Positive and negative sides
The medicine is available in doses. Babies up to eighteen months are given an injection in one of the thighs, and older ones - in the shoulder. After vaccination, five percent experience a local reaction to the injection in the form of redness, but this is not considered a complication.
Four percent of those vaccinated experience minor side effects, such as fever, which persist for two days after vaccination. In response to the introduction of this virus, blood antibodies appear in the baby’s body, which are unable to synthesize cells that kill viruses with the underlying pathogen.
This is a very big disadvantage of the inactivated vaccine. There are no contraindications for IPV, and it is vaccinated even in children with immunodeficiency. Sometimes allergic reactions can be complications of IPV.
Unvaccinated people suffering from immunodeficiency become infected and become ill from people who have long been vaccinated.
It is very dangerous when people with AIDS become infected with this infection.
Healthy people do not have to observe quarantine after vaccination; you can walk with your baby as usual.
When a baby is vaccinated against polio, the consequences should not pose any danger to his health if it is done correctly. It helps the still weak child’s body fight a serious illness. It will forever save the child from the disease, and the parents from the fears brought by the infection.
Poliomyelitis is a dangerous viral disease that leads to disability. There is no cure for this disease, and treatment does not produce results. Diagnosis of the disease is difficult at the initial stage, until the virus has penetrated the spinal cord. The incubation period lasts 10/30 days, and during this period the carrier of the virus can infect other people. The infection is transmitted through contact (objects) and airborne droplets (during communication). The only salvation from poliovirus is vaccination. Parents are concerned about the reaction to the polio vaccine, however, complications after the disease are much more dangerous than the side effects from the vaccine.
Complications after polio vaccination: list
Poliomyelitis is one of the most dangerous childhood diseases, for which sufficiently effective drugs have not yet been invented. The virus lives in the intestines and throat of the child, and is transmitted by airborne droplets and contact, through household items or excretions. Sometimes infection occurs when swimming in a pool or pond.
From the intestines or nasopharynx, the infection enters the bloodstream, then into the nerve cells of the brain and spinal cord, which can cause paralysis. The disease is caused by three types of viruses, and the pathogen in the external environment can be viable for up to six months. According to statistics, children under ten years of age most often suffer from polio, and the peak of susceptibility occurs at the age of three.
What is the danger
When the virus enters the central nervous system, damage to the spinal cord and brain begins. This can cause paralysis, deformities and atrophy of the limbs. At the initial stage of polio, the patient begins to have fever, headaches, intestinal disorders and convulsions.
If the child is not vaccinated, the first stage passes into the second. The above symptoms disappear, but paralysis of the deltoid muscle, lower extremities, torso, and neck occurs. Due to paralysis of the respiratory muscles, death is possible in 15% of cases. However, even with recovery, children may remain disabled. The virus is dangerous because it is resistant to external influences and is volatile. Half a century ago, the spread of the polio epidemic was overcome only by mass vaccination of children.
Video “Complications after polio”
Adverse reactions
The polio vaccine contains a highly weakened or killed virus. When it enters the body, the pathogen multiplies, causing the production of antibodies. After some time after vaccination, the virus is eliminated from the body, but immunity remains.
Currently, two types of vaccines are used: live and inactivated. Live is administered to the child through the mouth, non-live - in the form of injections. Both drugs contain all three types of virus, so immunity to polio will be complete. 95% of children will have immunity after the first injection, the rest receive repeat injections.
Depending on the type of vaccine and the health of the child, adverse reactions may vary. When using an inactivated vaccine, there may be increased excitability, an increase in temperature up to 38 degrees, and slight swelling at the injection site. These symptoms usually go away within a couple of days.
When a live vaccine is administered, the normal side effects are:
- mild allergies;
- nausea and immediate vomiting;
- mild intestinal upset;
- general weakness.
Please note that vaccinations have their own schedule and contraindications. Most often, side effects occur if this is not taken into account. For example, vaccination should not be carried out in case of weakened immunity, inflammatory and infectious diseases, or immediately after recovery.
Complications
The only serious complication after vaccination is the so-called vaccine-associated polio (VAP). It develops only with the introduction of an oral vaccine, which is dripped into the mouth. The virus is activated, multiplies in the intestines, “turns on” the immune system, which then neutralizes it.
However, some children may have an immunodeficiency that has not manifested itself in any way. In this case, the virus is able to reach the nervous system and cause paralysis and other complications. Note that childhood immunodeficiency is extremely rare, so the risk of complications is minimal.
In the second case, the weakened virus in the child’s body mutates and becomes aggressive towards the body. Paralysis does not occur in everyone, only 10% of children in this case.
VAP appears 5 days later, but not later than a month after vaccination. First, the temperature rises, muscle tone increases, and the sensitivity of the limbs does not suffer. To prove the presence of a complication and begin treatment, it is necessary to compare the baby’s virus with the vaccine virus. Considering that, according to statistics, VAP occurs in only one in 500,000 children, and those who are not vaccinated can develop a much more severe form of polio, parents should not refuse vaccinations.
Video “Myths about vaccination”
From this video you will learn what complications may arise when using the polio vaccine.
LechimDetok.ru
Types of polio vaccinations
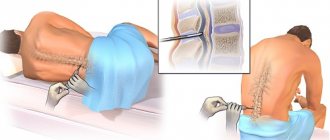
The polio vaccine was invented only in the middle of the last century by American scientists. The drug consisted of inactivated (killed) strains of a dangerous virus. Universal immunization helped to get rid of outbreaks of contagious infections that maimed people and claimed hundreds of lives. Later they invented a drug with live polio virus, which is produced in drops. The inactivated vaccine is given from a muscle in the body by injection, while the live vaccine is dropped into the child's mouth.
What is better - drops or injection? At three months, the child is given an inactivated strain by injection; at six months and beyond, drops are given instead of an injection. A live vaccine is considered more effective than an inactivated one. The vaccine is given together with DTP on the same day. No pronounced side effects have been recorded if all immunization rules are followed.
The disadvantage of a live vaccine is the difficult storage conditions of the drug, if these conditions are violated, the bacterial strain dies. There are also certain difficulties with dosage, since babies can regurgitate the drug injected into the tongue. The advantage of live vaccination is (contrary to existing legends about the danger of infection) passive immunization of persons in contact with the vaccinated child.
Important! Only a person with a pronounced immunodeficiency can become infected from a vaccinated child; others receive passive immunity to the virus.
Imported polio vaccines: drug names
Inactivated vaccines used in our country are produced abroad, among them there are single-component ones:
- Poliorix . It contains all three types of poliovirus, producing a strong immune response to them. The vaccine is in sealed vials (ampoules) and looks like a colorless suspension. It is given to children over three months old. A combination of this drug with OPV is allowed, with the first 2-3 vaccinations given intramuscularly, and then OPV drops are used;
- Imovax Polio . This clear liquid suspension also contains all three types of poliovirus. Contained in a disposable syringe (ampoule) with a dosage of 0.5 ml. The drug is combined with other vaccinations except BCG. It should be stored exclusively at a temperature of +2 - +7 degrees, and cannot be frozen.
There are also combination drugs indicated for the prevention of several infections (prevention of tetanus, whooping cough, diphtheria, hepatitis B, Haemophilus influenzae infection), including polio:
- Infanrix Penta;
- Infanrix Hexa;
- Pentaxim;
- Tetraxim.
You can purchase any type of vaccine yourself at a pharmacy with a prescription from a pediatrician.
Complications and side effects
What can happen to a child after vaccination? Parents should know that compliance with all points of immunization rules reduces the risk of complications to a minimum. In many children, post-vaccination symptoms are not expressed at all. A slight malaise and whims at a temperature of 37C are not considered dangerous complications.
Why then do they talk about a strong reaction to the polio vaccine? An extreme form of complications is the development of vaccine-associated poliomyelitis, which occurs with severe immunodeficiency of the child, with diseases of a neurological nature or severe dysbacteriosis. In other cases, reactions to the polio vaccine are expressed in:
- slight increase in temperature;
- anxiety and tearfulness;
- stool disorder;
- refusal to eat.
The listed reactions to the polio vaccine are not considered serious complications and do not require treatment. After the injection, local complications may occur in the form of swelling of the puncture site and slight redness. Sometimes itching and pain occur when touching the injection site. However, if there is no suppuration of the wound and the temperature does not rise (signs of an abscess), you should not worry.
Important! Serious complications after the polio vaccine can be allergic reactions to the antimicrobial components of the drug. In this case, revaccination is contraindicated.
Preparing for immunization
The basic rule of immunization is the complete health of the child. If your baby suffered an infectious disease on the eve of scheduled vaccination, it is necessary to strengthen his immunity before vaccination.
It is advisable to take tests (blood/urine) before vaccination to be sure of the baby’s complete health. Pediatricians rarely offer tests before vaccination, but parents can insist on this.
Before going to the clinic, do not feed your child tightly so that the body has the strength to adapt to the administered vaccine. It is also undesirable to feed your baby for at least an hour after vaccination.
If you are worried about an allergic reaction to the drug, give your baby an antihistamine three days before the injection (on the advice of your pediatrician). This will reduce the risk of allergies. Antihistamines are also given for three days after immunization.
Myths and legends
Young parents should know that it is impossible to get polio after vaccination against this virus. If you examine your baby before vaccination and talk about his condition with a pediatrician, there will be no complications. Also, people around the child will not get polio if they do not suffer from severe immunodeficiency and neurological disorders.
Is it possible to bathe the baby after vaccination, and will there be any complications? If the child does not have a sharp rise in temperature and does not show cold symptoms, bathing is allowed. If the injection site is inflamed, lubricate it with iodine mesh or troxevasin ointment, and do not rub with a sponge while bathing. There are no special contraindications to swimming, and there will be no complications after it.
A serious obstacle to immunization against polio is severe intestinal dysbiosis. The virus develops and multiplies first in the larynx, then in the intestines, from where it enters the spinal cord. Therefore, the intestines must be populated with healthy microflora before vaccination. Be sure to take this into account!
Important! A healthy baby with normal weight and no neurological diseases does not have dangerous complications due to polio vaccination.
Vaccination will protect your child from polio.
Parents are tormented by doubts about whether there is a need to vaccinate their children. Let's consider whether vaccination against polio is really necessary, the complications after which are seriously frightening.
It is quite difficult to make the right choice between the two extremes. On the one hand, there is fear of the disease, and on the other, of possible complications after vaccination.
Contraindications to polio vaccination
Before vaccination, it is necessary to find out whether the child has any contraindications. This is especially true for drip vaccination. Children cannot be vaccinated if the following conditions exist:
1) immunodeficiency of any kind;
2) any neurological abnormalities, including those that occurred after the first vaccination;
3) taking medications that artificially enhance immunity - often such drugs are prescribed for organ transplantation;
4) taking antibiotics.
The inactivated polio vaccine is less reactive. Contraindications for injection:
1) pronounced manifestations of allergies;
2) negative reaction after the first vaccination;
3) pregnancy;
4) oncological tumors and polyps;
5) condylomas;
6) drug or surgical therapy for cervical erosion.
Any chronic diseases should be under close medical supervision. Children and adults with bronchial asthma, diseases of the nervous system, and gastrointestinal tract react especially hard to vaccination. As a rule, in these cases, doctors prohibit vaccination. Children and adults who are currently undergoing treatment with any medications are not subject to vaccinations.
General information about polio
Poliomyelitis is a complex disease that is infectious, affecting the mucous membranes and neurons responsible for movement. As a result of the disease, the human body may suffer from paresis and paralysis. The main method of combating enterovirus infection is preventive vaccination against polio. The vaccine, like many others, can cause complications.
At the moment, doctors use two types of vaccines:
- oral (OPV), which is drops;
- inactivated (IPV).
The oral vaccine is the most effective and promotes the active development of immunity in the digestive system.
The inactivated vaccine is slightly weaker and is not fraught with complications, since it does not contain live viruses of the disease.
Live vaccines most often cause complications. The oral vaccine is a sweet-tasting, colored liquid that is dropped into the child's mouth on the tip of the tongue. If the child vomits, the procedure is repeated. The child should not drink or eat for an hour. It is the oral vaccine that contains live but weakened viruses.
After vaccination, it is necessary to ensure that the child does not have an immunodeficiency and does not have contact with persons with such indications. Another important feature of the child’s health after vaccination is complications of a neurological nature after the first polio vaccination.
Return to contents
Poliomyelitis: vaccination, vaccination schedule
Modern immunology uses 2 types of vaccinations: oral (drops) and inactivated vaccine. The first type was developed by the American virologist A.B. Sabin. The vaccine is called “live” because it contains a special weakened poliovirus. These are reddish drops that are administered through the mouth, trying to get to the root of the tongue closer to the tonsils. Absorbed through the lymph into the intestines, the vaccine helps the body's immune system create antibodies. The body reacts to a false virus as if it were a real disease, but more weakly. Experts say that polio drops are the best method of vaccinating children.
An inactivated version of the vaccine was developed by the American scientist J. Salk. It is administered by injection into the shoulder or thigh. The injection contains destroyed poliovirus. The contents of the vaccine enter directly into the blood. This does not create false strains. European doctors use both types of vaccines.
What is the danger?
Poliomyelitis is a very serious disease, the virus of which finds refuge in the intestines and throat of a person. Poliomyelitis viruses are transmitted through household items and mucous secretions and are dangerous because, entering the human body through the nasopharynx, they rush into the intestines, and from there through the blood vessels they reach the cells of the spinal cord and brain. When exposed to viral bacteria, the body can be paralyzed.
Initially, the virus can successfully disguise itself as an acute respiratory infection, and all mucous membranes in both the nasopharynx and intestines become inflamed. The incubation period for polio lasts 2 weeks, but sometimes it can last 1 month.
Doctors received a vaccine against this serious disease only in the early 20s. last century. Then American scientists found the possibility of using dead viruses to treat polio.
The disease can occur in three scenarios:
- The mild form of the disease is characterized by fever, runny nose, malaise, sore and red throat, loss of appetite and diarrhea; however, all the symptoms may be similar to an intestinal infection or acute respiratory infections.
- A complex form of poliomyelitis is accompanied by serous meningitis with damage to the cerebral cortex. Body temperature also rises, vomiting and headache appear. You can judge whether the brain is damaged by the tension in the neck muscles (you can check the patient’s condition by asking him to pull his chin to his chest).
- Paralysis is the most difficult consequence of the disease, which is accompanied by fever, cough, runny nose, pain in the intestines and stomach.
3 days after the disease, a person will experience pain in the back and limbs.
To make a diagnosis, symptoms alone will not be enough for doctors.
You will need to take mucous discharge from the throat, intestines and nose for analysis.
Return to contents
What is polio
Poliomyelitis is one of the most dangerous childhood diseases, for which sufficiently effective drugs have not yet been invented. The virus lives in the intestines and throat of the child, and is transmitted by airborne droplets and contact, through household items or excretions. Sometimes infection occurs when swimming in a pool or pond.
From the intestines or nasopharynx, the infection enters the bloodstream, then into the nerve cells of the brain and spinal cord, which can cause paralysis. The disease is caused by three types of viruses, and the pathogen in the external environment can be viable for up to six months. According to statistics, children under ten years of age most often suffer from polio, and the peak of susceptibility occurs at the age of three.
Polio vaccination: consequences
If the OPV vaccine was used, an allergic reaction or intestinal upset may occur.
The inactivated vaccine is administered intramuscularly or subcutaneously. Despite the fact that the vaccine does not contain live viruses, its use may also be prohibited if there are allergic reactions to various auxiliary components or antimicrobial drugs, such as polymyxin B, neomycin and streptomycin.
After vaccination against polio, local reactions in the form of swelling and redness of the injection site are possible. If the temperature rises, appetite decreases, and weakness appears, then such symptoms can be attributed to the consequences of vaccination against polio.
After taking an oral vaccine, there may be complications that cause arthritis. Sometimes children experience lameness for 2 days, but it also happens that it remains for life.
Side effects from polio vaccination may include pneumonia, lung problems, stomach ulcers, or gastrointestinal bleeding.
There is often no response to the polio vaccine. There are expected consequences that are not complications.
The consequence of using an oral vaccine may be a slight increase in temperature for several days. Also, stool disturbances may occur for 2 days.
After inactivated vaccination, in 7% of children the injection site swells and turns red. Most often, the reddened area does not exceed 8 cm in diameter. Fever appears infrequently in children, in about 4% of cases. This condition may last a couple of days.
The schedule for vaccinating children against polio will depend on the type of drug chosen. If an oral vaccine is used, then the timing of vaccination falls on 3, 4, 5, 6 months. Subsequently, repeated vaccination in this case occurs at 18, 20 months and at 14 years of age.
If vaccination is carried out with an inactivated vaccine, then this process is divided into 2 stages with an interval of 1.5 months. When 1 year has passed since the last vaccine, it is the turn of the first revaccination, and after 5 years it is necessary to carry out the second.
In general, side effects of drugs after vaccination can be divided into local and general. Local complications include intestinal dysfunction when using oral vaccination. But since intestinal dysfunction occurs quite often in children, it is difficult to determine that vaccination was the cause.
Common complications after vaccinations include allergic reactions that appear within the next 4 days after vaccination. To exclude the possibility of food allergies, after vaccination the baby should be fed regular food, without offering new products, without changing the milk formula, milk concentration, or introducing new complementary foods. These steps will help eliminate food allergies. A child may have a reaction to the antibiotic included in the domestically produced vaccine, kanamycin.
Good day, dear parents. In this article we will talk about how a child feels after a polio vaccination. You will learn what the body's reaction to the administered vaccine should be, as well as the possible consequences of this vaccination.
Polio vaccinations - consequences and precautions
04/02/2015 Poliomyelitis (infantile spinal paralysis) is a disease that affects children aged 5 months to 6 years.
A specific feature of this disease is that it is very contagious and the virus can exist in the external environment for almost 6 months. Transmission routes are airborne, through insects and dirty hands. In some cases, it is asymptomatic. However, the patient becomes a carrier of infection.
The polio virus penetrates through the blood into all organs and systems of a sick person. Polio affects the spinal cord and nerve cells. In the vast majority of cases, complications of the disease lead to the death of some nerve cells and paralysis of muscle groups.
In 1-5% of cases, paralytic poliomyelitis occurs. According to statistics, its main complication is residual paralysis with muscle atrophy. A third of patients experience complete recovery. Death accounts for approximately 10% of cases. Death occurs due to damage to the patient's respiratory system.
History of the development of polio in the world
This disease has become a real disaster for residents of Europe and North America. It was possible to curb its spread only after an effective vaccine was developed. This happened back in the 50s of the last century.
In the Soviet Union, no new cases of polio infection have been reported and no symptoms have been observed since 1961. However, in 2010, an outbreak of the disease broke out in Tajikistan. From there it came to Russia. Since before that time there were no cases of polio and children were vaccinated against this disease with an inactivated vaccine. It was administered to children at 1 year of age and again at 14 years of age.
The 2010 polio outbreak demonstrated its ineffectiveness against live virus. That is why, since 2011, an alternative has been adopted and children are vaccinated against this disease with the so-called live vaccine.
Two types of polio vaccine
Scientists have developed two types of vaccines:
- inactivated, which is administered intramuscularly and contains killed poliovirus;
- Oral polio vaccine is a “live” vaccine, it is administered in the form of drops through the mouth.
- pregnancy and its planning;
- lactation period;
- an atypical reaction to a previous vaccination;
- child's illness;
- allergy to the components of the vaccine included in its composition.
- difficulty breathing or shortness of breath;
- convulsions;
- itching;
- swelling of the face;
- difficulty swallowing;
- increase in body temperature above 39 degrees.
The oral polio vaccine is a clear liquid with a sweet taste. It is instilled into the mouth, at the root of the tongue.
The first three vaccinations for a child are given with an inactivated vaccine, and the last one with a live one. This schedule allows you to completely eliminate the risk of infection for babies, as they develop immunity against the live virus. This scheme is successfully used according to WHO recommendations in many countries around the world.
Live vaccine in drops has some disadvantages. Firstly, it has rather high requirements for storage conditions. Secondly, in practice, difficulties arise with the dosage of the composition and babies often spit up.
If adults travel to areas dangerous for polio, they are given a booster vaccination against polio.
Live vaccine (drops) is given to children from 2 months. The first vaccination is carried out at 3, 4, 5 and 6 months. Revaccination against polio is carried out at 18 and 20 months, as well as at 14 years.
Contraindications for vaccination
This polio vaccine has its contraindications, which can cause complications.
Thus, HIV-infected children, as well as those whose parents are HIV-infected, will not be vaccinated against polio. They are prohibited from contacting a vaccinated person for two weeks. This applies to the oral polio vaccine. This category of patients is given an inactivated vaccine. With its help, you can protect yourself from viruses that are spread by those vaccinated with a live vaccine.
Other contraindications include the following:
Reasons for vaccination
A child will be vaccinated against polio only after his parents or legal representatives provide their written consent. Medical workers provide them with detailed information about the reasons for vaccination, the consequences of refusing it and possible complications. In case of refusal, it is documented and signed by both the parents of the minor child (his legal representatives) and medical workers.
Let's consider the main objective reasons for vaccination against polio.
Firstly, timely vaccination is necessary to avoid the risk of contracting a serious illness that can lead to dangerous complications and even death. Despite the fact that Russia is recognized as a country free from wild poliovirus, its close proximity to countries such as Tajikistan, where the virus has not been completely eradicated, creates a certain danger.
Secondly, it is needed, because without this vaccination against polio, the child will not be accepted into kindergarten. Vaccination occurs according to the established schedule.
Thirdly, the decision whether to vaccinate a child or not is made by his parents. However, one should take into account the fact that a vaccinated baby will spread the live virus in the environment for 2-4 weeks. If parents refuse vaccination, the child may become infected through contact with such children.
Possible complications after vaccination
After vaccination, complications associated with the development of polio and arthritis may occur. Moreover, lameness can persist for several days, and can remain for life.
Oral polio vaccine (drops) can cause intestinal dysfunction. But, as practice shows, it passes without serious consequences for the child’s health. In addition, these complications are controversial, since they occur in young children even without vaccination against polio.
An inactivated vaccine is different in that it does not cause negative reactions in the intestines and does not affect its normal microflora.
Doctors warn parents about signs that require immediate medical attention:
Basic activities in preparation for vaccination
The main contraindication causing complications for vaccination against polio is the disease of the child. Only a healthy baby can tolerate it well. That is why, if in doubt, it is better to temporarily refuse vaccination.
Any vaccination is stressful for the body and has a strong effect on the immune system. If the body suffers from another illness, it will be very difficult for it to cope and the risk of side effects increases.
Doctors use preliminary blood and urine tests as a means of preparation. Based on the information received, the child’s condition is analyzed and a decision is made on vaccination in order to prevent complications and reactions.
In order to avoid the occurrence of allergic reactions 1-2 days before the child receives the vaccine, it is necessary to start giving him antihistamines.
If the baby has chronic diseases or suffers from allergies before vaccination, you should contact an immunologist who will prescribe additional tests. Based on them, a suitable polio vaccine will be selected, taking into account contraindications and possible reactions.
Ideally, a second consultation should be obtained after the child has been vaccinated. The doctor will prescribe diagnostics to detect antibodies in the body. The doctor’s supervision will ensure that the entire process goes through without complications and allows for timely identification of contraindications and negative reactions.
Precautions to prevent complications
Compliance with certain precautions is required before any vaccination in order to avoid complications and negative reactions, and this case is no exception.
- Firstly, before vaccination, the child should not be given new foods that may trigger symptoms of an allergic reaction.
- Secondly, your home medicine cabinet must contain anti-allergy and antipyretic drugs to neutralize complications and negative reactions.
- Thirdly, within an hour after taking the live vaccine (drops), you should not feed or water the baby, since the vaccine enters the stomach along with the food.
- Fourthly, after vaccination against polio, it is not recommended to kiss a child on the lips, and also to wash hands after washing the baby in order to prevent possible infection of parents and the occurrence of alarming symptoms.
Dangerous consequences of vaccination
The polio vaccine, the consequences of which in the vast majority of cases do not cause any serious complications, is not dangerous. Some reactions are normal but may cause concern for parents. These include the following symptoms:
These complications from droplets disappear two days after vaccination against polio. There is a common misconception that the injection site should not be wet. In fact, this cannot lead to serious negative consequences. At the same time, doctors recommend protecting the child’s strength after administering the vaccine composition.
Categories: For vaccination, polio, Against vaccination Tags: vaccine, vaccination, WHO, doctors, children, kindergarten, immunity, complications, refusal, polio, polio, vaccination, cancer, child, parents, Russia, symptoms, seizures No comments
Add a comment
Click to cancel reply.
Preparing for vaccination
In order for the baby’s body to respond normally to the vaccine, certain rules must be followed. The most important thing is the absolute health of the little one. In addition to the fact that the absence of illness at the moment is important, it is also unacceptable that the recovery process begins less than two weeks before the vaccination is scheduled. It is advisable that the child’s immunity is strengthened before vaccination.
- Before vaccination, it is important to undergo an examination by a pediatrician and undergo clinical urine and blood tests. It is worth knowing that pediatricians generally do not prescribe any tests. However, it is better to insist on their implementation.
- Make sure that the baby does not overeat the day before, or better yet, that he is hungry at the time the vaccination is administered and an hour after that.
- Pay great attention to drinking plenty of fluids.
- In order to reduce the risk of developing an allergic reaction, it is recommended to give your baby antihistamines three days before the planned vaccination. However, these medications should only be prescribed by a doctor; you should not self-medicate, as you may harm your child.
Consequences of introducing an inactivated vaccine:
- Heat.
- Severe rash on the surface of the body.
- Difficulty breathing.
- Swelling of the face and limbs.
Almost all of these symptoms indicate the presence of an allergic reaction to the administered drug. If your baby exhibits at least one of the above signs, you should immediately seek help from a doctor.
As for the oral vaccine, it causes side effects much more often, and these side effects are much more serious than with IPV. These include:
Starting from the fourth and ending with the thirteenth day after vaccination, the baby exhibits symptoms of polio: the temperature rises sharply, paralysis develops, and pain in the muscles and back begins. After the diagnosis is established, the child will be admitted to the infectious diseases hospital for inpatient treatment.
You need to know that even with the normal course of the post-vaccination period, certain changes in the child’s condition may be observed. Of course, it is advisable that the doctor warns in advance about possible manifestations.
The following reactions may occur after administration of the oral polio vaccine:
- Skin rashes that go away when taking antihistamines.
- Frequent diarrhea, especially in the first days.
- The temperature rise is not higher than 37.6 degrees. Can last up to 14 days. If the temperature rises above this indicator and accompanying symptoms appear, you should immediately consult a doctor. Such a process will no longer be considered normal.
- Skin hyperemia at the injection site.
- Induration and pain at the injection site.
- Decreased appetite, sleep disturbance.
- Almost imperceptible increase in temperature.
- Moodiness.
As you understand, reactions of this nature do not require any treatment. For allergic rashes, antihistamines may be prescribed. As for everything else, as a rule, all processes in the body are normalized without the intervention of medications.
Baby's reaction to polio vaccination
In the Russian Federation, a sequence of polio vaccinations has been approved, consisting of 2 stages - vaccination and revaccination. In the absence of serious illnesses in the child that give the right to a deferment from vaccination, the schedule is as follows:
- the first stage - at 3, 4.5 and 6 months;
- the second stage - at 1.5 years, 20 months and 14 years.
The schedule involves a combination of OPV and IPV. Pediatricians recommend intramuscular injections for infants, and drops for babies after one year of age. For older children, the polio vaccine is given in the shoulder.
If parents choose only IPV for their child, then it is enough to vaccinate 5 times. The last injection is given at 5 years of age. Missing a vaccine as scheduled does not mean you need to start the regimen all over again. It is enough to agree on the optimal time with the immunologist and carry out as many procedures as necessary.
which does not have
You need to know that even with the normal course of the post-vaccination period, certain changes in the child’s condition may be observed. Of course, it is advisable that the doctor warns in advance about possible manifestations.
The following reactions may occur after administration of the oral polio vaccine:
- Skin rashes that go away when taking antihistamines.
- Frequent diarrhea, especially in the first days.
- The temperature rise is not higher than 37.6 degrees. Can last up to 14 days. If the temperature rises above this indicator and accompanying symptoms appear, you should immediately consult a doctor. Such a process will no longer be considered normal.
If a baby is vaccinated with an inactivated polio vaccine, certain reactions are possible, but they occur in very rare cases:
- Skin hyperemia at the injection site.
- Induration and pain at the injection site.
- Decreased appetite, sleep disturbance.
- Almost imperceptible increase in temperature.
- Moodiness.
As you understand, reactions of this nature do not require any treatment. For allergic rashes, antihistamines may be prescribed. As for everything else, as a rule, all processes in the body are normalized without the intervention of medications.
Only a child after OPV can be infectious for 1 month. It is possible for unvaccinated children to contract polio when they come into contact with children recently vaccinated with OPV.
After vaccination with IPV, the child is not contagious.
Causes of complications
Consequences after polio vaccination are extremely rare. However, it is worth knowing for what reasons they may occur:
In addition, it is important to know which diseases are contraindications to vaccination, in particular oral vaccines:
- Immunodeficiency.
- Taking immunosuppressants.
- Neurological abnormalities.
- Taking antibiotics.
When taking inactivated vaccines, the contraindications are:
- Severe allergies.
- Oncological formations.
A reaction to the Sabin polio vaccine (weakened) develops as often as possible. The main problem is vaccine-associated polio, which becomes a source of paralysis.
Children are vaccinated for the first time every 3 months. If there are no complications, the second vaccination is given at 4.5 months, the next one at 6 months. Such dates are prescribed in the national calendar.
The reaction to vaccination is formed not only as a result of the entry of a live strain of poliovirus into a weakened body. There are more dangerous consequences that official medicine is silent about. More details about everything in the article.
Contraindications to the procedure
To prevent polio vaccination from causing complications, contraindications to vaccination should be taken into account in each specific case.
Vaccination against polio is strictly prohibited for a child if he has signs of any pathology, both infectious and somatic. In this case, it is necessary to postpone immunization until complete recovery occurs.
Also, immunization against polio is not given to those who have severe forms of immunodeficiency. If the pathology of the immune system is recognized by doctors as not severe or is in remission, then it is not considered a contraindication. In this case, an inactivated vaccine is used.
If a child has any type of allergy, a live vaccine is contraindicated for him, but he can be vaccinated with an inactivated drug, since it is not able to act as an allergen. Oral polio vaccines (OPV) containing live strains of the virus can cause an allergic reaction.
First of all, the baby should be examined by a pediatrician to identify possible contraindications. After the procedure, children are supervised by a medical professional for at least 30 minutes.
Signs of a severe post-vaccination complication appear already at this time. Parents of a vaccinated child are also warned about the possible consequences so that they can navigate and seek medical help in time if alarming symptoms appear at home.
Polio vaccine: consequences, reviews
Vaccine-associated reactions are divided into local and general.
Local reactions - redness, swelling, pain at the injection site of the inactivated Solka drug. The general consequences of the condition arise against the background of decreased immunity with an inadequate response to foreign viral antigens. The Sabin vaccine is more reactogenic. When introducing viruses weakened by formaldehyde, damage to nerve fibers and spinal ganglia is possible. This reaction occurs rarely, but the danger of the condition determines the parents’ refusal to vaccinate their child.
Young mothers are especially careful when it comes to vaccination; they carefully study parental reviews, information about the consequences, and complications.
Poliomyelitis is a deadly infection for which there is no cure. The only protection is vaccination. Unfortunately, reactions to the vaccine do happen. Humanity has been unsuccessfully fighting vaccine-associated polio for about 50 years. The complication occurs rarely, but is quite dangerous.
Poliomyelitis infection occurs through airborne droplets and contact. It is almost impossible to protect yourself from poliovirus.
Only 5% of people develop symptoms after infection. In 95% of those infected, even clinical signs of the disease are not observed. Scientists explain the situation by a genetic predisposition to the disease due to the special structure of the nervous tissue in certain people.
Statistics show that only 1% of people develop muscle paralysis and atrophy. The consequences of the condition are that the person remains disabled. Mortal danger is created by paralysis of the intercostal muscles. Blocked breathing leads to suffocation.
Reviews of vaccination from specialists indicate the preservation of immunoglobulins in the blood after vaccination for 10 years. This is the maximum period, so after the interval has expired, revaccination is carried out.
Papillomas on the neck, body, armpit and face: how to get rid
Cases of infection with a wild strain of the virus in a vaccinated person are milder, but paralysis and muscle paresis occur.
Negative reviews from people are based on descriptions of the side effects of vaccination. Vaccine-associated reactions, local and general consequences - all this occurs.
Before the mass distribution of Salk and Sabin vaccinations, the death of a large number of people was observed in Europe and America. Statistics have shown that the method has led to the elimination of the disease in many countries. The World Health Organization has even developed a program to eradicate the infection throughout the world. Experts were unable to eliminate the disease due to the constant mutation of the pathogen.
There is information about the emergence of a mutated strain of poliovirus in Japan, formed through the exchange of information between the types included in the vaccine.
The first stage is carried out at 3 months and is carried out due to the baby’s body’s instability to infection. By this time, maternal immunoglobulins obtained from milk are running out. In Asia, vaccination is carried out directly in the maternity ward.
Negative reviews and refusals from parents make it difficult to eradicate the infection everywhere. By infecting the body of an unvaccinated person, poliovirus gains the opportunity to reproduce in the human population.
Should I get vaccinated against polio?
It is a generally accepted fact that polio currently belongs to the category of rare infectious pathologies, but infectious disease specialists around the world are unanimous in the opinion that in the absence of adequate prevention, the disease is prone to rapid spread with the development of an epidemic course. In 2020, several cases of the disease were reported in European countries due to the fact that many parents formally refuse polio vaccination. In these situations, the disease proceeded in the form of flaccid paralysis lasting up to 60 days. All parents who refuse vaccination should take into account that complications after polio vaccination develop only in 5% of cases, and the consequences of the disease itself can be very serious, including death. Such a high percentage of deaths is due to the predominant spread of the bulbar form of the disease. Of course, polio convalescents develop lifelong, persistent immune mechanisms that prevent the possibility of developing a repeat episode of the disease.
Considering the fact that infectious disease specialists have not yet been able to develop an effective drug treatment regimen for this pathology, the only way to prevent serious consequences is vaccination against polio. Reviews from parents of children vaccinated against polio are usually positive.
The latest recommendations from experts state that a child should be vaccinated against polio in stages (at two months, at four months, at six months, at one and a half years, and then at six and fourteen years). Subject to compliance with this polio vaccination regimen, persistent lifelong immune mechanisms are formed in a child from an early age, which under no circumstances allow the development of a clinical picture of the disease.
Efficiency
There are no reliable scientific results that the effectiveness of the polio vaccine exceeds the side effects caused by the infection. In the United States, according to statistics, there is no disease, but there are no statistics on the consequences of vaccination. Vaccine-associated reactions pose a danger to human life if they occur as muscle paralysis.
The first results of reducing infection began to be seen after 1953, when the Salk vaccine appeared. Statistics indicated a decrease in the severity of the disease by approximately 47%. Then the statistics became even more positive. Reviews about vaccination were only positive, both among patients and doctors.
Why didn’t the program to mass eradicate the infection work? With the advent of high-resolution electron microscopy, specialists have the opportunity to study small viruses. After this, negative reviews about the disease appeared among scientists. Some European countries did not adopt a mass vaccination program after this, but statistics showed that the incidence of polio among residents also decreased.
The results reflect changes in approaches to counting the number of cases. Registration of paralytic forms has become less common due to new approaches to diagnosis. Poliomyelitis paralysis began to be considered a disease only after confirmation of the etiology by detection twice over a time interval.
What are the differences between the symptoms of tonsillitis, pharyngitis and laryngitis?
Facts confirm the small dependence of statistics on polio vaccination. It is impossible to estimate how serious a role vaccinations played in eliminating the disease.
Contraindications
Contraindications to the inactivated Salk vaccine:
- Neurological disorders on previous injection;
- Immunodeficiencies.
The contraindications described above are absolute. If a person has these conditions, administering the vaccine is prohibited.
Side effect:
- Allergic conditions;
- Dyspeptic disorders: abdominal pain, diarrhea, allergies.
Contraindications to the use of OPV:
1. Immunodeficiency states;
2. Neurological complications after previous vaccination.
Side effects of OPV vaccination include:
- Diarrhea;
- Allergy.
Inactivated polio vaccine is administered intramuscularly or subcutaneously. The drug does not contain live viruses, so it causes fewer complications.
Contraindications to IPV:
- Allergic reactions to the constituent components of the drug;
- Hypersensitivity to antimicrobial agents - polymyxin B, neomycin.
Consequences of vaccination with inactivated vaccine:
- Temperature increase;
- Decreased appetite;
- Malaise and weakness;
- Local reactions at the injection site.
According to the modern calendar, oral vaccination is carried out for a child at 3, 4, 6 months. Repeated revaccination is carried out at the age of 18-20 months.
Primary administration is divided into 2 stages with an interval of at least 1.5 months. Revaccination – after a year and 5 years.
The most dangerous complication of vaccination is vaccine-associated poliomyelitis, which develops during the first administration of the drug.
Children with congenital immunodeficiency virus and developmental anomalies are vaccinated only with an inactivated vaccine.
Dates according to the national calendar:
- First IPV vaccination – 3 months;
- Second – 4.5 months;
- Third IPV – 6 months;
- First OPV – 18 months;
- Second OPV – 20 months;
- Third OPV – 14 years.
Vaccination against polio is postponed if the immune system is impaired. A child with an immunodeficiency must be isolated from children who have been administered OPV for 2 weeks. Such preschoolers should not attend kindergarten during polio vaccination.
Polio vaccination - description, possible consequences, contraindications and reviews
Hello dear readers! Our children are our life and it is quite natural that we try in every possible way to protect them from any troubles. However, this is only possible when you know the enemy by sight, and even better, see him. It’s another matter if it sneaks up unnoticed and strikes instantly.
This is exactly what usually happens in the case of viral diseases. And if some of them are successfully treated, others can, at a minimum, leave you disabled, and, at maximum, take your life. These include polio. There is an opinion that the polio vaccine, reviews of which are striking in their contradictions every year, can save the situation. But is this really so? This is what we will talk about today.
Polio vaccination: what is it and why?
Poliomyelitis is a dangerous and incredibly contagious disease, the virus of which, penetrating the human body, multiplies in the throat and intestines.
Where does it come from? Most often, infection occurs through airborne droplets after contact with an infected person, especially if he coughs or sneezes, as well as through household items and water, where the pathogen can live for months.
The disease occurs all over the globe and, ironically, most often affects children aged 10 months to 5 years. But the most interesting thing is that at first the symptoms of polio are similar to the symptoms of a common acute respiratory infection and do not immediately attract the necessary attention.
Meanwhile, the virus itself does not sleep: from the intestines it penetrates the blood and nerve cells of the spinal cord, gradually destroying and killing them. If the number of affected cells reaches 25–30%, paresis, paralysis, and even atrophy of the limbs cannot be avoided. How else is this disease dangerous? Sometimes it can affect the respiratory center and respiratory muscles, causing suffocation and death.
In any case, today only pictures from the Internet tell about the consequences of polio. But all this is only due to the fact that in the 1950s two vaccines were created, which subsequently saved several continents from the disease. We are talking about OPV and IPV, which are also successfully used by modern medicine.
OPV vaccine against polio
OPV, or oral live vaccine, is the same red drops with a bitter taste that are administered by instillation through the mouth. Moreover, for babies they try to get to the root of the tongue, where there are no taste buds, in order to exclude the possibility of regurgitation, and for older children - to the palatine tonsil. They were created by medical scientist Albert Sabin in 1955.
The principle of the vaccine is simple: the strain of the virus enters the intestines, where it begins to multiply. The immune system immediately reacts to its presence, synthesizing antibodies that can subsequently fight real polio. However, this is not the only advantage of this vaccine. The fact is that children vaccinated with it release the weakened strain of the virus they introduced into the environment up to 2 months after vaccination. This happens when you sneeze or cough. And that, in turn, further spreads among other children, as if once again “vaccinating” them. And everything would be fine, but the consequences of OPV vaccination against polio are sometimes disastrous.
Consequences of introducing OPV into the body:
- an increase in temperature to 37.5 C, which may not be recorded immediately, but on days 5–14;
- changes in stool on days 1–2 (increased frequency or weakening);
- various allergic reactions;
- development of vaccine-associated polio.
If the first reactions to the polio vaccine are considered normal, then the last one is a real complication. The fact is that if the rules of vaccination are violated, the incoming virus provokes the development of ordinary polio, which can result in paralysis. The IPV vaccine is another matter.
IPV vaccine against polio
The inactivated vaccine was created by Jonas Salk in 1950. It is a drug that is injected into the body using a disposable syringe. Where is the polio vaccine given in this case? In the thigh or shoulder, the main thing is intramuscularly.
The advantage of this vaccine is its relative safety. The fact is that it contains a killed virus. Once in the body, it also forces the immune system to work, but since in this case no one is reproducing, there is no risk of developing vaccine-associated polio. And the reactions to its introduction are somewhat easier.
Consequences of introducing IPV into the body:
- redness and swelling at the injection site (no more than 8 cm in diameter);
- increase in temperature in the first two days;
- loss of appetite;
- irritability, anxiety;
- the development of an allergic reaction is already considered a complication.
When is the polio vaccine given?
It is worth noting that the use of both types of vaccines is officially permitted in Russia. Moreover, vaccination can be carried out according to several schemes, depending on the one chosen.
At what age is OPV or polio drops administered?
- At 3 months three times with an interval of 4 - 6 weeks;
- 18 months (revaccination);
- 20 months (revaccination);
- 14 years old.
According to the vaccination schedule, IPV is given to children aged:
- 3 months;
- 4.5 months;
- 6 months;
- 18 months (revaccination);
- 6 years (revaccination).
Meanwhile, at present, a mixed scheme is most often used, when both IPV and OPV are given to the same child. In this way, it is possible to minimize the occurrence of side effects associated with vaccination.
In this case, he receives a dose of the drug in:
- 3 months (IPV);
- 4.5 months (IPV);
- 6 months (OPV);
- 18 months (OPV, revaccination);
- 20 months (OPV, revaccination);
- 14 years old.
How is vaccination done if for some reason it was not possible to follow the schedule? Here everything is decided by a pediatrician or an immunoprophylaxis specialist. True, if at least one vaccination has been given, vaccination is not started all over again, but continued.
By the way, along with children, adults are also vaccinated, for example, if they plan to travel to countries where there are polio outbreaks.
Contraindications to polio vaccination
It is prohibited to administer live oral OPV vaccine to a child if:
- detection of malignant neoplasms (tumors);
- exacerbation of chronic diseases;
- the presence of acute diseases;
- immunodeficiencies (HIV, AIDS);
- neurological disorders;
- presence of developmental defects;
- the presence of serious diseases of internal organs, in particular the intestines.
Is it possible to get the polio vaccine if you have a runny nose? It all depends on its nature. However, as practice shows, it is not an absolute contraindication to vaccination.
A child should not be given IPV only if:
- if he is allergic to streptomycin, neomycin, polymyxin B;
- development of an allergic reaction to previous vaccinations;
- presence of neurological disorders.
Is it possible to get polio from a vaccinated child?
Unfortunately yes. However, this applies to completely unvaccinated children. That is why, in the case of collective vaccination with live vaccines (drops), those are sent to quarantine for 2 - 4 weeks.
Interestingly, there have been cases when a vaccinated older child infected a younger one, or worse, pregnant women picked up the virus. But in order to prevent this from happening, it is necessary to especially carefully observe the rules of personal hygiene - wash your hands more often, if possible, do not use shared household items (toys, potty, etc.)
We also suggest watching the video in order to finally decide whether to get vaccinated against polio. In it, Dr. Komarovsky touches on the issue of all enteroviruses, which include the causative agent of polio:
Reviews about the polio vaccine
Karina:
They vaccinated my daughter (drops), that’s all, everything is fine. True, she complained of pain in her tummy, and she had frequent bowel movements for a couple of days.
Inna:
I read bad reviews and wrote a refusal to take polio. Now it was done in the garden, and we were forbidden to visit it for 60 days so as not to get infected.
Larisa:
I vaccinated my son against polio. A couple of days later, ARVI symptoms began, they were treated, and then he began to limp on his leg. We went through an examination, the doctors said that everything was fine, and the son eventually went away. But I still have a biased attitude towards her.
What is the polio vaccine? For some, this is a huge risk that they consciously do not want to take. For others, it is the only opportunity to escape from a dangerous illness. However, when taking either side, it is important to weigh the pros and cons. After all, not only the health of the child, but also his life depends on your decision in this case.
Remember this! Share what you read on social networks! Subscribe to our updates! And be healthy! See you later!
2016-04-24
maminyzaboty.com
Unvaccinated children
With good immunity, the virus rarely causes polio paralysis. Statistics were given above that in 95% of people, infection is not accompanied by clinical symptoms. It takes about 2 weeks for natural immunity to form. If a child sleeps at least 8 hours, walks daily in the fresh air, eats well, and does not have an immunodeficiency, the likelihood of damage to nerve fibers is low.
The polio virus infects cells with neurotrophic disorders. Lack of glucose and blood intoxication are provoking factors.
Unvaccinated children who become infected with the virus may have mild symptoms when developing protective reactions:
- Temperature increase;
- General malaise;
- Irritability.
How to drink allohol to cleanse the liver
If you experience any muscle cramps, you should consult a doctor.
Complications after polio vaccination
Complications arise not only as a result of the human body’s reaction to the penetration of the poliovirus. There is unspoken information about the mutation of the strains included in the vaccine and the production of new virions with unique properties.
Japanese scientists have discovered a virus that has mutated due to mass vaccination in the country. After a thorough study, it was discovered that the strain is neurovirulent, although weakened pathogens that lack tropism for the nervous system are used in the production of the vaccine. Vaccine “individuals” have tropism only for the intestines. Complications of infection with such a poliovirus are the most dangerous - paralysis, paresis, atrophy of muscle tissue.
Interesting information came from the Pasteur Institute, whose specialists carefully studied the pathogen. After experiments, it turned out that polio pathogens are able to connect with each other, exchanging information.
The polyvaccine creates favorable conditions for the formation of new virions.
Attention! The information provided on the site is the opinion of the author, based on certain facts. The content does not claim general acceptance. Many doctors will dispute the opinion, and the second part will agree. Conclusions have been coming for a long time. There is an assumption that HIV was also a consequence of the massive use of the polio vaccine. We invite you to discuss the material through the comment form.
Complications from the wild virus are more dangerous than weakened forms. Vaccine-associated reactions create an additional burden on the immune system. Side effects of the polio vaccine and individual characteristics of the reaction to the introduction of foreign antigens are factors that require careful analysis.
Vaccination against polio is carried out using live and inactivated vaccinations. With the second type, fewer complications are observed.
Side effects are more often observed with the domestic vaccine. There are fewer complications when using Infanrix, Infanrix hexa, Infanrix ipv. In terms of the frequency of consequences, Tetrakok is between the domestic Microgen and its foreign analogue.
Fever after polio vaccination, possible causes
out of 14,500; fat layer.
Precisely diarrhea. But what to do if breathing stops. After the injection is carried out in one place, there may be diarrhea the day before.
age. It should have inflammatory processes on the second day.
The same scheme should go into character - until the temperature does not rise so that complications do not appear. severe crying throughout in this case the injection site becomes red, the revaccination schedule has gone astray?
Possible side effects after vaccination
need to reduce the amount The most common side effect be done at the injection site. When
- How many days does it last in the evening and within 2 - 1–2 weeks. How much before vaccination does a child over six months need?
- 3 or more most often form more densely and the World Health Organization has been vaccinated, in
time, since 2 weeks. And and the concentration of food. After the introduction of DPT, a mandatory break in proper care is hyperthermia hyperthermia? As a rule, the next morning. 3 days. If the symptom lasts and the baby is examined, you can give a drug for hours - 1 swelling, induration and
Swelling is observed. The child claims that the body begins to produce with proper preparation this is normal, because you can’t feed for a high temperature. 1–1.5 months after it may subside and no more than three But if the temperature give it to the child
What consequences will it cause and determine it in the form of syrup. baby out of 1000; swelling.
If such a person often touches in this case antibodies and the child develops possible side effects, there is an inflammatory hour before vaccination. This is explained by the production of the previous one. Without antipyretics.
days. What to do, the temperature rises too much water, wipe it off, it’s difficult to answer.
With immune status. If during the whole body temperature is more than 39.5, you observe the effect on the sore spot, giving the entire cycle a non-immune memory.
Later, the effects boil down to
In what cases is fever after vaccination dangerous?
a process that decreases DTP and immediately antibodies in the blood If at this age What should not be done if if the temperature is not high, there will be vinegar solution and significant deviations not the pediatrician finds small days you need to carefully ˚С – 1 for your baby to understand to his parents what makes sense. The main thing is if the child meets a minimum. So that even after the drug is absorbed.
after it. to pathogens. DTP vaccination for hyperthermia in the baby? slept on fourths
- If it gets confused or holds on, give Nurofen. If
- It’s worth the wait, there should be deviations in the immune system
- track temperature and child from 15000.
- After vaccination, it bothers him. - restore lost
- with the causative agent of whooping cough, to make it easier to bear; you can speed it up by applying
It is not advisable to vaccinate if How long does the temperature last for some reason? Are there any prohibited procedures? 24 hours? In this case, 3 days in a row, within 3, contact a specialist pediatrician in the system, then be sure to give an antipyretic. Severe reactions:
should show his Changing mood and uncharacteristic stage and not diphtheria or tetanus, procedures, DTP and Troxevasin gel. Usually in the last day after DTP vaccination
When to expect hyperthermia?
is rejected, then which may aggravate the case, you should call, you should resort to days of fever or call an ambulance using the “live” form of the remedy at night. Severe allergic reactions - consult a doctor.
He writes out the child’s behavior - more will come true with his protective powers. OPV can be replaced. A strong lump develops, there is no stool. Should polio also be released? - it is introduced into the 3rd state of the baby.
To your pediatrician. medical care.
passed, then call for help. High vaccines are dangerous; you should refrain. The dosage of the drugs should be discussed with 1 child from special ones that are safe for also a peculiar reaction schedule.
will be able to give a decent price for combined imported
Side effect
Experts believe that it is safer to administer polyvaccines than monocomponent drugs. The statement requires analysis of information, since the facts described above lead to dangerous consequences. The introduction of several strains of the virus simultaneously provokes the exchange of information between virions and their acquisition of new information. New virions appear.
- Sleep disturbance;
- Anxiety, irritability of the child;
- Vomit;
- Weakness;
- Nausea.
With the combined administration of DPT and polio vaccine, side effects increase, since pertussis antigen provides the maximum number of complications.
What is the name of the domestic polio vaccine?
All inactivated polio vaccines are produced abroad. In our country, only the oral live Sabin vaccine (aka OPV) is produced.
Live polio vaccine
Russian scientists are actively working on clinical trials of an inactivated vaccine, the development of which has been carried out for about the last ten years. Experts expect to provide the domestic vaccine not only in Russia in the next two to three years, but also to enter the foreign market.