Duodenal ulcer is a chronic disease that is characterized by the presence of ulcers on the mucous membrane of the intestinal wall, vomiting, pain in the epigastric region after eating, and seasonal exacerbations (in spring and autumn). Has a tendency to relapse.
According to medical statistics, the pathology most often occurs in men aged 20–50 years.
Kinds
There are several classifications based on different characteristics. Pathology is classified according to a combination of the following signs:
- acute with bleeding;
- acute with perforation;
- acute with perforation and bleeding;
- acute without bleeding or perforation;
- chronic or unspecified form with bleeding;
- unspecified or chronic with perforation;
- unspecified or chronic with bleeding and perforation;
- unspecified or chronic without perforation and bleeding;
- unspecified, as acute, or chronic without bleeding and perforation.
By frequency of exacerbations:
- with rare exacerbations - acute symptoms occur no more than once a year;
- with frequent exacerbations - more than once a year.
By educational status:
- scarring;
- remission;
- active exacerbation.
Due to the occurrence:
- shock – occur as a result of burns, injuries;
- hormonal – appear after long-term use of hormonal drugs;
- stressful – develop due to depression and strong negative experiences.
According to the number of formations, multiple and single ulcers are distinguished, and according to the depth of the lesion - deep and superficial.
By localization, ulcers are determined in the post-bulb and bulbous (expanded part of the intestine) sections.
Treatment with folk remedies
Not only pills can treat ulcerative lesions; folk recipes play an important role in the healing of erosions. It is prohibited to use traditional medicine without first consulting your doctor.
Such recipes can be used not only as a preventive measure, but as a way to treat exacerbation of ulcers. Today there are many drugs known that are used for such purposes. They receive a lot of positive feedback daily. It is useful to drink rosehip decoction and herbal teas.
Recipe No. 1. Honey
3 tbsp. l. Melt honey in a glass of water. It is necessary to take the medicine 1.5 hours before a meal if the pH level is higher than normal, and 10 minutes before a meal if it is lower. If honey causes heartburn, you should take the medicine with milk.
Recipe No. 2. Sea buckthorn oil
Medicine with sea buckthorn oil is drunk on an empty stomach.
5 g of oil is mixed with ¼ cup of an aqueous solution of soda (2%). You need to drink the product for a month 3 times a day, half an hour before meals.
Recipe No. 3. Alcohol tincture of propolis
Dissolve 50 drops. tincture in 200 g of water and drink 60 minutes before meals for 3 weeks.
Recipe No. 4. Beet
A third of a glass of vegetable juice should be taken 3 times a day a third of an hour before meals. The course of treatment is 1.5 weeks.
Recipe No. 5. Potato
Complaints about ulcers will appear less and less if you drink potato juice. Before use, you need to prepare fresh medicine each time. You need to take it three times a day, 10 g, half an hour before meals. To prepare the product, you need to peel the potatoes and grate them, then squeeze out the juice.
Causes
Causes of duodenal ulcer development:
- Helicobacter Pylori infection.
- Increased acidity of gastric juice. Acid disrupts the integrity of the duodenal mucosa.
- Regular intake of non-steroidal anti-inflammatory drugs and hormones.
In addition to direct causes, there are factors that significantly increase the risk of pathology. These include:
- alcohol abuse;
- smoking;
- violation of diet and consumption of large amounts of unhealthy foods;
- binge eating;
- genetic predisposition;
- chronic duodenitis;
- heart and vascular diseases;
- congestion in the portal vein;
- contusion;
- abdominal injuries;
- extensive burns and frostbite;
- lesions of the spinal cord and brain;
- anemia, chlorosis and other blood diseases;
- frequent chemical or thermal strokes;
- disorders of the immune system;
- chronic intoxication;
- psycho-emotional instability;
- syphilis;
- disruption of hormone production (enterogastron, gastrin, secretin);
- consequences of surgical operations (appendectomy, amputation of limbs);
- working the night shift (increases the likelihood of developing the disease by 50%).
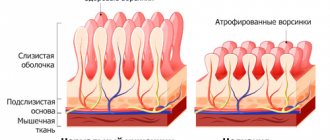
Disorders leading to increased secretion of pepsins, hydrochloric acid, decreased production of mucous substances, and impaired motility of the gastroduodenal zone occur for various reasons. These include changes in the autonomic and central nervous systems - they can provoke the formation of ulcers on the surface of the walls, since as a result of their occurrence, the balance between aggressive factors and the body’s defenses is disrupted.
Causes of duodenal ulcer
In the overwhelming majority of cases, duodenal ulcers occur due to exposure to the previously noted bacterium Helicobacter Pylori. The peculiarities of its vital processes occur not only with the production of substances that damage the mucous membrane of the duodenum and stomach, but also with the production of ammonia, which, in turn, leads to increased production of hydrochloric acid by the body.
Until relatively recently, the bacterium Helicobacter pylori was considered exclusively the causative agent of gastritis (its chronic form), but later its role in the occurrence and development of gastric ulcers and, accordingly, duodenal ulcers was proven. Considering this fact, treatment of a duodenal ulcer cannot be called adequate if it is not focused on appropriate measures to destroy this bacterium.
In addition to the previously noted smoking, alcohol, use of certain medications and other factors, heredity cannot be ruled out as possible precursors to the onset of this disease in the future. Statistics indicate that the presence of an ulcer in parents determines their child’s predisposition to it in the order of 40%.
As for the causes of relapses of peptic ulcer disease in the area under consideration, bleeding can be identified as such, as well as the patient’s violation of the instructions that the doctor has determined for him.
Symptoms
The signs of an ulcer are similar to many of the symptoms that occur with other pathologies of the gastrointestinal tract.
Symptoms of duodenal ulcer:
- bloating and flatulence;
- belching;
- nausea;
- feeling hungry several hours after eating;
- sharp, piercing pain below the sternum, in the upper abdomen, which can radiate to the heart and back;
- disappearance of pain immediately after eating;
- sleep disturbance due to pain at night;
- weight loss regardless of food intake and calorie content;
- chronic vomiting of blood, which can be fatal.
Cases of asymptomatic disease have been recorded. This form of ulcer most often develops in elderly patients.
With timely diagnosis, relief of exacerbations, and adherence to diet, the prognosis is favorable. It is possible to achieve long-term remission and scarring of the ulcer.
The discomfort that the patient complains about is the reason for conducting a detailed examination and comparing the data obtained with the described symptoms of duodenal ulcer.
Duodenal ulcer with bleeding: symptoms
Returning to the characteristics of the types of duodenal ulcers, I would like to dwell on perforated ulcers and ulcers with bleeding. First, let's look at the symptoms of a bleeding ulcer and, in particular, what it is.
In case of a duodenal ulcer, the development of bleeding is provoked by the formation of neutrophic lesions in the area of the walls of this organ, as well as hypovitaminosis K, P and C, mental and physical stress, vascular damage against the background of atherosclerosis in the gastroduodenal area, trauma and abdomen, etc. As for statistical data Regarding the prevalence of such a manifestation as bleeding during duodenal ulcer, there are certain discrepancies on this score - in some sources the data is reduced to 4.4%, in others it reaches 37% or more.
Complications of ulcers by bleeding are primarily observed in men; for the most part they occur in people 40-50 years old. Mortality due to such bleeding is still more than high to this day, reaching about 1-24% in various countries and ages, and most often such an outcome is observed in people 45 years of age.
It should also be noted that the patient’s previous bleeding puts him at greater risk of re-bleeding; predicting possible risks against this background is not possible. An extremely severe complication of duodenal ulcer disease is early recurrent bleeding, which occurs within the first six weeks from the end of the acute previous bleeding. Accordingly, late recurrent bleeding occurs already after 6 weeks from the moment of such previous bleeding.
Early recurrent bleeding indicates a fairly high mortality rate, and this is true even if the patient undergoes emergency surgery. The risk of death increases with each subsequent bleeding, and their prediction is also impossible.
Peculiarities of bleeding in patients with duodenal ulcers:
- Sudden massive bleeding . Indicates another exacerbation.
- Minor bleeding . As a rule, it occurs as a result of excessive use of medications that are contraindicated for use. A small ulcer can bleed almost daily; blood loss occurs in the patient’s stool (without changing its color to black). In this case, the only symptom is often severe fatigue, not dictated by anything.
The clinical picture that accompanies massive ulcerative bleeding has quite characteristic symptoms. So, this includes loose black stools, nausea and slight chills, some cases indicate fainting after or during bowel movements.
When blood loss exceeds 350 ml, its total volume decreases, therefore, corresponding compensatory reactions arise in the form of vascular spasm, a rapid drop in blood pressure, and pallor. If an ECG is performed, myocardial hypoxia may be detected.
As a result of massive bleeding, vascular collapse quickly develops, which, in turn, is accompanied by dizziness and weakness of the patient, pallor, low blood pressure, and tachycardia. The temperature is low-grade (37.5-38°C), pain may cease.
Vomiting of blood is accompanied by the release of dark clots, which is explained by the effect of hydrochloric acid from the stomach on hemoglobin.
It is noteworthy that before tarry stools with bloody vomiting, internal bleeding can also be determined based on its general signs (which is possible in the absence of severe cardiovascular diseases in the patient). Thus, gastroduodenal bleeding is not accompanied by characteristic muscle tension in the abdominal area, or other pronounced symptoms indicating irritation of the peritoneum. When conducting tests, a decrease in the number of red blood cells, hematocrit and hemoglobin levels is determined.
The prognosis of duodenal ulcer is often quite difficult, especially when bloody vomiting appears along with tarry black stools.
The nature of the pain before and after bleeding also determines its significance in the prognosis; the age of the patient is not overlooked. For example, an erosive artery that has hardened and lost its inherent elasticity, which has also undergone sclerotic changes, loses the ability to contract (which is important for elderly patients); accordingly, the chances of stopping bleeding are significantly reduced, even if conservative therapy methods are used.
It should also be noted that abdominal pain, which is so debilitating for the patient before bleeding, often disappears after it. If this does not happen, then the prognosis, accordingly, worsens. The fact is that here we are talking about a callous or penetrating ulcer; each of these ulcers, in turn, determines the insignificant chances of the bleeding ending on its own or of a positive result in stopping it using biological or chemical therapy.
Diagnostics
For diagnosis, a complex of laboratory and instrumental studies is used, which make it possible to determine the pathology, its form and degree of development, and accurately determine the location.
The following methods are used to identify ulcers:
- Endoscopy is the most informative method. Allows you to obtain extensive information about the condition of the mucous membranes, including sampling of tissues and stomach contents for laboratory analysis.
- Test for the presence of Helicobacter Pylori. It is carried out on the basis of material taken from the patient during endoscopy, or feces, vomit, and blood are examined. Breath test.
- Ultrasound examination of the abdominal cavity.
- Palpation.
- Antroduodenal manometry.
- Fecal blood test (Gregersen test), general blood and urine test, biochemical blood test, gastric juice analysis to determine the level of acidity, histological analysis of the material to determine the malignant nature of the formation.
- X-ray examination using barium suspension.
- Electrogastroenterography.
Differential diagnosis:
- granulomatous enteritis (Crohn's disease);
- stomach ulcer;
- cholelithiasis;
- symptomatic ulcers;
- non-ulcer dyspepsia;
- gastrinoma (Zollinger-Ellison syndrome).
Associated pathologies:
- chronic renal failure;
- cirrhosis of the liver;
- reactive pancreatitis;
- chronic cholecystitis;
- Wermer's syndrome.
Treatment
Dietary nutrition is important. The patient must always comply with the restrictions, but doctors also allow a zigzag regime, when a strict diet is needed only during the months of exacerbation - in spring and autumn. The rest of the time, it is allowed to eat foods not from the dietary list.
Taking medications is necessary during periods of exacerbation.
For the treatment of duodenal ulcer, the following groups of drugs are used:
- Antibiotics – to eliminate pathogenic bacteria.
- Antacids - to reduce the acidity of gastric juice.
- Antisecretory drugs - to reduce the level of gastric juice produced.
- Antispasmodics – to relieve pain.
Exacerbation of ulcers is treated in a hospital setting. The course takes on average from 2 to 5 weeks, depending on the pathology’s response to therapy.
Surgery is usually required only if there is associated bleeding or a perforated ulcer. In other cases, drug treatment during periods of exacerbation and dietary nutrition are sufficient.
Treatment of duodenal ulcers
The treatment of the disease in question is determined comprehensively, based on the general condition of the patient, laboratory data and a number of other conditions; accordingly, the definition of specific treatment options in our article is inappropriate due to their exceptional complexity and extreme individuality in selection.
Let us only note that surgical treatment, once so popular in the fight against ulcers, is today carried out only in cases of bleeding or perforated ulcers. As for pharmacological therapy, it is focused on destroying the bacterium Helicobacter pylori, restoring the mucous membrane of the affected organ and preventing complications due to this disease. The main drugs used in treatment include Omez and De Nol, as well as some antibiotics.
To diagnose a duodenal ulcer if the listed symptoms are relevant for the patient, you must contact a gastroenterologist. The occurrence of critical conditions (severe pain, bloody vomiting) requires an immediate call for an ambulance.
What to do?
If you think you have a duodenal ulcer
and symptoms characteristic of this disease, then a gastroenterologist can help you.
Source
Did you like the article? Share with friends on social networks:
Complications
- Perforation of an ulcer is a rupture of the intestinal wall at the location of the wound. Occurs after physical activity or overeating. Accompanied by very sharp stabbing pains, vomiting, nausea, abdominal muscle tension, cold sweat and rapid heartbeat.
- Chronic duodenitis.
- Ulcer malignancy.
- Narrowing of the intestine due to scar tissue.
- Peritonitis is inflammation of the peritoneum due to perforation of an ulcer.
- Bleeding. Manifested by vomiting like coffee grounds, dark feces.
In the absence of treatment for duodenal ulcer, the pathology becomes a dangerous disease that can lead to death as a result of peritonitis, bleeding or the development of an oncological tumor.
general description
Duodenal ulcer is much more common than in other organs of the gastrointestinal tract. It is more typical for city dwellers, due to the rhythm of life, eating habits and stress. Damage to the duodenum occurs more often in men. Pathogenesis is associated with Helicobacter, bad habits and psychosomatics.
The disease often recurs, especially if the ulcers spread to the stomach. The disease manifests itself as painful sensations in the epigastrium, which are characterized by cyclicity. It occurs with exacerbations and remissions. If the peptic ulcer is in an advanced state, or the ulcer is poorly healed, it may be accompanied by bleeding, perforation and other complications.
Usually, ulcers do not appear singly; they tend to come in pairs. Code ICD-10, K26.
Features of duodenal ulcer in children
Duodenal ulcers in children can be detected as early as 5–6 years of age. The causes of the pathology are the action of Helicobacter Pylori, psycho-emotional factors and genetic predisposition.
The symptoms do not differ from the signs of the disease in adults, but diagnosis is complicated by the fact that the child, as a rule, cannot explain his feelings. It is typical that children often try to take a comfortable position to relieve pain - pressing their legs to their stomach while sitting or lying on their side.
The disease is also dangerous when it is latent. The lack of discomfort allows the ulcer to progress without proper treatment. A detailed examination of the child can reveal the following signs:
- moderately severe chronic intoxication;
- hypovitaminosis;
- white coating on the tongue;
- pain when palpating the abdomen in the upper part and right hypochondrium.
For diagnosis in children, the method of gastrofibroduodenoscopy is used, and treatment is based on pain relief in the acute period with the help of antispasmodics, antibiotic therapy and dietary nutrition.
Perforated duodenal ulcer: symptoms
A perforated duodenal ulcer is an extremely serious complication of this disease; its development occurs as a result of the formation of a through defect in the wall of the organ in question, opening into the abdominal cavity or into the retroperitoneal space.
Most often, perforation of an ulcer is observed among men, and their age mainly falls within the age category from 20 to 40 years, although in general this manifestation is not excluded among patients representing other age groups.
Diagnosis of this condition is quite difficult in some cases. For example, if we are talking about a covered perforation or perforation to the area of the omental bursa. Such difficulties are also relevant when trying to establish a diagnosis in elderly patients and patients in a weakened state.
Mostly perforation of an ulcer is the result of a long course of peptic ulcer disease; about 10% of cases are perforation of the so-called “silent” ulcer, most often observed in young patients, as well as in the elderly. Perforation and its symptoms, in particular, can develop against the background of bleeding from a peptic ulcer, which, accordingly, turns the doctor’s attention to the latter manifestation.
The symptoms of a perforated ulcer determine a separate classification:
- Etiology. Depending on the characteristics of the etiology, chronic perforation or acute symptomatic perforation (stress, hormonal, etc.) is determined.
- Localization. Bulbar or postbulbar.
- Clinical form. 1) perforation to the abdominal cavity (covered and typical perforation); 2) atypical perforation (to the omental bursa, to the greater or lesser omentum); 3) combined perforation, occurring in combination with bleeding in the gastrointestinal tract.
- Clinical periods. Corresponds to the peritonitis phase (primary shock, imaginary well-being, severe abdominal sepsis).
There are three stages of the course of this disease, that is, clinical periods noted in the classification:
- Stage I. This is the stage of shock, which occurs in the first 6 hours. It is characterized by symptoms in the form of sharp pain in the epigastric region, similar to the “strike of a dagger,” vomiting at the very beginning, and immobility of the patient. In frequent cases, patients are in a position with their legs brought up to their stomach. There is pallor of the skin and slight cyanosis (blueness) of the lips, shallow breathing, and cold sweat. The pulse at this stage is either normal or slightly low, and blood pressure is also low. When tapping the abdominal area, sharp pain is noted. Palpation determines the tension in the buttocks area, the stomach becomes rigid, which reveals an analogy with a board.
- Stage II. This stage is characterized by an imaginary improvement. Its onset occurs within the next 6 hours from the completion of the previous stage. As can be understood from the initial characteristics, the patient’s condition stabilizes somewhat within this stage, pain decreases, muscle tension subsides, which allows us to judge a general improvement. Here it is important to pay attention to the symptoms indicating the development of peritonitis, which consists of the phenomena of tachycardia and euphoria, dry tongue and increased temperature, possible retention of gases and stool due to paresis, which is relevant for the intestines. Leukocytosis, which was not present in the first stage, gradually increases in this stage. Palpation determines the greatest degree of pain on the part of the iliac region (on the right); as a result, the patient’s condition may be misinterpreted and diagnosed against the background of such manifestations of acute appendicitis.
- III . It develops about 12 hours after the completion of the previous stage; this stage corresponds to the pronounced clinical manifestations of diffuse peritonitis. Establishing the cause that became the initial factor in the development of the disease is significantly complicated; for this, it is necessary to rely in conjunction on the entire anamnesis collected on the patient’s condition. His condition at this stage of the disease is rapidly deteriorating. The first symptom indicating this stage is vomiting, which is systematically repeated and leads to gradual dehydration of the patient and loss of strength. The patient's restlessness, dry mucous membranes and skin are noted. The temperature rises, the pressure drops, the pulse reaches 120 beats per minute. Breathing becomes rapid. Again, bloating occurs. The tongue becomes dry and a dirty brown coating appears on it. Determining the diagnosis, as well as providing surgical care, become not only belated actions, but also, one might say, useless.
Features of duodenal ulcer in pregnant women
The pathology worsens most often in the first and third trimesters of pregnancy. Stopping an exacerbation is an important point in pregnancy management, since the disease can lead to serious consequences - the risk of complications in the expectant mother increases.
Diagnosis and treatment are complicated by the fact that pregnancy limits the number of methods used. X-ray diagnostics are contraindicated, as is the use of many medications.
Treatment of exacerbations in pregnant women:
- bed rest;
- fractional meals (small portions 3–6 times a day);
- diet 1–1b according to Pevzner;
- mineral water;
- enzyme preparations (to eliminate bloating).
Women who have suffered an exacerbation of the disease during pregnancy are given preventive treatment 2-3 weeks before the expected date of delivery.
Treatment of peptic ulcer
Treatment of duodenal ulcers most often does not cause difficulties; a complex therapy regimen is used, which includes:
Elimination of duodenal ulcer depends on the nature of the disease.
- treatment aimed at destroying Helicobacter and inhibiting the secretion of gastric juice;
- relief of symptoms of the disease;
- quitting smoking and other factors that adversely affect the digestive organs or cause increased secretion of hydrochloric acid;
- dietary nutrition, which is aimed at reducing the load on the gastrointestinal tract, eliminating food irritants from the menu, etc.;
- arrangement of daily routine and food intake;
- avoiding stressful situations and severe overwork (they lead to neuroses, and, therefore, affect the functioning of the autonomic nervous system, which aggravates the problem);
- giving up alcohol;
- Sometimes surgical treatment is needed.
Treatment regimen and diet
It is impossible to treat an ulcer without a diet. The most strict diet is during an exacerbation, when a chronic ulcer makes itself felt with pain and other unpleasant symptoms. The patient should eat only food that will have a gentle effect on the duodenum, which means that only mechanically, thermally and chemically gentle food is allowed.
The meal schedule should be put in order. You need to eat small portions at the same time 6 times a day. The optimal temperature for the dish is 36-37 degrees. Cold and hot foods irritate the intestines. You should not eat on the go, especially dry snacks.
If you get sick, you need to give up bad habits
Alcohol is strictly prohibited. You should stop smoking. Experienced smokers sometimes cannot completely give up this bad habit. In this case, it is recommended to quit smoking on an empty stomach.
Food must be steamed or boiled. During the period of exacerbation of peptic ulcer disease, mucous soups, mashed boiled vegetables, and porridge are recommended for consumption. Later, you can eat lean meats and fish in a pureed state. It is possible to use soufflé or steam cutlets.
You should not eat fried, spicy, salty, fatty, smoked foods, marinades, or canned food. Caffeine-containing drinks should not be drunk, especially if you have pain. Rosehip has healing and soothing properties, so a rosehip decoction will be useful.
During the period of remission of an ulcer, you can eat vegetables and fruits, which are high in fiber, which should not be done during the period of healing of ulcers. Such products include apples, tomatoes, cabbage, cucumbers, etc.
The health effects of milk are controversial in peptic ulcer disease, as its beneficial and detrimental effects are known. Remission allows you to diversify your diet a little.
Drug therapy
Duodenal ulcers require taking pills that block stomach acid and heal the affected areas.
Questions rarely arise with diet; almost everyone knows what is harmful to the digestive system. Many are still more interested in how to treat duodenal ulcers. Treatment of the disease is complex. It is aimed at relieving pain, eliminating inflammation, normalizing the secretion of enzymes, etc.
Today there are two schemes that determine that an ulcer is treated with three or four components. They will permanently eliminate the problem caused by ulcerations of the duodenal mucosa caused by Helicobacter. These two regimens will help not only cure the ulcer and relieve pain, but also avoid the consequences.
Each regimen uses antibacterial drugs (two different ones at once) together with an antiprotozoal substance, which is indicated to be taken for 1-1.5 weeks if the patient is diagnosed with Helicobacter. This will relieve inflammation.
The patient is prescribed drugs that inhibit the secretion of hydrochloric acid by the stomach - histamine receptor blockers and proton pump inhibitors. It is necessary to take a course of antacids; they neutralize gastric juice, reducing the impact of an aggressive environment. This medicine should be taken if your stomach or intestines hurt, and not as a course. For pain, it is recommended to use antispasmodics (for example, No-shpa tablets).
Physiotherapy
You can use hardware to treat attacks of pain from duodenal ulcers.
Today, medicine offers treatment of duodenal ulcers with physiotherapeutic procedures, which enhance the effects of drug therapy. During an attack of an ulcer, the following methods are used:
- microwave therapy;
- ultrasound treatment;
- sinusoidal modulated current;
- electrophoresis using pharmaceuticals (for example, papaverine);
- heat therapy (alcohol compress, which can be done at home).
This helps relieve pain, overcome inflammation, improves blood flow in the gastrointestinal tract, etc.
Physiotherapy
Exercise therapy is useful for normalizing the production of enzymatic juice in the gastrointestinal tract, improving peristalsis in the duodenum, and accelerating blood flow. Exercise therapy is used for preventive purposes, as it helps to avoid congestion in the stomach and intestines, which is especially important for bedridden or temporarily bedridden patients.
Do not neglect therapeutic physical exercises to improve health after suffering a duodenal ulcer.
Physical therapy is recommended after the exacerbation has been cured (nothing hurts, blood tests are normal, there is no blood in the stool). At this time, the person may also be advised to remain in bed, so gymnastics is initially performed in bed at a slow pace. It is important to learn how to breathe correctly when doing exercises and do as many approaches as is comfortable. Exercise therapy slightly increases intra-abdominal pressure, which improves organ performance.
When the patient can no longer stay only in bed, the range of exercises expands, and sitting and standing exercises are introduced. In exercise therapy it is allowed to use dumbbells weighing up to 2 kg. The pace of the exercises is accelerated as much as possible. Walking is added to exercise therapy (up to 3 km on steps). It is better to do gymnastics in the morning.
Use of mineral waters (at the resort and outside the resort)
It is recommended that a person with an ulcer take mineral water 60-90 minutes before meals. If ulcer healing does not occur for a long time in patients over 40 years of age, they are recommended to drink water half an hour before meals.
During an exacerbation, treating an ulcer with mineral water is contraindicated.
The water should be 38-40 degrees, so it needs to be heated at home. Low-mineral waters are indicated for use (for example, Borjomi, Essentuki, Jermuk, etc.). At the resort, baths with mineral waters are prescribed; they help with pain and normalize the activity of the nervous system, which will speed up recovery, which is due to the fact that the psychosomatics of ulcers is a fairly common occurrence.
Surgery
Surgical treatment methods are used if ulcer bleeding, perforation occurs, pyloric stenosis occurs (a healed ulcer blocks the passage) and other complications that are dangerous to the life and health of the patient and cannot be treated with medication.
When a benign ulcer is diagnosed, surgical intervention is sometimes necessary - if the scar does not form for more than 4 months with adequate drug treatment.
There are 2 types of operations that are carried out in such situations:
Surgery of the duodenum is necessary in cases of frequent bleeding and dangerous complications.
- resection;
- vagotomy.
Resection is the excision of part of an organ, in which the remaining area is sutured to a further organ.
Vagotomy is the cutting of the nerve endings that lead to the stomach and stimulate the secretion of hydrochloric acid, which is why the remission of the ulcer is not long-lasting.
Laparotomy surgery is performed as a vagotomy with gastric drainage or as a proximal selective vagotomy. The latter method is more often used today, but it is technically more difficult.
Features of duodenal ulcer in elderly people
According to studies, treatment of ulcers in elderly patients requires a lower dosage.
Surgery is usually required only if there is associated bleeding or a perforated ulcer. In other cases, drug treatment during periods of exacerbation and dietary nutrition are sufficient.
When developing a treatment regimen for older and elderly patients, this feature must be taken into account in order to minimize the intake of medications and facilitate their removal from the body.
Forecast
With timely diagnosis, relief of exacerbations, and adherence to diet, the prognosis is favorable. It is possible to achieve long-term remission and scarring of the ulcer.
Prognosis for different patient groups:
- Elderly patients: the highest percentage of deaths due to complications occurs - callous ulcers, bleeding.
- Juvenile ulcers: the pathology is prone to frequent relapses. The prognosis for recovery is unfavorable.
- Women of childbearing age: high chances of recovery.
The prognosis largely depends on concomitant diseases, household and professional conditions, the location of the ulcer and the characteristics of the clinical course of the disease.
Complications and consequences of duodenal ulcer
It is not always necessary to treat an ulcer; sometimes scars form on their own, but more often the disease worsens, which is fraught with the development of complications that are dangerous to health and life. Complications can be classified into:
- destructive;
- dysmorphic.
Destructive
Complications of the destructive type are violations of the integrity of the intestinal walls, as a result of which the following can develop:
- bleeding;
- perforations;
- penetration.