General concept, classification.
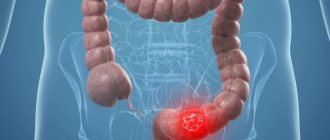
Rectal fistula or fistula (from the Latin fistula - tube) is a chronic disease characterized by the formation of deep pathological canals connecting the rectum with the skin, perirectal tissue or the uterus.
Basically, a fistula is formed as a result of chronic inflammation of the Morganian crypt located in the anal canal. Crypts are blind pockets open to the movement of feces. In the center of the crypt there is a gland that secretes mucus. Thus, fecal lumps stuck in the crypts are enveloped in mucus and easily jump out of the pockets. If this process is disrupted, microbes and foreign substances that enter the crypt cause inflammation, spreading into the perirectal tissue, where an abscess is formed, and when drained, a fistula is formed. There are also other mechanisms of fistula formation, more often associated with traumatic effects on the rectum.
Fistula in the rectum: causes
In 95% of cases, fistulas are a consequence of acute paraproctitis. Chronic disease most often develops for one of 2 reasons:
- Spontaneous opening of the abscess.
- Refusal of radical surgical treatment of acute paraproctitis, the operation performed included only opening and drainage, while the internal intestinal opening (entry gate of infection) remained.
Fistulas can also occur as a result of pathologies:
- Severe chronic intestinal diseases (Crohn's disease, intestinal tuberculosis).
- Other infectious diseases: syphilis, AIDS, chlamydia.
In some cases, chronic paraproctitis develops after:
- Birth injuries (with breech presentation of the fetus, rupture of the birth canal).
- Rectal resections.
- Gynecological operations.
A prerequisite for the occurrence of a fistula is the presence of infection.
Symptoms
Clinical manifestations of rectal fistula closely depend on the severity of the inflammatory process, which is characterized by:
- pain, aggravated by defecation, prolonged sitting, prolonged walking, coughing, laughing
- redness in the area of the fistula tract
- swelling
- increase in body temperature during exacerbation of the disease to 39-400C
If the inflammatory process is mild or absent (observed during drainage of the fistula), there will be practically no symptoms.
When the fistulous tract opens to the surface of the skin of the anal area, patients note the presence of a wound, with the release of ichor (yellowish liquid) or pus with an unpleasant fetid odor. The discharge irritates the skin around the fistula, causing itching. The whole process is accompanied by symptoms of intoxication (general malaise, weakness, nausea, vomiting, sleep disturbance, muscle, joint and headaches).
Internal or incomplete fistulas are more severe due to the inability to drain the abscess. In this case, the pain syndrome and symptoms of intoxication are very pronounced with an increase in temperature up to 400C.
Rectovaginal fistulas, in addition to the listed symptoms, are characterized by frequent exacerbations of colpitis (inflammation of the vaginal mucosa) and vulvitis (inflammation of the external female genital organs).
Rectal fistulas occur with relapses and remissions, that is, with periods of exacerbation and reduction of symptoms until their absence. Relapse is associated with blockage of the fistula tract by growing granulations, purulent-necrotic masses, and therefore an abscess with symptoms of acute inflammation is formed in the fistula cavity. Full recovery does not occur; after some time the symptoms resume.
Branch
An anal fistula is a small canal (passage, tunnel) in the tissue that begins at the mucous membrane of the end of the colon and opens outward on the skin around the anus.
An anal fistula is formed, as a rule, as a result of an acute infectious process of surrounding tissues in the form of a limited accumulation of pus (abscess). After the abscess empties, a small canal forms at the site of the passage of pus, giving rise to the disease.
Anal fistula manifests itself with a number of unpleasant symptoms. Among them: a feeling of discomfort, irritation of the skin of the anal area. Most anal fistulas require surgical treatment.
Symptoms of anal fistulas.
Symptoms of an anal fistula include:
- irritation of the skin around the anus.
- constant throbbing pain, aggravated by sitting, changing body position, defecation and coughing.
- foul odor emanating from the perianal area.
- discharge of pus or blood in the stool.
- redness of the skin, swelling and increased temperature of the tissues around the anus if an abscess forms.
- in some cases, impaired control of the bowel movement process (stool and gas incontinence).
Ultimately, a fistula can be visually identified as a hole in the skin next to the anus from which pus is released. However, it can be difficult for the patient to see it on their own.
When to go to the doctor
Go to the doctor if you notice signs of an anal fistula. Your doctor will evaluate your symptoms and your bowel function.
For a more detailed assessment of the manifestations of an anal fistula, a doctor's examination may include a digital rectal examination.
If the doctor confirms your suspicions, he will refer you to a coloproctologist for a more detailed examination in order to clarify the diagnosis and determine the optimal treatment method.
An examination by a coloproctologist surgeon will usually include:
- detailed general examination and rectal examination.
- proctoscopy (this is an examination with a special optical device with light that is inserted into the anus), colonoscopy.
- Ultrasound examination (including rectal), magnetic resonance imaging (MRI) or computed tomography (CT).
Causes of anal fistulas.
Most anal fistulas develop as a result of acute inflammatory diseases of the perianal (surrounding the anus) area, most often abscesses that were not subjected to specialized treatment and opened independently (the channel for the passage of pus becomes the channel for the fistula).
Half of patients with anal abscesses develop an anal fistula.
To a lesser extent, the formation of an anal fistula is promoted by:
- Crohn's disease is a condition in which inflammation in the digestive system persists for a long time
- Diverticulitis – infection from diverticula (small protrusions in the wall of the large intestine) can spread beyond the colon.
- Hidradenitis suppurativa is an inflammatory skin disease accompanied by the formation of abscesses and scars.
- specific infections – tuberculosis and HIV.
- complication of surgical interventions near the anus.
Treatment of anal fistula
Most cases of anal fistula require surgical treatment and only in rare cases does spontaneous recovery occur.
The main types of surgical interventions for rectal fistula:
- fistulotomy is a procedure for opening the fistulous tract along its entire length (the resulting wound gradually heals later).
- ligature technique - when a surgical thread (ligature) is passed through the fistula canal and left in it for several weeks. The thread is gradually tightened, passes through the tissue, and the resulting wound surface heals.
- other technologies - including filling the fistula with biological glue, filling with special devices, closing the wound defect with a blood-supplied tissue flap.
All of the above operations have their advantages and disadvantages. You can talk to your proctologist about this in more detail.
Sometimes surgical interventions for anal fistulas do not require hospitalization, but in some cases postoperative hospital treatment is required.
Surgery
The main method of treating anal fistulas is surgical. In very rare cases, spontaneous healing is observed. The choice of surgical treatment method depends on the specific characteristics of your disease (localization of the fistula tract, the number and direction of its branches). In some cases, to determine the tactics of surgical treatment, it is necessary to conduct a detailed instrumental examination of the anal area under general anesthesia (while the patient is asleep).
A coloproctologist surgeon will assess your situation and suggest the optimal surgical method for you.
Surgery for an anal fistula is usually performed under general anesthesia. In most cases, postoperative hospital treatment is required. The goal of surgery is to remove the fistulous tract, avoiding damage to the anal sphincter (the circular muscle that closes and opens the anus), to avoid the development of future anal sphincter incompetence (fecal and gas incontinence).
The main types of transactions are shown below.
Fistulotomy.
The most common treatment for anal fistula is fistulotomy. The method consists of dissecting the fistula tract along its entire length, forming an open wound. Afterwards, spontaneous healing of the resulting wound defect occurs.
Fistulotomy is the most effective treatment for anal fistula. Its use is most justified for fistulas that do not pass through the anal sphincter, in which case the risk of anal sphincter failure is minimal.
If the surgeon has to dissect a small portion of the anal sphincter, he takes all necessary measures to prevent its failure. In cases where the risk of developing sphincter incompetence after fistulotomy is assessed by the surgeon as high, he may offer you an alternative surgical technique.
Ligature method.
If your fistula passes through a significant portion of the anal sphincter, your surgeon may recommend starting surgical treatment with a ligature. A ligature is a fragment of surgical thread that is inserted through the anal fistula canal and left there for several weeks. This promotes good drainage of the fistula and, in some cases, ensures healing of the fistula without cutting the sphincter. The use of a free ligature promotes drainage, but does not always lead to healing of the fistula. In such cases, they resort to tightening the ligature. By tying the ends of the ligature together in a tense position, the surgeon achieves its slow, gradual cutting through the tissue. Tightening is carried out in several stages, this requires several patient visits.
As an alternative, the surgeon may suggest a step-by-step gradual dissection of the fistula tract as the ligature is tightened.
Plastic method
The plastic method of treatment is considered for complex fistulas passing through the sphincter, when the use of fistulotomy is associated with a high risk of developing anal sphincter incompetence.
The plastic method involves, after dissecting the fistula tract and removing purulent streaks, isolating a mucomuscular flap and moving it to the site of the wound defect in order to close the fistula. This method is inferior in effectiveness to fistulotomy, but avoids cutting the circular muscles of the anal sphincter.
Use of biological implants
This method is also used for complex transsphincteric fistulas, where fistulotomy is associated with an increased risk of failure.
The method consists of introducing a conical plug made of biological tissue of animal origin into the fistula cavity in order to seal the internal fistula opening.
Some studies show the effectiveness of this method in the treatment of anal fistulas, but it needs further study.
Bandaging the fistula.
Another relatively new surgical method for treating a rectal fistula is its ligation at the level of the anal sphincter. This technique was developed for transsphincteric (passing through the anal sphincter) fistulas with high risks of fistulotomy. A skin incision is made directly above the fistula. A part of the fistula is isolated from its external opening to the anal sphincter. At the level of the anal sphincter, the fistula tract is ligated and the selected part is excised. The resulting wound defect heals on its own. The current results of the ligation operation are promising. Currently, the study of its immediate and long-term results continues.
Fibrin glue.
The use of fibrin glue is the only non-operative technology in the treatment of anal fistula.
The technology consists of the surgeon introducing a special adhesive solution into the fistula tract when the patient is under general anesthesia. The glue seals the fistula tract, which creates conditions for healing.
This procedure is inferior in effectiveness to fistulotomy and does not always achieve lasting long-term results. However, it can be useful in transsphincteric cases, since it does not require dissection of the muscular structures of the anal sphincter.
Complications of surgical interventions for anal fistulas
Like any type of treatment, surgery for anal fistulas is associated with a certain risk and is accompanied by a number of complications.
The most common complications:
- infectious complications - antibiotics must be prescribed, in some cases additional hospital treatment is required.
- relapse of the disease - despite surgical treatment, anal fistulas can recur.
- incompetence of the anal sphincter - the risk of this complication always exists, regardless of the chosen technique, provided that all necessary precautions are observed.
The degree of risk of complications depends on the localization of the anal fistula and the chosen method of surgical treatment. Discuss the potential risks of your surgery with your surgeon.
Treatment.
There are two types of treatment for rectal fistula: conservative and surgical. But the only effective and proven treatment is surgical treatment, the essence of which is the excision of the fistula tract and the inflamed crypt. The operation is performed during an exacerbation period, because during remission, the boundaries of the fistula tract are unclear. In addition, etiotropic therapy is carried out aimed at eliminating the cause, for example, an infectious agent.
Conservative treatment is carried out for small fistulas by closing the passage with specialized biological glue.
Complications of chronic paraproctitis
If left untreated, the following complications may occur:
- Regular exacerbations with the appearance of purulent cavities and infiltrates in the soft tissues.
- The appearance of scars in the anal canal, soft tissues near the anus, or the muscles of the anal area.
- Decreased potency.
- Deformation of the anal canal or rectum.
The listed signs may be accompanied by the following symptoms:
- General malaise.
- Increased body temperature.
- Swelling in the anus.
Diagnostics
Diagnosis of fistulas is carried out during an examination by a proctologist.
The patient is positioned on a gynecological chair. The external fistula opening in the anal area is determined visually. The presence of scar tissue along the fistula can be detected using digital examination. However, this method is suitable for intrasphincteric and transsphincteric fistulas. Extrasphincteric fistulas are not easy to diagnose using this method.
Also used to diagnose fistulas are:
- Sphincterometry is a hardware diagnostic method used to assess sphincter tone.
- Probing the fistula - determining the direction of the fistula tract.
- Sigmoidoscopy – assessment of the condition of the rectal mucosa.
- Fistulography is an x-ray examination using a contrast agent.
- Ultrasound of the rectum.