The large intestine is the part of the digestive system in which the digestion process ends and undigested residues are excreted. The large intestine begins from the ileocecal angle (the transition of the ileum to the cecum) and ends with the anus. The Bauginian valve, located at the beginning, allows the food bolus to pass in only one direction.
Where is the large intestine located?
The large intestine is the lower, final part of the digestive tract, in which water is mainly absorbed and formed feces are formed from food gruel (chyme). The large intestine got its name due to the fact that its walls are somewhat thicker than the walls of other parts of the intestine - this is due to the greater thickness of the connective tissue and muscle layers.
Sections of the colon:
- cecum with vermiform appendix;
- colon: ascending, transverse, descending and sigmoid colon;
- the rectum, which consists of the ampulla, anus and anus.
The large intestine is a large, hollow organ of the digestive tract. It performs many important functions, while constantly being in contact with food masses. As a result, the colon is constantly exposed to various harmful factors that can cause deterioration in its functioning. Diseases of this part of the digestive system, according to medical statistics, are the most common today.
The large intestine is the last section of the gastrointestinal tract. The length of this section ranges from 1.1 to 2-2.7 meters, and the diameter reaches 5-6 cm. It is much wider than the small intestine, approximately 2.5 times. The lumen of the large intestine narrows closer to the exit from the rectum, which ends in a sphincter that allows for normal voluntary bowel movements.
How do sphincters work?
In addition to the sphincter, which separates the rectum from the sigmoid colon, there are three more sphincters along its length, each of which differs in structure:
- Nelaton's sphincter consists of many smooth muscle fibers that are located circumferentially or circularly. The top of the sphincter is covered with additional mucous membrane.
- The involuntary (internal) sphincter separates the section of the perineal flexure and the section that follows it and extends to the external sphincter. The smooth muscle fibers of this sphincter are located not only circumferentially, but also longitudinally and transversely. The sphincter is long, about 1.5-3 cm. The fibers, which have a longitudinal arrangement, enter the distal part of the sphincter and there go into the skin membrane. This sphincter differs in thickness between men and women. In the first case it is thicker.
- The voluntary (external) sphincter, unlike other sphincters, is entirely composed of striated muscles. The origin of the muscle that forms this section comes from the puborectalis muscle. The length of the sphincter is located at the border of 2.5-5 cm. This sphincter is important because it is regulated by the will of the person and, if the nerve fibers are damaged, fecal incontinence may occur. The anus is based on the work of this sphincter, which is a complete section of the rectum. The rectum is one of the few organs that obey the conscious will of a person.
Bowel functions
The large intestine ensures the completion of the movement of chyme through the digestive tract. It communicates with the external environment, which determines the specificity of its functions:
- Excretory. The main function of the large intestine. Aimed at removing various pathogens and unprocessed substances from the body. This process must occur regularly and without failures, otherwise, due to the abundance of toxins in the digestive tract, poisoning of the body develops. It is in the large intestine that stool is finally formed, which is then excreted from the rectum. The excretory function is stimulated by the next meal. After a person eats food, his brain receives a signal that increases intestinal motility and accelerates the movement of chyme towards the anus.
- Digestive. Most of the nutrients are absorbed in the small intestine, but some of the components of chyme enter the body from the large intestine: salts, amino acids, fatty acids, monosaccharides, etc.
- Protective. The large intestine contains about three kilograms of beneficial microflora, which not only ensures normal digestion, but also promotes the functioning of the immune system. Disruption of the bacterial balance leads to a decrease in the body's protective function, increased susceptibility to infectious diseases, etc.
- Suction. It is in this section of the digestive system that the bulk of the liquid is removed from the feces - more than 50%, which prevents dehydration of the body. Due to this, feces acquire a characteristic consistency and shape.
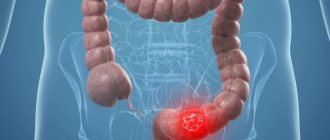
Rectal cancer
Cancer develops in the rectum
Organ cancer is equally common among men and women. There are a number of diseases that usually precede the formation of a tumor. These include:
- adenomatous polyps (including familial ones);
- ulcerative colitis;
- Crohn's disease;
- paraproctitis in chronic form.
Rectal cancer is a fairly common disease and the percentage of cases has been increasing in recent years.
Rectal cancer is a disease that rarely has a transient nature, much more often developing slowly, gradually. The severity of symptoms often depends greatly on how big the tumor is and where it is located.
Sphincters of the colon
The presence of a large number of physiological sphincters in the colon ensures its motility.
- The ileocecal sphincter of Varolius is located at the junction of the ileum and the cecum.
- The colocecal sphincter of Busi separates the cecum and ascending colon.
- Geertz's sphincter is located on the border of the middle and upper third of the ascending colon.
- The right and left Kenon sphincters are located, respectively, near the right and left bends of the transverse colon.
- Horst's sphincter is located in the middle third of the transverse colon.
- The sphincters of Pyra and Bally limit the descending meningeal colon above and below.
- The Rossi-Moutier sphincter is located in the middle third of the sigmoid colon.
- The Auburn-Pirogov-Muthier sphincter is in the last third of this intestine.
Sphincters are wide folds that are closed in the normal state and straighten during peristalsis.
General structure and functions of the intestine (small and large)
The intestine is the longest part of the human digestive tract. They are distinguished: a small intestine 4-6.5 m long, in which the digestion and absorption of nutrients occurs, and a large intestine 1.1-2.1 m long.
The small intestine at the exit from the stomach begins with the duodenum, 18-22 cm long. The ducts of the liver and pancreas flow into it (Fig. 88). Pancreatic juice enzymes break down proteins (trypsin), fats (lipase) and carbohydrates (amylase, lactase). They are active only in an alkaline environment and are activated by bile.
Bile is produced by the largest gland in our body - the liver. Bile contains water, bile acids and the pigment bilirubin. It accumulates in the gallbladder and is released when a bolus of food enters the duodenum. The main function of bile is the emulsification of food fats. Only in the form of small droplets in an aqueous solution (emulsion) can fats be etched by lipase. Bile enhances intestinal motility and performs a disinfecting function. Regulation of the production of pancreatic juice and bile is ensured by reflex (nervous) and humoral mechanisms. Unconditioned reflexes are predominant.
| Rice. 88. Liver, duodenum and pancreas: 1 - right lobe of the liver; 2 - left lobe of the liver; 3 - gallbladder; 4 - common hepatic duct; 5 - pancreatic duct; 6 - pancreas; 7 - duodenum; 8 - gallbladder duct; 9 - common bile duct |
The duodenum passes into the small intestine, and then into the ileum. Almost along the entire length, the diameter of the small intestine is 3-5 cm. Its walls, like other parts of the digestive tract, consist of four layers. The mucous membrane of the small intestine, thanks to the submucosal layer, is collected into folds - intestinal villi. They greatly increase the digestive and absorption surfaces (Fig. 89). Epithelial cells are covered with microvilli. Digestive enzymes are placed on them in a certain sequence, ensuring parietal digestion. Thanks to the villi, the absorption surface of the small intestine reaches 450-550 m2, which is 300-380 times the surface area of the human body. The mucous membrane of the small intestine contains many small glands that produce intestinal juice. Under its influence, the breakdown of proteins into amino acids, fats into glycerol and fatty acids, and carbohydrates into glucose ends.
| Rice. 89. Villi of the small intestine: 1 - outer (mucous) membrane; 2 - submucosal layer; 3 - muscular layer; 4 - serous membrane; 5 - lymphatic capillary; 6 - arterial part of the capillary; 7 - venous part of the capillary; 8 - vein; 9 - artery; 10 - lymphatic vessel |
The muscular layer of the intestinal wall ensures mixing of the food bolus due to pendulum-like contractions and its movement as a result of peristaltic contractions.
The total duration of the movement of the food bolus and its digestion in the small intestine is 6-7 hours. Material from the site https://worldofschool.ru
| Rice. 90. Absorption of nutrient breakdown products by the villi: 1 - proteins; 2 - fats; 3 - carbohydrates; 4 - blood capillaries; 5 - lymphatic capillary |
In the small intestine, nutrients are absorbed by the villi. In the center of each villi there is a lymphatic capillary, and on both sides there are small arteries and veins that branch into capillaries (Fig. 89). Smooth muscles located in the walls of the villi contract rhythmically during digestion (5-6 times per minute), squeezing lymph from the lymphatic capillary. When the muscles relax in the middle of the villi, a negative pressure arises relative to the intestinal cavity, which draws water, mineral salts, vitamins and nutrients into the villi (Fig. 90).
Undigested food remains from the small intestine enter the large intestine due to peristalsis. The large intestine has: the cecum with the appendix, colon, sigmoid and rectum. E. coli constantly multiplies in the appendix, which breaks down plant fiber, synthesizing vitamin K and B vitamins. Water is absorbed in the large intestine and feces are formed, which enter the rectum. When the appendix becomes inflamed, a disease occurs that is accompanied by pain in the lower abdomen, fever, nausea and vomiting. If such symptoms occur, you should immediately call a doctor.
On this page there is material by topic: Questions about this material:
worldofschool.ru
Blood supply of the large intestine
The intestinal blood supply comes from two mesenteric arteries - superior and inferior. The large intestine is supplied with blood by the superior mesenteric artery to the left flexure. The inferior mesenteric supplies blood to the left parts of the colon.
The distribution of blood to all parts of the intestine is carried out by straight vessels, which arise from a parallel vessel running along the entire mesenteric edge. Along with the arteries there are veins and lymph nodes of the same name.
With mesentral insufficiency of the inferior mesenteric artery, areas of the colon are affected, in 80% of cases in the area of the left flexure. This leads to the development of ischemic colitis.
Large intestine: diseases and their prevention
As in the case of the thin section, the following may lie in wait for us here:
- functional problems, colitis;
- impaired digestion and absorption;
- neoplasms - polyps, benign tumors, cancer;
- inflammation and infections;
- dysbacteriosis;
- varicose veins - hemorrhoids.
Increased motility, rapid formation of gases and excessively rapid movement of masses towards the exit cause the water to not be absorbed in time and at the exit we get diarrhea. Many who want to urgently lose weight are looking for how to cleanse the gastrointestinal tract and resort to teas and tablets that stimulate peristalsis. This can lead to irritable bowel syndrome and the evacuation of beneficial microflora.
Congestion, on the contrary, can cause stool retention, constipation, bloating and obstruction. This condition is also very dangerous.
As usual, let me remind you that self-medication is excluded. If you have pain, gas, cramps or other symptoms, consult your doctor. You will be prescribed tests and hardware tests. The most effective and reliable means of making a diagnosis is colonoscopy. When carried out correctly, this procedure is practically painless, allows you to identify tumors in the early stages and prescribe effective treatment.
Let us not forget that there are a lot of dangerous infections in which the mucous membrane is affected and the large intestine ceases to perform its functions. Since it is responsible for cleansing the body, removing waste and toxins, we must take special care of its condition if we want to remain healthy and beautiful.
Of the most well-known diseases, you need to remember about appendicitis - acute inflammation of the appendix, as well as hemorrhoids. Hemorrhoids can form both inside the rectum and in the sphincter area. This leads to pain, discomfort, weakened sphincters, fecal incontinence, cracks and inflammation.
Movement and proper nutrition are the key to preventing problems with hemorrhoids.
How does digestion occur in the large intestine?
- The digested food mass sooner or later ends up in the large intestine, where water and mineral salts are absorbed. Those food residues that were not digested in the previous section are also transferred here. All these movements take about 12 hours.
- The colonic section contains microorganisms that cause rotting and fermentation. These bacteria are not capable of harming the body only if they do not enter other parts of the body. Residues of food, together with waste products and pigments, form feces, which are stored until removed.
- The composition of the colon microflora is balanced. If its composition is qualitatively or quantitatively changed, this will lead to the occurrence of dysbacteriosis.
- The structural components of this organ are the glands responsible for the production of mucus. It contains few enzymes, so food is promoted better. This mucus, formed in the colon, contains antibodies that protect the organ from pathologies.
- The walls of the large intestine contain blood and lymphatic vessels.
Methods for diagnosing the colon
- X-ray of the abdominal organs with contrast. It is the main method for diagnosing diseases of the colon. The method is based on the penetration of X-rays through the intestine, which contains a radiopaque substance (barium suspension), and obtaining images. Using this method, developmental anomalies and intestinal obstruction can be diagnosed. Assess the condition of the intestinal mucosa, tone and peristaltic movements, the speed and nature of the movement of barium suspension through the intestine. The disadvantages include the difficulty of diagnosing tumors in the early stages of development.
- Colonoscopy. An endoscopic diagnostic method, which is based on visual examination of the inner wall of the intestine using an endoscope. Under visual control, the doctor can judge the condition of the mucous wall, identify organic pathology (polyps, erosions, tumors), and take biopsy material. The disadvantages of the study include the presence of a special preparatory stage before the study, the painfulness of the procedure, and the inability to evaluate other intestinal linings.
- Computed tomography (CT). A modern diagnostic method is based on the penetration of X-rays into the abdominal cavity in different planes simultaneously and reading information by several sensors at once. Using a computer program, an image of the intestines and surrounding organs and tissues is obtained in several planes. CT reveals tumors with minimal size, metastases, organic pathology, inflammatory changes, and developmental abnormalities.
- MRI (magnetic resonance imaging). The method is based on layer-by-layer examination of the required area of the body using magnetic fields. MRI is used to diagnose neoplasms, inflammatory processes in the intestines, and metastases in surrounding tissues. It is a safe research method. Not used only if there are metal objects in the body.
- Ultrasound. Advanced ultrasound diagnostics allows you to examine the intestines. Ultrasound reveals tumors in the intestinal wall, inflammatory changes in the walls of the colon. At the same time, nearby organs and tissues can be examined.
- Endoscopic ultrasound diagnostics. A type of ultrasound diagnostics is this method, which is based on the introduction of an ultrasound sensor into the intestinal lumen through the rectum. This position of the sensor allows you to accurately determine from which intestinal lining the tumor is growing, and to determine the presence of compression of surrounding tissues.
- Diagnostic laparoscopy. An invasive method that is based on microsurgical insertion of endoscopes through incisions in the anterior abdominal wall. More often it combines diagnostic testing and surgical treatment (removal of part of the intestine).
We recommend reading:
Colorectal cancer: early and late symptoms, treatment methods and prognosis for life
In continuation of the topic, be sure to read:
- Sigmoid colon: location, structure, functions and diseases of the organ
- Diseases of the sigmoid colon: symptoms and signs of disease, their treatment
- Sigmoiditis (inflammation of the sigmoid colon): symptoms and treatment methods
- Proctitis: symptoms and treatment methods (diet, drugs, surgery)
- Preparation and performance of intestinal sigmoidoscopy
- Intestinal dolichocolon in adults: definition of pathology and treatment
- Details about the intestines: structure, sections and functions of the organ
- Large intestine: location, structure and functions
- Diseases of the colon: symptoms and signs of pathologies, treatment
- Intestinal colonoptosis: definition, symptoms, treatment and prognosis
Features of pain syndrome in pathologies of the large intestine
Pain syndrome in diseases of the large intestine has its own characteristics:
- localization - meso- and hypogastrium;
- irradiation - does not irradiate;
- more associated with the act of defecation rather than with food intake;
- relief occurs after defecation or passing of gas;
- with damage to the rectum and sigmoid colon - tenesmus (painful and frequent muscle contractions in the anus and false urge to defecate).
Pain in the intestines is often accompanied by bloating, constipation, diarrhea, and the appearance of pathological impurities in the stool (blood, mucus, pus, undigested food).
General signs of diseases of the large and small intestines
Intestinal diseases are accompanied by the following groups of symptoms:
- large intestine hurts;
- dyspepsia;
- dyskinesia;
- malabsorption and maldigestion syndrome;
- bleeding syndrome.
Visceral pain occurs when the receptors of the hollow organs of the gastrointestinal tract (GIT) are irritated. It can be spastic (with spasm of smooth muscles) and distensional (with stretching of the organ). Characteristics of pain syndrome:
- unclearly localized;
- reflex autonomic reactions often occur (vomiting, changes in blood pressure and pulse);
- pain on palpation.
What to do to keep your rectum healthy
A small set of rules significantly reduces the likelihood of rectal lesions.
- Maintain hygiene.
- Eat enough fiber, moderate amounts of meat, alcohol, and spicy seasonings.
- Don't overeat at dinner.
- Strengthen the muscles of the pelvis and diaphragm.
- Do a simple exercise every day. Squeeze and relax the muscles of the perineum as many times as you are old.
- Try not to restrain the natural urge to defecate, so as not to disrupt the body’s regulatory mechanisms.
data-matched-content-rows-num=”4.2″ data-matched-content-columns-num=”1.2″ data-matched-content-ui-type=”image_stacked” data-ad-format=” autorelaxed">
Colon diseases
Typically, with pathology, pain is localized on the side of the abdomen. A lot of complaints from patients are about pain in the intestine on the left; this occurs due to infectious inflammation, which intensifies with movement.
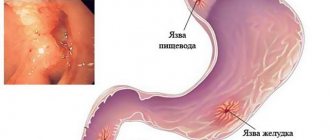
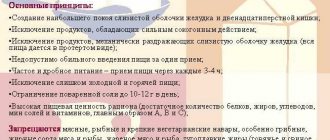
Ulcerative colitis
Pathological disease. With this disease, the mucous membrane of the colon suffers. A sign of the disease is a long course with worsening symptoms. Painful symptoms are localized at the bottom left.
The etiology of the disease is still unknown. Suggestions have been made about the involvement of hereditary pathology of the immune system. Patient complaints of weakness, weight loss, and general malaise are typical. Disease management continues for a long time. It is recommended to eliminate dairy products due to increased sensitivity to milk proteins.
Proctitis
Inflammatory process due to constipation, injury, infection. Often, cancer and benign tissue formations above the mucous membrane progress in the rectal area. The anus is prone to pain that increases when walking.
Ischemic colitis
The main symptom is stenosis, which provokes inflammation. At the initial stage of the disease, short-term pain is present in the left side of the abdomen. Subsequently, an ulcer may develop. Ischemic colitis predominantly progresses in the sigmoid and transverse colon.
Colon tumors
There are two types of tumors: benign and malignant. The most common malignant type. Today, colorectal cancer is the most common malignant tumor.
There are extremely few specific indicators by which cancer can be detected at the initial stage. If you have intestinal disorders, it is important to seek help from a doctor in order to identify a tumor in the intestines at an early stage.
Irritated colon
A group of intestinal disorders expressed by pathologies of motor function in the absence of organic changes. Patients begin to experience stomach pain, stool disturbances, and bloating. The nature of the pain is uncertain - sharp, stabbing, cutting.
Treatment depends on the doctor's ability to identify the etiology that is at the root of the disease. Doctors recommend following a loyal diet. In the chronic course of the disease, dysbiosis or disruption of a group of microorganisms found in the natural conditions of the intestine may occur.
Diverticulosis
As a result of the disease, local pouch-like protrusions appear in the intestinal wall. They often form in older people. The reason is an insufficient amount of plant-based food in the diet. In addition to constipation, the formation of diverticula is promoted by:
- Excessive body weight.
- Excessive use of laxatives.
- Increased gas formation.
The main method in treating the disease is to regulate bowel movements.
Dolichosigma
Elongated sigmoid colon. It can be either congenital or acquired. The course of the disease occurs without obvious symptoms. Usually treatment is conservative and aimed at normalizing stool. Surgery is required to resect the accessory sigmoid loop.
Megacolon
Enlargement of part or all of the colon. The need for surgical intervention depends on the form of the disease. If surgery is required, the enlarged part is removed.
Rectal prolapse - symptoms and treatment
For rectal prolapse and especially internal intussusception, one of the leading methods of treatment is surgical, however, in the initial stages, the course of treatment should begin with conservative measures. The main directions of therapy are the normalization of stool and passage of intestinal contents. To this end, the first step is to prescribe a diet rich in fiber, as well as drinking plenty of fluids. The next step is the prescription of laxatives that increase the volume of fecal contents, as well as enhancing intestinal motility. Medicinal preparations of plantain seeds, for example “Mukofalk,” have become widespread. The latter is prescribed 1 sachet or 1 teaspoon up to 5-6 times a day.
Conservative methods of treating rectal prolapse also include neurostimulation methods. These methods include biofeedback therapy and tibial neuromodulation. This therapy is aimed at normalizing innervation. The biofeedback method is based on modeling the normal functioning of the muscles of the perineum and pelvic floor. The technique is a visualization of signals from sensors located in the rectum and on the skin of the perineum. The data is displayed on a monitor or as an audio signal. The patient, depending on the regimen or planned program, is able to control muscle contractions through volitional effort. Regular procedures can achieve a positive effect in 70% of patients with impaired innervation of the pelvic floor muscles. Tibial neuromodulation involves stimulating the tibial nerve to strengthen the perineal and anal sphincter muscles. Two electrodes are placed on the medial malleolus area. The impulses are given with periods of relaxation and tension.
Conservative methods lose their effectiveness with further development of the disease. In these cases, it is necessary to resort to surgical correction methods. All surgical interventions, depending on the access, are divided into perineal and transabdominal, which, in turn, can be divided into open and laparoscopic.
Despite the positive effect of conservative treatment methods, the most effective is the use of surgical methods for correcting rectal prolapse.[14] Currently, many methods of surgical treatment of rectal prolapse have been described in world practice. All described techniques can be divided depending on the access used through the perineum or through the abdominal cavity. Perineal treatment options are more preferable for patients with existing severe concomitant pathology, since such operations are less traumatic. Along with less trauma, it is worth noting the high frequency of relapses, as well as postoperative complications.
Among perineal interventions, operations such as:
- Delorme;
- Altmeer;
- Longo.
The essence of the Delorme operation is that the mucous layer is cut along the entire circumference two centimeters proximal to the pectineal line. Next, after preparation, the prolapsed area is excised from the underlying layer. Sutures are placed on the muscle layer in the longitudinal direction to create a cushion, after which the mucous layer is sutured. The advantages of this operation are low trauma and a significant increase in the function of the anal sphincter, which leads to improved retention of fecal components. However, based on data from various studies, the incidence of relapses is higher than during operations through the abdominal cavity, and the incidence of complications, such as acute urinary retention, postoperative bleeding and impaired passage of intestinal contents, reaches 15%.
During rectosigmoidectomy or Altmayer's operation, it is necessary to dissect the mucous layer of the rectum along the entire circumference two centimeters above the dentate line, as in the Delorme operation. The next stage is the mobilization of the sigmoid and rectum and ligation of the vessels to the level of absence of excessive mobility. Next, the excess mucosa is cut off, after which it is necessary to apply a hardware or manual anastomosis. The positive side of this surgical intervention is the low percentage of bleeding from the anastomotic line, its failures, as well as a small number of purulent complications in the pelvic tissue. Recurrence of the disease is up to 30%, which, according to research, decreases by 3-4 times if this operation is supplemented with plastic surgery of the levator muscles.
The Longo operation, also called transanal proctoplasty, involves the use of circular staplers. During this operation, semi-purse string sutures are applied to the mucosa along its anterior and posterior surfaces. Next, one by one, the anterior semi-purse-string suture is first tightened on the head of the stapling apparatus, with excision of excess mucosa, then the sutures are tightened along the posterior semicircle on the head of the stapling apparatus and the excess mucous is cut off in the same way as the anterior semicircle. The Longo operation can also be performed through the abdominal cavity, which expands the possibilities of this operation, allowing it to be used in a wider range of patients, including those with concomitant pathologies. The rate of postoperative complications reaches 47%.
Despite the minimal trauma of perineal interventions, the high percentage of relapses causes their limited applicability. In recent years, an increasing percentage of surgical interventions are performed through the abdominal cavity, and most of the proposed techniques are either modifications of the described operations or are of only historical interest and are not currently used.
The minimal percentage of relapses and better functional results compared to perineal operations determine the wider introduction of transabdominal interventions. It is worth noting that due to the high percentage of postoperative complications in this type of operation, its application to elderly patients with severe concomitant pathology is limited.
Among the most common interventions it is worth noting:
- method of anterior rectal resection;
- rectopexy;
- rectopromontofixation;
- surgical intervention according to Wells;
- surgical intervention according to Zerenin-Kümmel.
For anterior resection, laparoscopic or open, an incision is made in the root of the mesentery of the sigmoid colon up to the pelvic region, bordering the rectum. Next, mobilization of the sigmoid and rectum is necessary, and in the presence of a solitary ulcer, mobilization is carried out below its level, i.e., with the capture of the ulcerative defect in the mobilized area. The selected area is cut off and both ends of the intestine are sutured; linear cutting devices are often used. Next, the head of a circular stapling device is inserted into the afferent end of the intestine, and the circular stapling device itself is inserted through the anal canal and, aligning the head with the device, an end-to-end anastomosis is performed. After monitoring hemostasis and the consistency of the anastomosis, the operation is completed. According to research, the percentage of relapses during such an operation increases over time and reaches 12-15%. Complications occur in approximately one third of patients. It is worth considering the increasing number of patients who develop one or another degree of anal incontinence (incontinence), associated with lower rectal secretion, necessary for the removal of a low solitary ulcer.
With rectopexy, the rectum is fixed above the promontory of the sacrum. Often, the first stage is rectal resection, with the anastomosis located above the sacral promontory. This method is characterized by a relatively low relapse rate, reaching 5%, while postoperative complications occur in approximately 20%. Also, some studies indicate improved intestinal transit.
A number of authors are convinced of the need for subtotal resection of the intestine, however, recent studies indicate the refusal of an expanded volume in patients with anal incontinence, since patients experience deterioration in the function of the anal sphincter.
Rectopromontofixation begins with mobilization of the rectum to the right of it along the posterior and lateral semicircle up to the lateral ligament. In women with prolapse of the rectovaginal septum, the latter is dissected and mobilized to the anal sphincter. In men, mobilization is carried out to the border of the middle and lower third of the ampullary section of the rectum along the posterior semicircle. Next, a mesh prosthesis is fixed to the isolated intestinal wall. In case of rectocele, the posterior vaginal vault is additionally fixed. The other end of the prosthesis is fixed to the promontorium.
Scheme of rectopromontoriofixation
A review of studies with large numbers of patients found recurrences to occur in 3.5% of cases, while postoperative complications occurred in 25%. Disturbances in the passage of intestinal contents occurred in an average of 15% of cases.
The Wells operative method consists of dissecting the peritoneum above the promontory of the sacrum down to the pelvic peritoneum and rectum on both sides. Next, the intestine is isolated to the levator muscles along the posterior and lateral semicircles, to which the mesh prosthesis is fixed. The other end of the prosthesis is fixed to the promontory of the sacrum across the axis of the latter. The relapse rate after this type of intervention reaches 6%, constipation occurs in 20%, and signs of anal incontinence occur in approximately 40% of cases.
The surgical method according to Zerenin-Kümmel consists in opening the peritoneum to the pouch of Douglas in front of the rectum, the latter is isolated to the levators. Further from the promontory and below, sutures are applied, including the longitudinal ligament, and the line of sutures is continued on the anterior wall of the rectum. When tightening the sutures, a rotation of 180 degrees occurs, eliminating the deep Douglas pocket. Relapse, according to the literature, occurs in approximately 10% of patients.
Large intestine: structure and functions
The large intestine (lat. intestinum crassum) is distally adjacent to the small intestine, extending from the ileo-blind processes of the valve to the anus. It consists of the cecum with the appendix, colon and rectum. Thus, the terminal part of the human digestive tract is formed.
Large intestine: structure and functions
Location of the large intestine
The large intestine originates from the ileocecal valve, which protects the small intestine from bacterial reflux. The adjacent cecum, located on the lower right side of the abdomen, is a blind pouch. Attached to it is an appendage, also known as the vermiphalic appendage. As a rule, it is located retrocecally, therefore, behind the cecum. The location of the appendage is variable. The ascending part of the large intestine is connected to the cecum and runs up to the chest.
Anatomy: parts of the large intestine
At approximately the level of the 9th rib, the curvature of the colon bends strongly inward to the left, forming the hepatic flexure. The transverse part passes like a garland above the loop of the small intestine, and ends with the splenic flexure in the left half of the body. From this point on, the descending part leads towards the left anterior iliac spine. The S-shaped bend with the rectum forms the distal end of the large intestine.
Appearance
The length of the large intestine is about 1.5 m and the diameter is 5-8 cm. It runs around the small intestine in the form of a frame.
Important macroscopic features of the walls of the large intestine are the haustra or group of pouches. If they are located in the inner wall of the intestine, they are called plicae semilunares coli.
Appearance of the large intestine
Colon segments:
- Cecum (cecum) with appendage.
- Hind intestine.
- Large intestine: ascending, colon, descending, sigmoid.
- Rectum.
Parts of the human colon
Large intestine relative to the abdominal cavity
In general, it can be noted that the sections of the colon alternate between intra- and retroperitoneal sites. Therefore, the cecum with its appendage is intraperitoneal. The blood vessels of the appendix pass through the mesoappendix leading to the cecum and ileum.
Structure and location of the appendix
The ascending and descending colon are secondary retroperitoneal. In turn, the colon and sigmoid are intraperitoneal. The gastrocolic ligament connects the greater curvature of the stomach to the colon. Behind it there is an omental bag.
Large intestine relative to adjacent organs
- The ascending colon extends from the right lower abdomen to the chest. The small intestine is usually located on the left side.
- In the right bend, the colon borders the liver and partially touches the right kidney.
- The colon is in contact with the liver and gallbladder.
- The left curve of the colon is slightly higher than the right, approximately at the level of the tenth rib. It borders the spleen and touches the left kidney.
- The small intestine is located on the right descending.
Abdominal organs
Vascular system of the colon
The large intestine is covered by branches of the superior mesenteric artery (iliac, middle and right colon). Arterial blood supply changes in the area of the left flexure of the colon. A change in innervation and blood supply occurs at the so-called Cannon point. The remaining parts of the intestine are supplied by the left colon and superior unpaired rectal artery, as well as 2-3 branches of the sigmoid arteries.
Vascular system of the colon
Nervous system of the colon
The movement of the colon is made possible by its plexuses in the intestinal wall. Sympathetic fibers reduce intestinal motility. Parasympathetic - increases. They come from the vagus nerve and are directed to the left flexure of the colon. At this moment, the parasympathetic nerve is innervated from the pelvic splanchnic nerves. This area is called Cannon's point, just like the blood supply.
Differences between large and small intestines
Macroscopically, the large intestine can be distinguished from the small intestine by circular protrusions of the colon wall, flat muscle thickenings and omental processes. At the microscopic level, the wall of the colon also has characteristics that differ from the small intestine. There are no villi in the colon, but there are crypts (0.4-0.6 mm long) with a large number of goblet cells.
Small and large intestine
Single lymphoid nodules are sometimes found on the wall. Most digestion occurs in the small intestine, where many nutrients are absorbed. In contrast, the colon is primarily where water is produced. The goblet cells secrete mucus, which serves as a lubricant for the stool produced.
Functions of the colon
This is interesting! The appendix is rich in lymphatic tissue and is an important component of the immune system.
Feces pass through the intestines over 12-48 hours by slow peristaltic movements and segmentation. Water is absorbed and the stool thickens. Every day, the large intestine absorbs from 0.5 to 2 liters of liquid. When absorbing water with a capacity of 5 to 6 liters, it is possible to compensate for its lack in the small intestine.
Large intestine - functions
Goblet cells, which are located in deep crypts, secrete mucins. The resulting mucus makes it easier for stool to pass through the intestines. Epithelial cells line the crypts with secretions and reabsorb electrolytes. The epithelial sodium channel (ENaC) regulates the reabsorption of sodium from stool. This process is controlled by the steroid hormone aldosterone. Potassium is released, which can be reabsorbed if there is a deficiency.
The acidic pH environment in the colon is 5.5-6.8, as a result of which it increases towards segments distant from the center.
In the rectum, stool is stored in such a way that excretion occurs only after it has accumulated in large quantities. Otherwise, the elimination process would be continuous.
Functions of the large intestine
Intestinal flora
Another feature of the colon is the diversity of colonizing bacteria. About 100 trillion mostly anaerobic organisms help digest some food components. In addition, they produce substances necessary for humans, such as vitamin K.
Attention! Sensitive intestinal flora may be disrupted by repeated antibiotic therapy. This, in turn, provokes diarrhea.
The role of intestinal microflora
Colon pathologies
Appendicitis
About 10% of the population suffers from appendicitis. Typically, inflammation is caused by obstruction of the cavity due to calcified feces, tumors, or foreign bodies.
Acute appendicitis may appear within a few hours. Initially, pain occurs in the umbilical region, and then in the right lower abdomen. In addition, nausea, vomiting and fever appear.
Inflammation of the appendix
The point on the right side of the abdomen is one third of the line connecting the superior anterior iliac spine to the umbilical cord. Pressure applied to this area can cause pain in patients with appendicitis.
A potential complication of advanced appendicitis is perforation of the peritoneal cavity and subsequent peritonitis, which can be life-threatening. In general, the only treatment is an appendectomy or removal of the appendix.
Irritable bowel syndrome
Irritable bowel syndrome is a group of intestinal diseases that are often not of organic origin. The etiology of the disorder is usually unclear. Symptoms include, but are not limited to, digestive problems accompanied by pain, diarrhea or constipation. Gluten sensitivity and psychological factors are also associated with irritable bowel syndrome.
Colon diverticulosis
Intestinal diverticulosis is a furry bulge of the wall or even the lining of the intestine. This is a kind of disease of civilization. Due to a low fiber diet, intestinal contents are transferred more slowly. The colon must contract more forcefully and therefore increase pressure.
Intestinal diverticulosis
Typically, these protrusions arise in the sigmoid colon. Diverticulosis is rare before the age of 30, and then the likelihood of its occurrence increases by 6-8% per year. The problem is difficult to detect due to the lack of symptoms. Possible complications include, but are not limited to, diverticulitis, bleeding, perforation, fistula and stenosis.
Intestinal inflammation
Inflammation in the colon is called colitis. There are acute inflammatory and chronic inflammatory bowel diseases.
Acute inflammation is also called enteritis. Ulcerative colitis is a chronic disease that occurs quite often. It involves inflammation of the intestinal tract that lasts for decades. The area of action of ulcerative colitis is limited to the colon and rectum.
Polyps in the colon
Polyps in the intestines
A polyp is an accumulation of tissue, either broad or flat, branched or polypoid. They are usually smaller than 1 cm and do not cause any symptoms. However, sometimes there is constipation, pain or blood in the stool. Especially large polyps can become malignant tumors and thus lead to colorectal carcinoma (adenocarcinoma).
Bowel cancer
A malignant tumor of the colon is called carcinoma. In most cases, it arises from still existing benign polyps of the adenoma-carcinoma sequence. Colon cancer is most common in the age group of 60 to 70 years.
Risk factors include advanced age, intestinal polyposis, genetic predisposition and ulcerative colitis. Diet plays a particularly important role. A diet high in fat increases the risk of cancer, while foods high in fiber reduce it. Therefore, bowel cancer is more common in industrialized countries.
Stages of bowel cancer
Symptoms, such as hidden bleeding, usually develop late. The prognosis usually depends on the stage of the cancer after discovery. It is determined according to the international classification of stages of malignant neoplasms (TNM). Lymphogenic metastases occur early, infecting regional lymph nodes. Hematogenously, colon carcinoma metastasizes predominantly to the liver, lungs and skeleton.
Bowel resection
Resection of the colon involves its partial removal. Indications include diverticulosis, polyps, carcinoma, or chronic inflammatory bowel disease such as ulcerative colitis.
Colon examination
Examination Image Description
| Percussion | Tympanic resonance can be heard |
| X-ray | Colon contrast enema |
| Colonoscopy | Performed using a flexible endoscope. Before the procedure, the patient received laxatives and saline solutions to cleanse the intestines. |
stomach-info.ru
Structure and functions of the large intestine
The large intestine is an organ that plays an important role in ensuring human life. First of all, it should be noted that this organ is a continuation of the small intestine. In order to maintain the body in a healthy state, it is worth understanding the peculiarities of the functioning of the organ in question.
About the structure of the large intestine
First, we should consider the structure of the large intestine. It is represented by the following segments:
- cecum;
- colon;
- straight.
The colonic part of the organ is divided into:
- ascending;
- transverse;
- descending;
- sigmoid.
All of the above sections are located to the right, left and below the small intestine in the abdominal cavity.
The cecum also has a vermiform appendix (located in the lower right part). The so-called bands lead from the process to the direct segment of the organ: free, mesenteric, omental.
The length can vary from 1.5 m to 2 m, depending on the characteristics of a particular human body. In diameter, its dimensions vary between 3.5-7 cm. The widest is the cecum. Then there is a gradual narrowing.
A characteristic feature of the organ in question is haustra (protrusion of the intestinal walls). Their formation is due to the fact that the ribbons are longer than the colon itself. There are also omental processes, which are also protrusions of layers of the wall containing fat. Their function is to protect the wall from infringement in areas of the organ. The structure of the wall of the colon is characterized by the presence of 3 membranes: mucous, muscular and serous. The first is absolutely devoid of any villi, it is smooth and has folds and glands. The second consists of longitudinal and circular layers. The third does not cover the entire length of the organ walls.
Return to contents
The anatomy of the colon is not as complicated as it might seem at first glance. The following information is subject to more detailed consideration: large intestine, departments. The initial section is the blind part of the organ, which is located on the right side of the abdominal cavity. Its width reaches 7 cm, and its length is 5-6 cm. A vermiform appendix extends from this section, the length of which is about 8 cm. It can be placed in different positions depending on the location of the blind part.
The ascending colon continues the cecum. It is located on the right and is directly adjacent to the wall of the abdominal cavity. Its continuation is the transverse colon part of the organ. Its length reaches 50 cm, it is in direct contact with organs such as the liver, stomach, gall bladder, pancreas, and spleen.
The descending colon is located on the left side of the abdominal cavity, followed by the sigmoid colon. It is usually shorter than the transverse one. The final section is the rectum, which ends near the anus. The end of this section is the anus. In general, its length varies from 13.5 to 19 cm. The organ is represented only by a muscle layer, which contains fibers arranged circularly and longitudinally. The lower part forms the anal canal (4 cm).
Return to contents
How does digestion occur in the large intestine? Digested food enters the large intestine, where water and mineral salts are absorbed. Remains of food that remained undigested at the previous stage end up here. Over the course of approximately 12 hours, all movements occur.
The human colon contains a large number of bacteria. The latter cause processes such as fermentation and rotting. Such bacteria do not harm the body provided they do not spread to other parts of the body. In the colon, bacteria produce vitamins K, B, hydrogen, hydrogen sulfide, carbon dioxide, and methane. Residues, including waste products and pigments, form fecal masses and are stored until removed.
The microflora of the colon is in dynamic equilibrium and determines the constant synthesis of a number of vitamins. If the composition of the microflora changes qualitatively and quantitatively, this causes the occurrence of dysbacteriosis. These reasons change the acidity of the environment, after which inflammatory processes develop.
The glands, which are a structural component of the organ in question, are designed to produce mucus. The latter contains enzymes in small quantities. This leads to better promotion of food. This mucus, formed in the colon, contains antibodies that protect the organ from disease.
Another important point worth considering is the blood supply to the colon. Its walls are enriched with blood and lymphatic vessels. The blood supply comes from the branches of the abdominal artery, as well as the inferior and superior mesenteric arteries. The outflow of blood from the organ occurs through the portal vein to the liver. Having summarized all the functions of the colon, we can highlight the main facts. One of the main functions is the implementation of final digestion. The colon converts masses into feces. The excretory system ensures that feces are released out through the rectum. The function of creating vitamins is also performed. It is worth mentioning the protective nature of the colon.
Return to contents
The most common disease of the colon is various types of infectious lesions. In developing countries, many people die from such diseases. The main symptoms are chills, diarrhea, fever, pain, and bleeding from the rectum. Inflammation can be caused by various microorganisms that provoke the development of ulcerative colitis and Crohn's disease. Treatment usually involves taking anti-inflammatory drugs.
Ulcerative colitis means damage to all parts of the organ. Accompanied by bleeding from the rectum. A person with this disease is at risk for developing colon cancer and must undergo regular examinations.
In Crohn's disease, the focus of inflammation develops directly in the organ itself. The transition zone between the small intestine and the large intestine may be affected. A characteristic feature of this disease is damage to the mucous membrane.
Chronic colitis of infectious origin occurs as a consequence of acute colitis. The main manifestation is alternating diarrhea with constipation. Otherwise, the picture of colitis depends on which part is affected. At the same time, all types of colitis lead to neuroticism, mental depression, and decreased productivity.
In the prevention of colitis, which is based on an infectious nature, compliance with the rules of personal hygiene plays an important role. Be sure to wash your hands before each meal, after visiting the restroom, and be sure to follow other generally accepted rules. The colon is most often affected by irritable bowel syndrome. This condition is the result of impaired intestinal motility. Accompanied by symptoms such as diarrhea, bloating, and abdominal pain. Treatment involves prescribing a special diet, and foods should contain a lot of fiber. The doctor prescribes medications to relieve spasms.
Colon cancer is common in developed countries. Causes may include inflammatory lesions and polyps. The disease is typical for older people. Symptoms are blood in the stool, diarrhea, abdominal pain.
Polyps are formations on the mucous membrane, resulting from the proliferation of the mucous membrane. Often cause bleeding from the rectum. This can lead to the development of malignant tumors.
Appendicitis is caused by inflammation of the appendix, which occurs most often in children. Features of the disease are acute pain in the lower right part of the abdominal cavity, loss of appetite, vomiting, nausea, fever. It can only be treated with surgery. If first aid is not provided in time, such a disease can be fatal.
Intestinal obstruction requires urgent surgical intervention. The processes that accompany the course of the disease are bloating, lack of stool, vomiting, dehydration, and severe pain in the abdominal area. At the first symptoms, you should immediately go to the hospital so as not to aggravate the process.
You should be careful about your body. By eating right, not forgetting to observe the rules of personal hygiene, and visiting a doctor for preventive purposes, you can protect your body for a long time.
Rate this article:
(No votes)
kishechnik03.ru
Large intestine in children and newborns
A child's colon is slightly more than 60 centimeters.
At the time of birth, the large intestine has not yet completed its formation, so the large intestine of a newborn baby has its own characteristics. A child's colon performs all the same functions as an adult's.
But initially, the baby’s colon does not have characteristic bulges and constrictions; it is smooth. There are no omental formations either. All this is formed in a child by about 2 years. The colon of a newborn baby is slightly more than 60 cm in length.
By the age of one year it increases by about 20 cm, and then equals the child’s height. The colon takes its final form by the age of 4 years. Different parts of the large intestine may develop unevenly.
The cecum eventually takes its usual position, but in infancy it is located high, under the liver. The appendix, which ends the cecum, in a small child is no more than 4 cm in size, and by the age of one year it already grows to 7 cm. Its position is difficult to determine accurately, since it is a fairly mobile appendage.
The cecum and appendix are not clearly separated from each other in infancy. The loops of the colon also increase as the child grows. The ascending part of the colon is the shortest (from 2 cm), it remains this way for up to a year, and then begins to grow.
The sigmoid colon in an adult is located below, in the pelvic area. In a child, the pelvis is not developed enough, so the sigmoid colon rises, located in the abdominal cavity. By the age of 5, the sigmoid colon takes its usual position. The inner layer of the colon is lined with epithelium containing various cells.
In a child, this epithelium is flatter. The epithelium contains crypts, that is, small tube-shaped depressions. The crypts inside are also lined with epithelial cells. The large intestine has more crypts, and in a newborn baby they are deeper.
The child's rectum also has its own anatomical features. In children, the rectum is not yet sufficiently curved and developed. Therefore, young children often suffer from rectal prolapse (much more often than adults).
Colon
Immediately after the cecum there is the next section, which is conventionally divided into 4 parts. The first of them - ascending - goes up the right side to the liver and ends in a smooth bend. The next subsection is the transverse colon. As its name suggests, it passes from right to left through the peritoneum. It also ends with a bend that turns into a descending part, running from top to bottom along the left side. The sigmoid colon (the last part of this section) is located in the left iliac fossa. It got its name from its S-shape.
Like other parts of the large intestine, this part is primarily responsible for the absorption of water and electrolytes and the formation of more solid contents from chyme. After the formation of a mass, colored dark by gall bladder enzymes and consisting of substances unnecessary for the body, exfoliated epithelium, etc., it moves on.