorofemoral cardiopulmonary bypass can be used to maintain circulation until thrombolysis or surgical embolectomy.
- Angiography of pulmonary vessels in patients with hypotension is dangerous, since the radiocontrast agent can cause dilation of blood vessels in the systemic circulation and collapse.
Embolectomy
- If thrombolytic therapy is contraindicated, as well as in shock requiring inotropic therapy, embolectomy is possible, provided that there is sufficient experience to carry out this manipulation.
- Embolectomy can be performed via a percutaneous approach in a specialized operating room or during surgery while on cardiopulmonary bypass.
- Percutaneous intervention can be combined with peripheral or central thrombolysis.
- You should seek advice from a specialist as soon as possible. The effectiveness of therapy is higher if it is started before the development of cardiogenic shock. Before performing thoracotomy, it is advisable to obtain radiological confirmation of the extent and level of thromboembolic occlusion of the pulmonary vessel.
- Mortality is 25-30%.
Kava filter
- It is rarely installed, as it has little effect on improving early and late mortality rates.
- Filters are placed via a percutaneous approach and, if possible, patients should continue to take anticoagulants to prevent further thrombus formation.
- Most filters are installed in the infrarenal part of the inferior vena cava (bird's nest filters), but installation in the suprarenal part (Greenfield filter) is also possible.
Indications for installation of a vena cava filter include:
- ineffectiveness of anticoagulant therapy, despite the use of adequate doses of drugs;
- prophylaxis in high-risk patients: for example, progressive venous thrombosis, severe pulmonary hypertension.
Epidemiology
PE is a relatively common cardiovascular pathology (approximately 1 case per thousand population per year)[1]. In the United States, PE affects approximately 650,000 people and results in 350,000 deaths per year[2]. PE occurs more often in the elderly (In the United States, venous thromboembolism occurs for the first time in about 100 out of 100,000 people per year and increases exponentially from less than 5 cases per 100,000 people in children under 15 years of age to 500 cases per 100,000 people at age 80 years) [3]. Data on the association of gender with PE vary, but an analysis of a US national database found that men have a 20% to 30% higher mortality rate than women.[4] The incidence of venous thromboembolism among the elderly is higher in men, but in patients under 55 years of age it is higher in women[5].
Algorithm of actions
Statistics show that the mortality rate from pulmonary infarction caused by thromboembolism is extremely high. All possible assistance to a patient who is expected to stop breathing should be provided immediately.
First of all, you need to call an ambulance. And then do everything possible to make it easier for the person to breathe. Open all windows, if there is a tie, remove it. In addition, you must:
- Unbutton the collar of your clothing.
- Place the patient on a flat surface.
- Find out if he has chronic heart problems or allergies.
- Find out if the victim has epilepsy attacks.
- Watch your pulse and general condition.
- When the pulse stops, perform artificial respiration and cardiac massage, standard in such cases.
Almost 50% of people whose embolus travels through the heart to the lungs die because there is no one to provide adequate assistance until doctors arrive.
First aid for pulmonary embolism is to prepare the patient for the arrival of the ambulance. Doctors will immediately carry out anti-shock therapy and endotracheal intubation. But before this therapy, he can be given Analgin as a pain reliever. In 10-15% of cases, according to official data, after an embolism of a large pulmonary artery, a person develops a pulmonary infarction. Then the blood pours out of the vessel directly into the lung tissue and provokes arterial hypoxemia or hemorrhagic pleurisy.
Important information: How to treat thrombocytopenic purpura in newborns (adults) and Werlhof's disease (thrombocytopenia) during pregnancy
Causes and risk factors
The disease is based on thrombus formation, which is facilitated by three factors (Virchow’s triad): impaired blood flow, damage to the endothelium of the vascular wall, hypercoagulation and inhibition of fibrinolysis.
Impaired blood flow is caused by varicose veins, compression of vessels from the outside (tumor, cyst, bone fragments, enlarged uterus), destruction of venous valves after phlebothrombosis, as well as immobilization, which disrupts the function of the muscular-venous pump of the lower extremities. Polycythemia, erythrocytosis, dehydration, dysproteinemia, and increased fibrinogen levels increase blood viscosity, which slows blood flow.
When the endothelium is damaged, the subendothelial zone is exposed, which triggers a cascade of blood clotting reactions. The reasons for this are direct damage to the vessel wall during the installation of intravascular catheters, filters, stents, vein replacement, trauma, and surgery. Hypoxia, viruses, and endotoxins also cause damage to the endothelium. During a systemic inflammatory reaction, leukocytes are activated, which, by attaching to the endothelium, damage it.
The source of blood clots in PE most often are the veins of the lower extremities (lower extremity venous thrombosis), much less often - the veins of the upper extremities and the right side of the heart. The likelihood of venous thrombosis increases in pregnant women, in women who have taken oral contraceptives for a long time, in patients with thrombophilia.
According to the recommendations of the European Society of Cardiology (English)Russian. In 2008, patients were stratified into high- and low-risk groups. The latter is also divided into moderate and low risk subgroups. High risk - the risk of early death (in hospital or within 30 days after pulmonary embolism) is more than 15%, moderate - no more than 15%, low - less than 1%[6]. To determine it, three groups of markers are taken into account: clinical markers, markers of right ventricular dysfunction and markers of myocardial damage.
The probability of pulmonary embolism is also assessed using the Wells score
, 2001)[7].
| Index | Points |
| Clinical symptoms of deep vein thrombosis of the lower extremities (objective swelling of the lower extremity, painful palpation) | 3 |
| PE is more likely than other pathologies | 3 |
| Tachycardia >100 beats/min | 1,5 |
| Immobilization or surgery within the last 3 days | 1,5 |
| History of deep vein thrombosis of the lower extremities or pulmonary embolism | 1,5 |
| Hemoptysis | 1 |
| Oncological pathology currently or up to 6 months ago | 1 |
If the total score is <2, the probability of pulmonary embolism is low; 2-6 points - moderate; >6 points – high.
The Geneva scale (2006)[8] is often used.
| Index | Points |
| Age >65 years | 1 |
| History of deep vein thrombosis of the lower extremities or pulmonary embolism | 3 |
| Surgery or fracture within the past month | 2 |
| Oncological pathology | 2 |
| Suspicion of deep vein thrombosis of the lower extremities (pain in one limb) | 3 |
| Hemoptysis | 2 |
| Tachycardia 75-94 beats/min | 3 |
| Tachycardia ≥ 95 beats/min | 5 |
| Pain on palpation of the vein + swelling of one limb | 4 |
If the total score is <3, the probability of pulmonary embolism is low; 4-10 points – moderate; ≥ 11 points – high.
PE reasons
Among the causes of pulmonary embolism, the following should be noted:
— acute phlebothrombosis of the veins of the lower extremities, complicated by thrombophlebitis (90% of cases);
- ileofemoral thrombosis;
— diseases of S.S.S. accompanied by increased thrombus formation in the pulmonary artery system (coronary heart disease, heart defects of rheumatic origin, heart pathologies of inflammatory and infectious nature, cardiomyopathy of various origins);
- atrial fibrillation, which results in the formation of a blood clot in the right atrium;
- generalized sepsis;
- blood diseases accompanied by impaired regulation of hemostasis (thrombophilia);
— autoimmune antiphospholipid syndrome (increased synthesis of antibodies to phospholipids of the endothelium and platelets, accompanied by an increased tendency to thrombus formation).
- sedentary lifestyle;
— concomitant diseases accompanied by cardiovascular failure;
- combination of constant use of diuretics with insufficient fluid intake;
- taking hormonal drugs;
- varicose veins of the lower extremities, which is accompanied by stagnation of venous blood and is marked by the creation of conditions for thrombus formation;
- diseases accompanied by metabolic disorders in the body (diabetes mellitus, hyperlipidemia);
— cardiac surgery and invasive intravascular manipulations.
Not all thromboses are complicated by thromboembolism, but only floating thrombi are able to break away from the vessel wall and enter the pulmonary bloodstream through the bloodstream. Most often, the source of such floating blood clots is the deep veins of the lower extremities.
Currently, a genetic theory of the occurrence of phlebothrombosis, which is the cause of pulmonary embolism, has emerged. This theory is supported by the development of thrombosis at a young age and confirmed episodes of pulmonary embolism in the patient’s relatives.
Pathogenesis
Embolization is caused by blood clots freely located in the lumen of the vein, attached to its wall only in the area of its base (floating blood clots). The detached thrombus flows through the right side of the heart into the pulmonary artery, obstructing its lumen. The consequences of this depend on the size, number of emboli, the reaction of the lungs and the activity of the body's thrombolytic system.
Thromboembolus
With small emboli there are no symptoms. Large emboli impair the perfusion of segments or even entire lobes of the lung, which leads to impaired gas exchange and the development of hypoxia. In response to this, the lumen of the vessels of the pulmonary circulation reflexively narrows, and the pressure in the pulmonary arteries increases. The load on the right ventricle increases due to high pulmonary vascular resistance caused by obstruction and vasoconstriction. Thromboembolism of small branches of the pulmonary artery is not accompanied by hemodynamic disorders and in 10% of cases pulmonary infarction and secondary infarction pneumonia develop.
Possible complications
Already a day after the arteries in the lungs are blocked by a blood clot, if a person successfully survives the first acute period, he experiences an increase in the manifestations of disorders caused by a lack of oxygen supply to all tissues of the body.
Subsequently, due to impaired cerebral circulation and saturation of brain cells with oxygen, dizziness, tinnitus, convulsions, bradycardia, vomiting, severe headache, and loss of consciousness are observed. In addition, extensive intracerebral bleeding and cerebral edema may occur, which often ends in deep fainting or even coma.
If the symptoms of thromboembolism increase slowly, the patient may experience psychomotor agitation, meningeal syndrome, polyneuritis and hemiparesis. There may be an increase in body temperature, which remains high for 2 to 12 days.
In some patients, due to circulatory disorders, the development of abdominal and immunological syndromes is observed. Abdominal syndrome is accompanied by liver swelling, belching, pain in the hypochondrium and vomiting. As a rule, if a person does not die within the first 24 hours, and comprehensive medical care was not provided, or if it turned out to be ineffective, due to a lack of oxygen supply to the lung tissues, their gradual death begins.
In severely ill patients, pulmonary infarction and infarction pneumonia already develop on days 1-3. The most dangerous complication of pulmonary embolism is multiple organ failure, which often causes death even in those patients who successfully survived the acute period of this pathological condition.
Classification
Clinically, PE is classified into the following types:
- massive - more than 50% of the volume of the vascular bed of the lungs is affected (embolism of the pulmonary trunk and/or main pulmonary arteries) and the disease manifests itself in shock and/or systemic hypotension;
- submassive - 30 - 50% of the volume of the vascular bed of the lungs is affected (embolism of several lobar or many segmental pulmonary arteries) and is manifested by symptoms of right ventricular failure;
- non-massive - less than 30% of the volume of the vascular bed of the lungs is affected (embolism of small distal pulmonary arteries), manifestations are absent or minimal (pulmonary infarction).
Classification of pulmonary embolism
Based on the volume of the arterial vascular bed excluded from the bloodstream during thrombotic occlusion, two main forms are distinguished: massive (over 45%) and non-massive (less than 45%) PE, expressed as a percentage, based on the fact that the basin of the right pulmonary artery is 55 %, each of the lower lobe branches – 20-25% of the pulmonary circulation.
Downstream (P. M. Zlochevsky, Pulmonary embolism, 1978):
- fulminant pulmonary embolism (or syncope);
- acute thromboembolism - death occurs within a few tens of minutes;
- subacute – death within a few hours or days;
- chronic form of pulmonary embolism, with progression of right ventricular failure over several months or years;
- recurrent, with repeated thromboembolisms;
- erased, latently leaking.
Clinical picture
Embolism of small branches of the pulmonary arteries may be asymptomatic or have nonspecific symptoms (slight increase in body temperature, cough).
Massive PE manifests as acute right ventricular failure with the development of shock and systemic hypotension (a decrease in blood pressure <90 mmHg or a drop of ≥40 mmHg, which is not associated with arrhythmia, hypovolemia, or sepsis). Shortness of breath, tachycardia, and fainting may occur. With submassive PE, there is no arterial hypotension, and pressure in the pulmonary circulation increases moderately. In this case, signs of dysfunction of the right ventricle of the heart and/or myocardial damage are detected, which indicates increased pressure in the pulmonary artery. With non-massive pulmonary embolism, there are no symptoms and after a few days a pulmonary infarction occurs, which is manifested by pain in the chest when breathing (due to irritation of the pleura), fever, cough and, sometimes, hemoptysis and is detected x-ray (typical triangular shadows).
During auscultation of the heart, an increase and accentuation of the second tone over the tricuspid valve and pulmonary artery is detected, as well as a systolic murmur at these points. Splitting of the second tone and gallop rhythm are possible, which is considered a bad prognostic sign. In the area of pulmonary infarction, weakened breathing, moist rales and pleural friction noise are heard.
Symptomatic manifestations of pulmonary embolism
The severity and rate of increase in symptomatic manifestations of thromboembolism largely depend on the location of the thrombus that has blocked the blood flow, the volume of blood vessels cut off from the main course, and some other factors. In most cases, acute symptoms of this pathological condition increase over 2-5 hours. It is usually characterized by manifestations of cardiovascular and pulmonary-pleural syndromes. The following signs of pulmonary embolism can be identified:
- dyspnea;
- hemoptysis;
- feeling of lack of air;
- cyanosis of the skin;
- increased body temperature;
- increased breathing;
- dry wheezing;
- general weakness;
- severe chest pain;
- tachycardia;
- positive venous pulse;
- swelling of the neck veins;
- arrhythmia;
- extrasystole.
In the absence of targeted therapy, a person’s condition steadily worsens. New symptoms appear as a result of cardiac dysfunction. The consequences of pulmonary embolism in the vast majority of cases are extremely unfavorable, since even if help is provided in a timely manner, in the future the person may experience repeated attacks of thromboembolism, the development of pleurisy, acute hypoxia of the brain, accompanied by impaired brain function, and other adverse events that can cause death or a significant decrease in quality of life. In some cases, symptomatic manifestations of respiratory and heart failure caused by thromboembolism increase so rapidly that a person dies within 10-15 minutes.
Diagnostics
Diagnosis is difficult because the symptoms of PE are not specific and diagnostic tests are imperfect. Standard testing (routine laboratory tests, electrocardiography (ECG), chest x-ray) is useful only to exclude other pathologies (eg, pneumonia, pneumothorax, rib fractures, myocardial infarction, pulmonary edema). Sensitive and specific methods for diagnosing PE include d-dimer determination, echocardiography, computed tomography (CT), ventilation-perfusion scintigraphy, pulmonary vascular angiography, as well as methods for diagnosing deep vein thrombosis of the lower extremities (ultrasonography, CT venography).[9]
Laboratory diagnostic methods
Determination of d-dimer levels
D-dimer is a fibrin breakdown product; its elevated level suggests recent thrombus formation. Determination of the level of d-dimers is a highly sensitive (more than 90%) but not specific method for diagnosing pulmonary embolism. This means that increased levels of d-dimers occur in a wide variety of other pathological conditions (eg, infection, inflammation, necrosis, aortic dissection). However, a normal level of d-dimers (<500 μg/L) allows one to exclude PE in patients with a low and intermediate probability[10].
Instrumental diagnostic methods
Electrocardiography
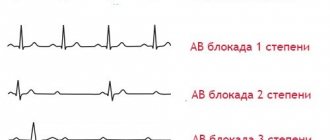
The ECG of a patient with PE shows sinus tachycardia (approximately 150 beats per minute) and right bundle branch block.
Signs of pulmonary embolism on the electrocardiogram are nonspecific and absent in most patients[11]. Sinus tachycardia and a tall and pointed P wave (P-pulmonale, a sign of right atrium overload) are often detected [12]. Approximately 20% of patients may exhibit signs of acute cor pulmonale (right ventricular overload): deviation of the electrical axis of the heart to the right; SIQIIITIII syndrome (McGinn-White syndrome[13]) - deep S wave in lead I, pronounced Q wave and negative T wave in lead III; new right bundle branch block; deep S waves in V5-6 combined with negative T waves in V1-4[14]. However, acute cor pulmonale can also occur in other acute pathologies of the respiratory system (massive pneumonia, severe attack of bronchial asthma)[15].
X-ray of the chest organs
An X-ray of the chest organs reveals signs of pulmonary hypertension of thromboembolic origin: high standing of the dome of the diaphragm on the affected side, dilation of the right heart and roots of the lung, Pall's sign (dilation of the right descending pulmonary artery), Westermarck's sign (English) Russian. (local depletion of the vascular pattern of the lung), discoid atelectasis. For pulmonary infarction - Hampton's triangle (English)Russian. (a cone-shaped compaction with the apex facing the hilum of the lungs), pleural effusion on the affected side.[11]
Echocardiography
Using echocardiography for pulmonary embolism, it is possible to detect dysfunction of the right ventricle (its dilatation and hypokinesis, bulging of the interventricular septum towards the left ventricle), signs of pulmonary hypertension, and tricuspid regurgitation. Sometimes it is possible to detect blood clots in the heart cavity (for this, transesophageal echocardiography is more informative)[16]. Also, using this method, they exclude other heart pathologies and can identify a patent foramen ovale, which can affect the severity of hemodynamic disorders and cause paradoxical embolism of the arteries of the systemic circulation[9].
Spiral computed tomography
CT angiopulmonography can detect blood clots in the pulmonary artery. With this method, the sensor rotates around the patient, who is previously injected intravenously with a contrast agent. As a result, a three-dimensional picture of the lungs is created. However, the patient must be able to hold his breath during the procedure (several seconds). The method is less invasive and safer than angiography[9]. According to experts from the European Society of Cardiology, in high-risk patients, single-detector CT is sufficient to confirm or exclude PE. In low-risk patients, multidetector CT is recommended, as it allows more clearly identifying thrombi in the branches of the pulmonary artery[17].
Ultrasound examination of the deep veins of the lower limb
Ultrasound examination (ultrasound) of peripheral veins can detect blood clots in the veins of the lower extremities. In most cases, they are the source of thromboembolism. For this, two methods are used. The first is compression ultrasound; in this case, in B-mode, a cross-section of the lumen of arteries and veins is obtained. Then the ultrasound sensor is pressed on the skin in the projection of the blood vessels. If there is a blood clot in the vein, its lumen does not decrease (compression does not occur). Another technique is Doppler ultrasound; at the same time, using the Doppler effect, the speed of blood flow in the vessels is determined. A decrease in the speed of blood flow in the veins is a possible sign of blockage by a blood clot. The combination of compression and Doppler ultrasound is called duplex ultrasonography.
Ventilation-perfusion scintigraphy
Ventilation-perfusion scintigraphy can identify areas of the lung that are ventilated but not perfused (as a result of obstruction by a thrombus). A normal lung scintigram can exclude pulmonary embolism with 90% accuracy. However, perfusion deficiency can occur in a variety of other lung pathologies. Typically, this method is used when CT is contraindicated.
Angiography of pulmonary vessels
Angiography of pulmonary vessels is the most accurate method for diagnosing pulmonary embolism, but at the same time it is invasive and has no advantages over CT. The criteria for a reliable diagnosis are a sudden break in the branch of the pulmonary artery and the contours of a blood clot; the criteria for a probable diagnosis are a sharp narrowing of the branch of the pulmonary artery and slow washout of contrast.
Etiology of the disease
Currently, pulmonary embolism is not considered an independent disease, since this pathological condition usually develops against the background of a person’s existing cardiovascular diseases. In 90% of cases of the development of a condition such as pulmonary embolism, the causes of the problem lie in various pathologies of the cardiovascular system. Pathologies of the cardiovascular system that can provoke the development of pulmonary embolism include:
- deep vein thrombosis;
- phlebeurysm;
- thrombophlebitis;
- mitral stenosis in rheumatism:
- cardiac ischemia;
- atrial fibrillation of any etiology;
- infective endocarditis;
- non-rheumatic myocarditis;
- cardiomyopathy;
- thrombophilia;
- thrombosis of the inferior vena cava.
Less commonly, blockage of blood flow in the pulmonary arteries is observed against the background of various oncological problems, respiratory diseases, autoimmune diseases and extensive injuries. Malignant tumors of the stomach, pancreas and lungs most contribute to the development of pulmonary embolism. Often, such a violation of blood flow in the lungs is associated with a generalized septic process. In addition, the appearance of PE may be a consequence of antiphospholipid syndrome, in which specific antibodies to phospholipids, platelets, nervous tissue and endothelial cells are formed in the human body, which leads to the formation of emboli.
There may be a hereditary predisposition to the development of pulmonary embolism. In addition, we can identify a number of predisposing factors for the development of pulmonary embolism, which, although they do not directly cause the development of this pathological condition, at the same time significantly contribute to it. Such predisposing factors include:
- forced bed rest for illness;
- elderly age;
- sedentary lifestyle;
- long hours behind the wheel;
- long flights;
- long course of taking diuretics;
- smoking;
- past chemotherapy;
- uncontrolled use of oral contraceptives;
- diabetes;
- open surgical interventions;
- obesity;
- frostbite;
- severe burns.
An unhealthy lifestyle greatly contributes to the formation of blood clots. For example, poor nutrition leads to a gradual increase in cholesterol and blood sugar levels, which often causes damage to individual elements of the cardiovascular system and the formation of blood clots, which can partially or completely block blood flow in one or more branches of the pulmonary artery.
Treatment
Treatment of patients with pulmonary embolism should be carried out in intensive care units.
Correction of hemodynamics and hypoxia
In case of cardiac arrest, cardiopulmonary resuscitation is performed. If hypoxia occurs in a patient with pulmonary embolism, oxygen therapy is administered (masks, nasal catheters); Artificial ventilation is less often required. To eliminate hypotension, saline solutions or vasopressors (adrenaline, dobutamine, dopamine) are administered intravenously [6].
Anticoagulant therapy
Timely anticoagulant therapy reduces the risk of death and recurrent thromboembolism, so it is recommended to start it not only with a confirmed diagnosis, but also during the diagnosis process if there is a high probability of pulmonary embolism. For this purpose, unfractionated heparin (intravenously), low molecular weight heparin is used: enoxaparin, dalteparin (subcutaneous) or fondaparinux (subcutaneous).
The dosage of unfractionated heparin is adjusted based on the patient's weight and activated partial thromboplastin time (aPTT)[18]. To do this, prepare a solution of sodium heparin - 20,000/kg per 500 ml of saline solution. First, 80 IU/kg is administered intravenously, and then an infusion is carried out at a rate of 18 IU/kg/h. 6 hours after the bolus injection, the APTT is checked and the rate of heparin administration is adjusted as indicated in the table. APTT is determined 3 hours after each speed change; when the desired level is reached (46-70 s, 1.5-2.5 times higher than control), this indicator is monitored daily.
| APTT, s | Changing dosage |
| <35 | Increase by 4 IU/kg/h |
| 35—45 | Increase by 2 IU/kg/h |
| 46—70 | Do not change |
| 71—90 | Decrease by 2 IU/kg/h |
| >90 | Stop administration for 1 hour, then reduce by 3 IU/kg/hour |
In most cases, low molecular weight heparins are used, as they are more effective, safer and more convenient to use than unfractionated heparins[19]. However, they should be prescribed with caution in cases of renal dysfunction (decreased creatinine clearance <30 ml/min) and with a high risk of hemorrhagic complications (the duration of action of unfractionated heparin is shorter and therefore can be discontinued more quickly in the event of bleeding). Of the low molecular weight heparins, the following are recommended: enoxaparin (1 mg/kg every 12 hours or 1.5 mg/kg once a day), tinzaparin (English) Russian. (175 IU/kg once a day). Dalteparin can be used in patients with cancer. (200 IU/kg once a day)[6].
For anticoagulation, fondaparinux, a selective factor Xa inhibitor, can be used. It is prescribed subcutaneously once a day at 5 mg for body weight <50 kg, 7.5 mg for 50-100 kg and 10 mg for >100 kg. It is highly effective for pulmonary embolism and does not cause thrombocytopenia, unlike heparin. However, fondaparinux is contraindicated in severe renal failure (creatinine clearance <20 ml/min)[6].
It is also advisable to prescribe warfarin on the first day of introducing direct-acting anticoagulants (heparins or fondaparinux). When an international normalized ratio (INR) level of 2-3 is reached and maintained at this level for at least 2 days, direct anticoagulants are discontinued (but not earlier than 5 days from the start of their use). The initial dose of warfarin is 5 or 7.5 mg once a day. For patients under 60 years of age and without serious concomitant pathology, an initial dose of 10 mg is acceptable. Warfarin is continued for at least 3 months[20].
Reperfusion therapy
The goal of reperfusion therapy is to remove the clot and restore normal pulmonary blood flow. Most often, thrombolytic therapy is used for this. It is recommended for high-risk patients. Some authors allow the use of thrombolysis for moderate risk, but the benefit of such therapy in this group of patients is currently unclear[21]. The following drugs are used:
- Streptokinase - loading dose of 250,000 IU over 30 minutes, then 100,000 IU per hour for 12-24 hours or accelerated regimen 1.5 million IU over 2 hours
- Urokinase - loading dose of 4400 IU/kg body weight for 10 minutes, then 4400 IU/kg body weight per hour for 12-24 hours or an accelerated regimen of 3 million IU for 2 hours
- Alteplase - 100 mg over 2 hours or accelerated regimen 0.6 mg/kg body weight over 15 minutes (maximum dose 50 mg)
Bleeding is the main problem of thrombolytic therapy. Massive bleeding develops in 13% of cases, and intracerebral hemorrhage occurs in 1.8% of cases.
Surgical methods
Kava filter.
Surgical removal of the blood clot (thrombectomy) is considered an alternative treatment for high-risk pulmonary embolism when thrombolytic therapy is contraindicated. In patients with a high risk of relapse and with absolute contraindications to anticoagulant therapy, vena cava filters can be installed[22]. They are mesh filters that catch blood clots coming off the wall and prevent them from entering the pulmonary artery. The vena cava filter is inserted percutaneously, usually through the internal jugular or femoral vein, and placed below the renal veins (higher in the presence of blood clots in the renal veins)[20].
Treatment of pulmonary embolism
- In the acute period of pulmonary embolism, strict bed rest is prescribed;
- To relieve pain during thromboembolism, narcotic analgesics are administered intravenously. The drug of choice is morphine;
- Inhalation of an oxygen-air mixture, according to indications, transition to mechanical ventilation;
- Heparin intravenously to prevent further thrombus formation;
- Eufillin for bronchospastic syndrome;
- For arterial hypotension - infusion of dopamine, with little effectiveness, simultaneously with norepinephrine;
- Thrombolytic therapy
- Embolectomy is indicated for patients with pulmonary embolism: 1) in need of cardiopulmonary resuscitation, 2) in the presence of contraindications to thrombolysis or its ineffectiveness, 3) patent foramen ovale and intracardiac thrombosis
- Treatment of complications, prevention of rethrombosis
Notes
- Geerts WH, Code KI, Jay RM, Chen E, Szalai JP (December 1994). "A prospective study of venous thromboembolism after major trauma." N.Engl. J. Med. 331
(24):1601–6. DOI:10.1056/NEJM199412153312401. PMID 7969340. Retrieved 2011-09-19. - A.I.Kirienko, A.A.Matyushenko, V.V.Andriyashkin, D.A.Churikov.
Thromboembolism of the pulmonary arteries: diagnosis, treatment and prevention (Russian) (14-06-2006). Archived March 19, 2012. - White RH (June 2003). "The epidemiology of venous thromboembolism". Circulation 107
(23 Suppl 1):I4–8. DOI:10.1161/01.CIR.0000078468.11849.66. PMID 12814979. Retrieved 2011-09-19. - Horlander KT, Mannino DM, Leeper KV (July 2003). "Pulmonary embolism mortality in the United States, 1979-1998: an analysis using multiple-cause mortality data." Arch. Intern. Med. 163
(14):1711–7. DOI:10.1001/archinte.163.14.1711. PMID 12885687. Retrieved 2011-09-19. - Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ (March 1998). "Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study." Arch. Intern. Med. 158
(6):585–93. PMID 9521222. Retrieved 2011-09-19. - ↑ 1 2 3 4
Torbicki A, Perrier A, Konstantinides S,
et al.
(September 2008).
"Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". Eur. Heart J 29
(18):2276–315. DOI:10.1093/eurheartj/ehn310. PMID 18757870. Retrieved 2011-09-15. - Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, Kovacs MJ (2001). "Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer." Ann Intern Med 135
(2):98–107. PMID 11453709. - Le Gal G, Righini M, Roy PM, et al.
(February 2006).
“Prediction of pulmonary embolism in the emergency department: the revised Geneva score.” Annals of Internal Medicine 144
(3):165–71. PMID 16461960. - ↑ 1 2 3 A. Kartasheva.
Pulmonary embolism. New ESC recommendations (2008) // Medicine Review. - T. 4, issue. 04. - pp. 56-64. - Schrecengost JE, LeGallo RD, Boyd JC, et al.
(September 2003).
"Comparison of diagnostic accuracies in outpatients and hospitalized patients of D-dimer testing for the evaluation of suspected pulmonary embolism." Clin. Chem. 49
(9):1483–90. DOI:10.1373/49.9.1483. PMID 12928229. - ↑ 1 2 V.S.
Savelyev, E.I. Chazov, E.I. Gusev et al. Russian clinical guidelines for the diagnosis, treatment and prevention of venous thromboembolic complications (Russian). - Moscow: Media Sphere, 2010. - T. 4, issue. 2. - pp. 1-37. - ISSN 1997-697. - Rodger M, Makropoulos D, Turek M, et al.
(October 2000).
"Diagnostic value of the electrocardiogram in suspected pulmonary embolism." Am. J. Cardiol. 86
(7):807–9, A10. DOI:10.1016/S0002-9149(00)01090-0. PMID 11018210. - Scott RC (July 1971). "The S1Q3 (McGinn-White) pattern in acute cor pulmonale: a form of transient left posterior hemiblock?". Am. Heart J 82
(1):135–7. PMID 5581712. - McGinn S, White P D (1935). "Acute cor pulmonale resulting from pulmonary embolism." J Am Med Assoc 104
:1473–80. - A. V. Strutynsky.
Electrocardiogram. Analysis and interpretation. - M: MEDpress-inform, 2009. - P. 120-123. — 224 p. — 10,000 copies. — ISBN 5-98322-542-1. - Come PC (April 1992). "Echocardiographic evaluation of pulmonary embolism and its response to therapeutic interventions." Chest 101
(4 Suppl):151S–162S. PMID 1555480. - Schaefer-Prokop C, Prokop M (November 2005). "MDCT for the diagnosis of acute pulmonary embolism." Eur Radiol 15 Suppl 4
:D37–41. PMID 16479644. Retrieved 2011-09-17. - Raschke RA, Gollihare B, Peirce JC (1996). "The effectiveness of implementing the weight-based heparin nomogram as a practice guideline." Arch. Intern. Med. 156
(15):1645–9. PMID 8694662. Retrieved 2011-09-18. - Erkens P. M., Prins M. H. (2010). "Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism." Cochrane Database Syst Rev
(9): CD001100. DOI:10.1002/14651858.CD001100.pub3. PMID 20824828. Retrieved 2011-09-18. - ↑ 1 2 Paul L. Marino.
Intensive therapy. - Moscow: GEOTAR-Media, 2010. - 770 p. — ISBN 978-5-9704-1399-9. - Dong BR, Hao Q, Yue J, Wu T, Liu GJ (2009). "Thrombolytic therapy for pulmonary embolism." Cochrane Database Syst Rev
(3): CD004437. DOI:10.1002/14651858.CD004437.pub3. PMID 19588357. Retrieved 2011-09-18. - Decousus H, Leizorovicz A, Parent F, et al.
(February 1998).
“A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group.” N.Engl. J. Med. 338
(7):409–15. DOI:10.1056/NEJM199802123380701. PMID 9459643. Retrieved 2011-09-18.
Conservative treatment
In the vast majority of cases, complete treatment of thromboembolism can only be carried out in a hospital hospital. In some cases, when a patient has prerequisites for the development of pulmonary embolism, and others suspect it, or emergency doctors believe that it is this pathology that provokes the existing signs of the disease, adequate emergency care can be provided.
The patient is freed from tight clothing and placed on a flat surface. To stabilize the condition, a large dose of a drug such as Heparin is usually injected into a vein, which promotes rapid resolution of the blood clot. If a clot completely blocks blood flow, administration of this drug may lead to partial resolution of the clot, allowing blood flow to be at least partially restored in the pulmonary arteries. Next, Eufilin, diluted in Reopoliglucin, is injected drip-wise. In the presence of severe manifestations of arterial hypertension, Reopoliglucin can be administered intravenously by emergency physicians.
As part of first aid, doctors who arrive on call can carry out therapy aimed at reducing the manifestations of respiratory failure. Complex drug treatment can be prescribed only after a comprehensive diagnosis in a hospital setting. If the medical staff suspected thromboembolism in a patient upon arrival to the call, and the necessary assistance was provided, the patient’s chances of survival increase significantly. After diagnosis, adequate drug treatment for pulmonary embolism can be prescribed. Complex conservative therapy should be aimed at:
- stopping further thrombus formation;
- ensuring the resorption of blood clots;
- compensation for manifestations of pulmonary insufficiency;
- compensation for heart failure;
- treatment of pulmonary infarction and other complications;
- desensitization;
- anesthesia;
- elimination of other complications.
To carry out targeted treatment of pulmonary embolism, it is necessary to provide the patient with complete rest; he should take a supine position on the bed with the head of the bed raised. Next, thrombolytic and anticoagulation therapy is carried out. The patient is prescribed drugs that have a thrombolytic effect, including Avelysin, Streptase and Streptodecase. These drugs help dissolve the blood clot. Typically, these drugs are injected into the subclavian vein or one of the peripheral veins of the upper extremities. If thrombosis is extensive, these drugs may be injected directly into the blocked pulmonary artery. In this case, intravenous administration of Heparin and Prednisolone, 0.9% sodium chloride solution and 1% nitroglycerin solution is indicated.
Solutions are administered using droppers. During the first 2 days from the moment of blockage of blood flow in the lungs, large doses of these drugs are prescribed, after which the patient can be transferred to maintenance doses. On the last day of intensive care, indirect anticoagulants are prescribed, for example, Warfarin or Pelentat. In the future, treatment with indirect anticoagulants can continue for quite a long time. For severe chest pain, drugs belonging to the group of antispasmodics and analgesics are usually prescribed. Oxygen inhalations are required to compensate for respiratory failure. In some cases, it is necessary to connect the patient to a ventilator.
If signs of cardiac weakness are detected, cardiac glycosides can be used. The entire range of measures indicated for acute vascular insufficiency can be carried out. In order to reduce the immunological reaction, strong antihistamines are prescribed, for example, Diphenhydramine, Suprastin, Pipolfen, etc. If there are additional disorders, the use of additional medications may be indicated to effectively relieve them.
Development mechanism
As stated, the immediate cause of pulmonary embolism is blockage of the pulmonary artery by a foreign structure. There are options here. The most common occurrence is thrombi (blood clots).
Similar formations form in the upper, lower extremities, and the heart itself (somewhat less frequently). They are not always rigidly attached to the place of their formation.
When exposed to a negative factor: pressure, impact, the clot can break off and move along the bloodstream. Further, everything depends on its size and the will of chance.
The thrombus will stop in one or another part of the vascular network, it is likely that it will be in the pulmonary artery.
The following is a standard scheme. A mechanical obstacle is formed to the flow of blood in a small circle.
Initially, it is poor in oxygen (venous), and is not sufficiently saturated with O2, which means the same meager amount enters the heart, is released into the aorta and circulates throughout the body.
For obvious reasons, such blood cannot meet the oxygen needs of cells. Therefore, severe starvation occurs against the background of cellular respiration disorder.
In the short term, this leads to cerebral ischemia and multiple organ failure. Death may occur within a matter of days. If a total blockage of the pulmonary artery occurs, death occurs almost instantly.
Causes
Pulmonary embolism is a multifactorial condition. There are a huge number of development factors: from excess body weight and excess cholesterol in the body (although PE is not a form of atherosclerosis, the connection is indirect), to pathologies of the cardiovascular system.
The most common reasons are:
- Arterial hypertension. It can provoke rupture of the vessel and the formation of a blood clot. And then its movement throughout the body.
- Heart attack and stroke (hemorrhagic type) create colossal risks.
- Injuries, large hematomas. The probability is small, but it is there. Especially if the rheological properties of the blood are impaired.
- Excessive thickness of liquid connective tissue.
Increase the likelihood of the process by being over 55 years old, being male, having an addiction to smoking, alcohol, drugs, and uncontrolled use of drugs of various groups (oral contraceptives and anti-inflammatory drugs are especially dangerous).
Lack of sleep and poor diet take their toll. Family history and a tendency to hematological diseases (changes in blood properties) play a certain role.
Symptoms of thromboembolism
Depending on what disease caused PE, the signs of pathology development also depend. Experts usually include the following as the main symptoms of pulmonary embolism:
- a sharp decrease in blood pressure;
- severe shortness of breath;
- against the background of shortness of breath, tachycardia develops;
- arrhythmia;
- blueness of the skin, cyanosis appears due to insufficient oxygen supply;
- localization of pain in the chest area;
- disruptions in the gastrointestinal tract;
- “tense stomach”;
- sudden swelling of the neck veins;
- interruptions in heart function.
To provide emergency care for pulmonary thromboembolism, it is necessary to carefully understand the specific symptoms of the pathology; they are not necessary. The indicated signs of pulmonary embolism include the following symptoms, but they may not appear at all:
- hemoptysis;
- feverish condition;
- accumulation of fluid in the chest area;
- fainting;
- vomit;
- less often comatose states.
With repeated blockage of the pulmonary arteries, the pathology becomes chronic; at this stage of pulmonary embolism, the symptoms are characterized by:
- constant lack of air, severe shortness of breath;
- skin cyanosis;
- obsessive cough;
- pain in the sternum.
How to quickly diagnose a disease
It is important to quickly determine what happened to the person and what kind of help he needs. PE, or pulmonary embolism, does not always manifest itself in the same way. Signs depend on the type of disease. With a massive embolus (thrombus), a person almost immediately loses consciousness, because he is critically short of air. But with a small blockage - a non-massive form of the disease - the patient will only hear strange noises when auscultating (listening) with a stethoscope; bluish-tinged skin. But he can live for several more years.
Only doctors can determine a 100% diagnosis upon arrival to the patient. But some special symptoms will help you draw the right conclusions and provide all possible assistance:
- The person begins to cough up blood.
- Complains of severe chest pain.
- He cannot stand on his feet and feels weak.
- Tachycardia.
- Skin cyanosis.
- In some severe cases, he falls into a coma.
- Another characteristic sign is severe shortness of breath.
In more than 85% of cases, the embolus forms in the veins of the lower extremities, and through the inferior vena cava enters the right atrium, from there into the right ventricle and directly into the lungs. A thrombus that blocks one of the main branches of the pulmonary trunk triggers a series of automatic reactions.
There is not enough oxygen, the tissues starve, and life-threatening heart failure begins. Therefore, blood clots formed in large veins are more dangerous than those in small vessels.
Air bubble blockage
In addition to blood clots, an air bubble may enter the bloodstream. This rarely happens spontaneously. Much more often as a result of medical intervention.
Contrary to popular misconception, a dropper after the medicine has been poured out is not capable of causing air to enter the bloodstream due to a difference in blood pressure and indicator in the system.
That is why special stands are used and glass containers with medicine are placed high.
Moreover, for the development of an embolism, at least 5 cubic meters of gas or more are required. This amount can only penetrate during open surgery or arterial catheterization. This option is much less common.
Then everything develops along an identical path. Blockage, disruption of cellular respiration, possible death of the patient without high-quality and urgent treatment. In some cases, it is impossible to radically influence the situation at all.
Causes of thromboembolism
As we have already said, everything that “can fly” to the right heart concerns the veins and the venous part of the systemic circulation. Therefore, the causes of pulmonary embolism, which most often lead to clinically significant manifestations, are the following:
- Thrombosis of deep-lying veins on the thigh and in higher sections, that is, large veins of the legs and pelvis;
- Thrombosis of deep veins located on the lower leg (with complicated thrombophlebitis varicose veins)
The degrees of risk are not comparable: 50% of all high thromboses are complicated by pulmonary embolism, and with thrombosis of the veins of the legs, only 1-5% of all cases lead to pulmonary embolism. If you combine the indicators, it turns out that in 70% of patients with pulmonary embolism, the source of blood clots is the venous vessels of the legs.
However, there is a whole list of diseases that lead to a sharp increase in the chances of pulmonary embolism. These include:
- various tumors and malignant neoplasms;
- severe cardiac pathology: congestive failure, heart attack, stroke;
- sepsis (purulent emboli in the veins);
- erythremia (Vaquez disease) - with it the blood thickens very much;
- nephrotic syndrome;
- systemic lupus erythematosus;
In addition, older age, taking oral estrogens in women, and prolonged immobility (for example, while in intensive care) increase the risk.
It is possible to list the variants of pulmonary embolism in which there is no separation and blockage by a thrombus. These options include air embolism. An air bubble can enter the pulmonary artery even with intensive rinsing of the sinuses. Also, during childbirth, amniotic fluid can enter the pulmonary veins through the uteroplacental sinuses, and this complication has a very high mortality rate.
There are variants of fatty, traumatic and septic embolism, consisting of bacteria and purulent tissue.
Prevention
There are no specific measures. It is enough to adhere to the rules of common sense.
- Stop smoking. Alcohol and drugs. Also, do not take any medications unless prescribed by a specialist. They can affect blood clotting and fluidity.
- Avoid serious injury. Hematomas require mandatory treatment.
- If you have somatic diseases, especially those affecting the rheological properties of liquid connective tissue, consult a doctor to prescribe treatment.
- Drink enough water per day: at least 1.5 liters. In the absence of contraindications - 1.8-2. This is not a hard indicator. It is important to base your weight on your body weight.
- Maintain an optimal level of physical activity. Walk in the fresh air for at least 1-2 hours.
Pulmonary embolism is a fatal condition in many cases. It requires urgent diagnosis and prompt treatment. Otherwise the consequences will be disastrous.
Acute disturbances of normal blood flow at a general, generalized level occur in cardiological practice in 10-15% of cases of all dangerous processes.
Depending on the severity of the disorder, the patient's risk of death differs. A prognosis can only be given after assessment and diagnosis, sometimes later, after the completion of primary therapeutic measures.
Pulmonary embolism is an acute disturbance of blood flow, the movement of liquid connective tissue from the heart into the pulmonary circle to enrich it with oxygen and further release into the aorta.
Deviation from the norm provokes catastrophic consequences.
The immediate cause of the pathological process is blockage of the pulmonary artery by some object. This is a blood clot (in the vast majority of cases), an air bubble (usually as a result of unsuccessful iatrogenic medical intervention).
Independent regression of the condition is impossible. In case of incomplete blockage, a general disturbance of hemodynamics (blood flow) and acute problems with cardiac activity are noted.
Hypoxia of all structures is detected (oxygen starvation), which in the short term leads to the death of the patient. Complete blockage results in rapid death within a few seconds.
Symptoms are nonspecific. Diagnosis is not very difficult if you know what to look for and where to look. Urgent therapy, in a hospital setting.