Tubulointpersitial (or interstitial) nephritis
called inflammation and damage to the tubules and interstitial tissue of the kidneys with relative safety of the glomeruli and blood vessels. There are not only primary forms of acute and chronic interstitial nephritis, but also its secondary forms with primary damage to the glomeruli and in systemic diseases.
The main distinguishing features of acute tubulointerstitial nephritis
are lymphocytic infiltration of interstitial tissue, edema and tubular damage. Eosinophils may be present in the infiltrates, especially in drug-induced tubulointerstitial nephritis, and sometimes granulomas. The pathogenesis is not fully understood. The involvement of T-cell immune mechanisms has been postulated. Causing agents include medications, especially antimicrobials, anticonvulsants, and anticonvulsants, as well as infections, primary glomerular diseases, and systemic diseases (eg, SLE).
Clinical manifestations of acute tubulointerstitial nephritis
. Classic signs of tubulointerstitial nephritis are fever, rash, and arthralgia associated with elevated serum creatinine levels. However, this typical triad of manifestations does not occur in all patients. The rash is often transient and varies in appearance, from maculopapular to urticaria. Nonspecific symptoms are common: nausea, vomiting, weakness, weight loss. Enlargement of the kidneys, leading to stretching of the renal capsule, usually causes pain in the lumbar region.
For acute tubulointerstitial nephritis
- complications of other diseases (for example, SLE) - specific signs of the underlying disease are usually observed.
In contrast to glomerular lesions, which are characterized by acute renal failure with oliguria, oliguria is absent in 30-40% of patients with acute tubulointerstitial nephritis. In drug-induced nephritis, peripheral eosinophilia is observed. In all cases, microhematuria of varying degrees occurs, but macrohematuria or proteinuria, as a rule, is absent. The exception is patients with nephritis caused by NSAIDs, in whom nephrotic syndrome is possible. The urine contains leukocytes and granular casts
, but red blood cell casts, characteristic of glomerular diseases, are rarely observed. The presence of eosinophils in the urine is not a specific sign.
Diagnosis of acute tubulointerstitial nephritis
. The diagnosis is made based on the clinical picture and laboratory data. It is extremely important to find out the time dependence of the onset of the disease on the use of certain medications. Since immune mechanisms are involved in the pathogenesis of tubulointerstitial nephritis, its signs and symptoms usually appear after 1-2 weeks. After exposure to drugs. In children, the cause of the disease is often antimicrobial drugs, as well as NSAIDs.
Urinalysis should be performed periodically and creatinine
and electrolytes in blood serum. Ultrasound of the kidneys does not have diagnostic value, but it can detect their enlargement and increased echogenicity. Improvement in renal function after eliminating all possible causative factors provides convincing evidence of the correctness of the diagnosis; further testing is usually not required.
In more complex cases, when the reason
remains unclear or the patient's renal function is rapidly deteriorating, a kidney biopsy is indicated. Treatment and prognosis. Symptomatic treatment is aimed at eliminating complications of acute renal failure, such as hyperkalemia and volume overload. Some data indicate the effectiveness of corticosteroids in severe renal impairment. In case of rapid spontaneous improvement, the prognosis is very favorable. However, in patients with long-term renal failure, the prognosis is unclear. Severe acute tubulointerstitial nephritis of any origin often becomes chronic.
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan) Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2010 (Order No. 239)
October 24-25, Kazakhstan, Nur-Sultan
New venue! Astana-EXPO territory, pavilion C3.5
Get a free ticket
International Healthcare Exhibition
October 24-25, Kazakhstan, Nur-Sultan
New venue! Astana-EXPO territory, pavilion C3.5
Get a free ticket
general information
Short description
Protocol “Acute tubulointerstitial nephritis in children”
ICD-10 codes: N10 Acute tubulointerstitial nephritis
October 17-19, Almaty, Atakent
200 participating companies, seminars and master classes, discounts, prize draws
Get an invitation card
October 17-19, Almaty, Atakent
200 participating companies, seminars and master classes, discounts, prize draws
Get an invitation card
Treatment
Treatment tactics
Treatment goals: elimination or reduction of microbial inflammatory process in the renal tissue and urinary tract.
Symptomatic therapy – correction of arterial hypertension, homeostasis disorders, anemia.
Diuretic, nephroprotective therapy.
Non-drug treatment: diet No. 7, protective regimen.
Drug therapy
Medicinal nephritis requires the abolition of medications - the causes of the disease, drinking plenty of fluids, and a gentle diet. Bacterial acute tubulointerstitial nephritis is fully consistent with acute pyelonephritis. “Starting” antibacterial therapy is prescribed empirically, since urine culture and sensitivity determination take time, and the start of therapy cannot be delayed. Preference is given to “protected” penicillins; correction is carried out taking into account the data obtained on the nature of the microbial flora and the sensitivity of the drug to it.
“Protected” penicillins (A) (augmentin, amoxiclav) – 375 mg for 7-10 days; amoxicillin 30 mg/kg/day. (up to 60 mg/kg) – 2-3 times a day.
Ampicillin 100-200 mc/kg/day. up to 3 years; 50-100 mg/kg/day. children over 3 years old.
2nd generation CF (B) – teclor: 20-40 mg/kg/day, taken 3 times a day; cefuroxime axetil (zinnate) – 125-250 mg orally 2 times a day.
3rd generation CF (B) (cedex) – 9 mg/kg/day once.
Nitrofurans (B) (furagin) – 5-8 mg/kg body weight per day, 3-4 times a day.
Causes
Tubulointerstitial kidney damage occurs for several reasons:
- infections;
- long-term use of medications (NSAIDs, diuretics, analgesics, antibiotics, probiotics);
- poisoning by toxins;
- radiation exposure;
- allergic reaction to medications taken;
- severe systemic diseases, for example, arterial hypertension, pyelonephritis, nephropathy, leptospirosis, hepatitis, diphtheria;
- unfavorable environmental conditions (polluted air, water, soil);
- cancerous tumors;
- heredity;
- immune diseases.
Causes of tubulointerstitial nephritis in patients
The acute form of this kind of disease affects the kidneys most often after a long course of use of antibiotics or other types of anti-inflammatory drugs; cases of an acute form of the disease occurring after poisoning with heavy metals, chemicals, and ethanol are no less rare.
Chronic tubulointerstitial nephritis may well result from the severe course of the acute form of this disease, but these are rare cases. The most common causes are infections, serious metabolic disorders, and severe drug intoxication.
Symptoms and types
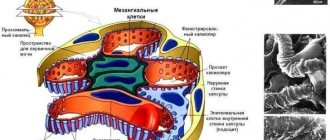
A feature of the disease is that the inflammatory process develops in the renal tubules, interstitium and renal tissue. The pyelocaliceal structure is not affected. First, swelling of the tubular epithelium is detected, then dystrophic changes occur, resulting in tissue necrosis.
Classification of interstitial nephritis according to the etiology of its appearance:
- Primary. The disease is independent; its appearance is not preceded by other pathologies.
- Secondary. Nephritis is a complication of other diseases, for example, diabetes, leukemia.
According to the nature of the flow, they are distinguished:
- Spicy. This form can manifest itself not only in adult patients, but even in children. Acute interstitial nephritis in 95% of cases develops after an infectious disease, less often it is the result of toxic effects. The inflammatory process involves the renal tubules, blood vessels and lymph. The disease occurs in a severe form, and if not treated in a timely manner, chronic renal failure develops.
- Chronic. The disease develops as a result of previous infectious diseases, metabolic disorders, and medications. In children, chronic interstitial nephritis is more common than its acute form. The onset of the disease is long; the appearance of pronounced symptoms is preceded by a long latent period. Tubular atrophy and thickening of the basement membranes occurs over several years.
Chronic and acute tubulointerstitial nephritis in children and adults: causes, symptoms, treatment
Tubulointerstitial nephritis (TIN) is a kidney pathology that affects the interstitium, the epithelial lining of the tubules, and blood vessels.
Tubulointerstitial nephritis
With TIN, changes in the interstitium are noted, the functioning of the tubules is disrupted, but the functions of the glomeruli are preserved. According to the International Classification ICD-10, tubulointerstitial nephritis belongs to diseases of the genitourinary system with code N10 - N 16.
In adults, drug damage is a common cause of TIN, especially in women over 40 years of age. The incidence of analgesics among people of working age of both sexes suffering from TIN is 65%.
Children are characterized by vesicoureteral reflux, which disappears as they grow older.
Children are more likely to suffer from infectious bacterial TIC - acute pyelonephritis. The peak of pyelonephritis in children occurs at the age of 3 years; mostly girls are affected, the ratio is compared to boys.
Adults mainly suffer from pyelonephritis after 60 years of age, and this disease often occurs in women 20-35 years old. Risk factors for TIN include:
- taking antibiotics, analgesics, non-steroidal anti-inflammatory drugs, warfarin, mesalazine, ranitidine, cimetidine, thiazide diuretics, captopril, carbamazepine;
- caffeine consumption;
- diabetes;
- cirrhosis of the liver;
- heart pathologies.
Definition of tubulointerstitial nephritis
Kinds
Tubulointerstitial nephritis is distinguished according to the nature of its course:
Tubulointerstitial nephritis develops as:
- primary - occurs under the influence of a damaging agent, which are some drugs, including medicinal plants, toxins, metabolic disorders;
- secondary – caused by chronic glomerulonephritis, amyloidosis, radiation nephritis, nephroangiosclerosis.
Tubulointercystial nephritis is classified according to the nature of the damaging agent.
Infectious
- Spicy;
- acute with systemic lesions;
- chronic, which includes bacterial pyelonephritis, pathologies caused by hepatitis B and C viruses;
- specific.
Drug
Medicines, both synthetic and herbal of natural origin, can affect kidney tissue, causing irreversible damage.
Tubulointerstitial nephritis of drug origin occurs in acute, hypersensitive, and chronic forms.
TIN develops when the immune system malfunctions in the following forms:
- hypersensitive delayed type;
- hypersensitive immediate type;
- caused by Sjögren's syndrome, sarcoidosis;
- caused by AT (antibodies) against AG (antigens) of the collecting ducts;
- stimulated by antigen-antibody complexes.
The immunoallergic type of development of TIN is most typical for childhood.
For metabolic disorders
- Hypercalcemic;
- hyperkalemic;
- urate.
Types of TIN also include:
- obstructive nephropathy;
- dysplastic, caused by congenital pathologies of the parenchyma;
- tumor caused by myeloma, lymphoma, hemoblastosis;
- reflux nephropathy;
- caused by heavy metals - lead, cadmium.
The disease is often diagnosed already in the chronic phase. Statistically, all types of nephritis are distributed: medicinal - more than 60%, bacterial - more than 14%, obstructive - more than 10%, 8% - of unknown etiology, 3% - under the influence of exogenous toxins.
Hereditary forms of TIN that arise from mutations in the mucin-1 gene are diagnosed.
Pathogenesis
TIN is characterized by swelling of the interstitial tissue of the renal parenchyma and necrosis of the tubules. In the chronic course of tubulointerstitial nephritis, foci of necrosis occupy a large area.
TIN is characterized by:
- increased collagen synthesis;
- atrophy of epithelial tubules;
- fibrous changes in the interstitium;
- sclerosis of capillaries;
- infiltration by macrophages, lymphocytes;
- deposition of calcium salts – papillary calcification.
With tubulointerstitial nephritis, the density of urine decreases, tubular epithelial cells appear in it, sodium content increases, calcium concentration decreases, the rate of tubular filtration decreases, and changes develop that lead to hypokalemia.
Dysfunction of the tubules is manifested by acidification of urine and metabolic acidosis. The urine acidity (pH) of patients is less than 5.3. Impaired concentration ability is manifested by polyuria and nocturia.
Symptoms
All types of TIN are accompanied by similar symptoms:
- increased blood pressure;
- the appearance of urinary syndrome;
- renal dysfunction.
Patients complain of deterioration in general health:
- frequent urination with sharp pain;
- frequent urge to urinate at night;
- pain in the lower back;
- thirsty;
- headache;
- dry mouth;
- poor appetite.
The most characteristic symptoms in both children and adults of TIN are an increase in the volume of daily urine (in 80% of patients), thirst (50%), discomfort, and lower back pain (25%).
An increase in the upper limit of blood pressure is observed in 80% of patients with TIN, an increase in the lower limit develops in 90% of patients.
Urinary syndrome manifests itself:
- proteinuria of low molecular weight proteins with daily protein up to 2 g;
- hematuria;
- abacterial leukocyturia - increased content of lymphocytes and eosinophils in the urine;
- hyponatremia;
- decrease in total blood volume (hypovolemia).
Symptoms of tubulointerstitial nephritis include polyuria, which develops in most patients affected by nonsteroidal anti-inflammatory drugs.
Forecasts
Provided proper treatment of the acute form of tubulointerstitial nephritis and isolation from the damaging agent, the prognosis of the disease is favorable.
When the disease is detected at the chronic stage, the prognosis depends on the duration of contact with the damaging agent and the intensity of exposure. Patients may need hemodialysis.
Diagnostics
The diagnosis is made based on a comprehensive examination. The diagnosis is as follows:
- clinical and biochemical blood test;
- general analysis of urine and feces;
- Ultrasound of the kidneys;
- radiography;
- MRI;
- kidney biopsy.
In a urine test, the following changes will be visible: a decrease in protein, leukocytes and red blood cells, a decrease in urine density, an alkaline reaction, and the appearance of sodium. Blood tests reveal anemia (hemoglobin below 100), sodium and eosonophil levels increase.
Before prescribing treatment, tubulointerstitial nephritis is differentiated from urolithiasis, tumors and nephroptosis.
In acute nephritis, ultrasound can detect enlarged kidneys; in the chronic form, the organs are within normal limits.
Symptoms of the disease
The course of the disease directly depends on its form. The main symptoms of the disease include:
- increased body temperature;
- fever;
- urticaria rash (urticaria);
- pain during urination;
- an increase in the size of both kidneys;
- detection of purulent discharge in the urine;
- presence of pain in the lumbar region and side;
- general weakness;
- decreased activity due to excessive fatigue;
- decreased appetite.
Sometimes the symptoms are hidden or unnoticeable over a long period of time, which makes it possible to identify the disease only during a medical examination, which will show the presence of renal failure.
Chronic tubulointerstitial nephritis has nonspecific symptoms, so the patient does not pay attention to the signs of pathology for a long time or simply confuses them with the symptoms of other ailments. In some cases, fluid may be retained in the body. The acute form of the disease is characterized by thirst and frequent urination.
Urticaria is the main symptom of tubulointerstitial nephritis
Tubulointerstitial nephritis occurs in children with an incidence of 1.5% to 5%, based on renal biopsy findings. Experts are inclined to believe that the etiology of the disease is immunoallergic. Quite often the disease begins to progress if the child has dysmetabolic nephropathy (approximately 15% of cases). To prevent the occurrence of pathology, the child’s parents need to consult a doctor when symptoms appear, and promptly and completely treat immune, allergic and other diseases, as well as metabolic pathologies.
Treatment
Treatment of tubulointerstitial nephritis should begin with eliminating the cause of the disease. If the disease is caused by a drug, then you need to stop taking it.
Nephritis should be treated before kidney failure occurs. Therapy is aimed at eliminating symptoms, normalizing urine outflow, restoring filtration and maintaining the normal functioning of all organs.
Treatment involves:
- taking medications;
- bed rest;
- dieting.
Drug therapy lasts at least 7 days.
It is important to lead a healthy lifestyle, avoid stress, physical activity and hypothermia. Dietary nutrition involves excluding salt, seasonings and spices from the diet. You need to give up smoked meats, pickles and marinades. Drinking plenty of fluids is important. Herbal infusions that have a diuretic effect are useful.
Patients with tubulointerstitial nephritis should undergo hemodialysis annually.
In children
Treatment of interstitial nephritis in children should be under the supervision of a physician. During therapy, intermediate blood and urine parameters are examined. Acute tubulointerstitial nephritis in children must be treated with antihistamines, for example, Suprastin. Prednisolone is used only in severe cases.
The child is prescribed antibacterial drugs. Ampicillin, Cedex, Furagin are effective. After the acute period subsides, physiotherapy is prescribed.
Chronic tubulointerstitial nephritis of an unspecified form is treated for a month with glucocorticosteroids.
In adults
Tubulointerstitial kidney disease is treated with the following medications:
- antibiotics (Ciprofloxacin, Levofloxacin, Sulfanilamide);
- detoxification drugs (Reosorbilact);
- diuretics (Furosemide);
- drugs to normalize blood pressure (Captopril).
It is necessary to reduce the intake of medications that are excreted by the kidneys. If no improvement is observed 2-3 days after the start of treatment, glucocorticosteroids are prescribed, for example, Prednisolone.
Treatment of chronic interstitial nephritis is long-term. Glucocorticosteroids, antihistamines, and anticoagulants are prescribed. Among vitamin complexes, Rutin, Pyrodixin, ascorbic acid, and calcium gluconate are effective. For iron deficiency anemia, B vitamins are prescribed, in particular B12.
It is possible to restore kidney function within 1-2 months. The prognosis for the chronic form depends on the timeliness of treatment and whether fibrosis was avoided.
Tubulointerstitial nephritis (acute and chronic): symptoms, causes and treatment
Acute tubulointerstitial nephritis (TIN) is nonspecific. If measures are not taken in time, the passages (tubules) of the kidneys gradually atrophy, and the kidneys themselves cease to function normally.
Due to disruption of the blood filtration process, all body systems suffer. The nature of tubulointerstitial nephritis may be hidden in metabolic or immune changes, external influences of infection and chemicals.
Inflammation of all structures of the renal tissue and canals of the kidneys occurs.
In the CIS countries, the disease is not widespread; according to statistics, 1.7% of the population have TIN. Every year such patients must undergo hemodialysis (extrarenal blood purification).
Classification of the disease
There are several criteria by which TIN is divided:
- by the nature of the flow;
- due to occurrence;
- by pathogenesis;
- by the nature of the tubular disorder.
The nature of the tubular disorder can be of three types:
- Endocrine dysfunctions.
- Partial violations.
- Disorders of the tubules.
The form of the disease can be acute or chronic.
The disease can be hereditary, in which case it is called Alport syndrome. A child is born with glomerulopathy or hematuria, which reduces kidney function and leads to failure. Tubulointerstitial nephritis in children is accompanied by visual and hearing impairment.
The sudden onset of renal failure is the main symptom of the acute form. This occurs as a result of damage to the kidney tubules and tissues.
Chronic tubulointerstitial nephritis appears after damage to these same structures on a larger scale. The most common reason is prolonged or uncontrolled use of medications, the influence of another kidney disease.
Tubulointerstitial nephritis can be primary or secondary. The primary one is caused by a harmful agent, for example, chemicals, infections, toxins, or metabolic failure. Secondary tubulointerstitial nephritis appears if the body already has chronic kidney disease, namely radiation nephritis, amyloidosis, nephroangiosclerosis, glomerulonephritis.
The following classification according to the nature of the damaging factor:
- infectious;
- drug;
- immune;
- metabolic disorders.
Various treatment options for the disease
In uncomplicated chronic tubulointerstitial nephritis, the patient receives most of the medications at home.
To monitor the state of health and the dynamics of the process, it is necessary to regularly undergo tests and be examined by a specialist.
In case of severe disease, the victim is hospitalized and measures are taken to stabilize his condition.
Main goals of therapy:
- normalization of blood pressure levels;
- stimulation of regeneration processes;
- increased activity of the immune system;
- prevention of the development of secondary complications;
- protecting the body from infections.
Table: pharmaceuticals for the treatment of chronic tubulointerstitial nephritis
| Name of the medication group | Examples of drugs | Main effects of the appointment |
| Nonsteroidal anti-inflammatory drugs |
| Relieves severe pain, lowers body temperature, eliminates swelling of soft tissues |
| Hormonal anti-inflammatory drugs |
| |
| Antihypertensive medications |
| Maintain stable blood pressure levels |
| Immunostimulants |
| Helps increase the overall activity of protective cells and protects against infections |
| Detoxification products |
| Removes toxins from the body in case of drug, drug or chemical poisoning |
Photo gallery: medications for the treatment of chronic tubulointerstitial nephritis
Capoten normalizes blood pressure
Immunal strengthens the immune system
Ketorol relieves pain and inflammation
Dietary recommendations for patients
With such a pathology, the load on the kidneys, which cleanse the blood of foreign impurities and eliminate them, sharply increases. Many chemicals enter the body in varying quantities with food: this is why it is so important to monitor the quality of food.
Doctors advise eating small portions 5-6 times a day, limiting the amount of table salt, eliminating fast food, alcoholic drinks, fatty and fried foods.
The diet should consist mainly of natural products that are heat-treated.
Sample nutrition menu for patients with a similar diagnosis:
- Breakfast. Omelette of two eggs with low-fat milk with the addition of parsley, cilantro, basil and spinach. Some toast with butter and goat cheese. As a drink, you can use natural freshly squeezed juice or tea.
- Dinner. Borscht made with lean beef and dill. Vegetable salad of cucumbers, cabbage, tomatoes and onions.
- Dinner. Durum pasta with broccoli, green peas and fish medallions (salmon, pollock). You can also eat a few crispbreads.
- Snacks. Vegetables, berries, nuts or dried fruits in combination with cottage cheese or yogurt.
Photo gallery: healthy food
Vegetables and fruits are rich in vitamins
Nuts are the best source of amino acids
Dairy products contain a lot of calcium
Folk remedies for relieving symptoms of chronic tubulointerstitial nephritis
Some kidney problems can be treated with alternative medicine. Folk remedies based on medicinal plants and herbs also have healing properties. But do not forget that you can completely get rid of the disease and the cause that caused it only with pharmaceutical drugs. All natural recipes help to cope only with symptoms.
One of my patients, who was diagnosed with chronic tubulointerstitial nephritis, upon learning of her diagnosis, refused hospitalization and subsequent treatment. She went home and sought the services of a healer, who prescribed her to take unnatural dietary supplements and tinctures.
As a result of the treatment received, the woman’s condition rapidly deteriorated, and one day the victim fell into a coma. The patient was urgently taken to our hospital, where doctors performed the necessary interventions.
It turned out that due to improper therapy, she developed uremic intoxication of the body, which entailed undesirable consequences.
The most popular drugs for the treatment of chronic tubulointerstitial nephritis:
- Mix 50 grams of fresh or frozen raspberries with the same amount of blueberries and pour a liter of boiling water. After cooling, drink 1 glass of the product in the morning and evening. These berries have a pronounced anti-inflammatory effect, relieve swelling of soft tissues and relieve discomfort. This product must be used at least twice a week for a month.
- Brew one teaspoon of calendula in a glass of boiling water and leave overnight. In the morning before breakfast, drink the product and start eating after 15 minutes. Calendula is believed to have antiseptic and antimicrobial properties, protecting the body from harmful microbes. This remedy should be used 2-3 times a week for six months.
- Mix 100 grams of lingonberries with 50 grams of blackberries and add 2 slices of lemon, placing everything in a saucepan with 2 liters of water. Cook for half an hour, stirring constantly. Then you can add sugar or honey according to your taste preferences. You need to drink 1 glass of this remedy every 3 hours: this will remove toxic substances from the body. The cleansing procedure should be carried out no more than once a week.
Photo gallery: folk remedies to combat pathology
Raspberries also reduce fever
Calendula has an anti-inflammatory effect
Lingonberry helps eliminate toxins
Causes of the disease
Unspecified acute tubulointerstitial nephritis occurs when the body is exposed to external harmful factors. The main harmful agents are infections, medications and allergens.
Which substances most affect the tissues and tubules of the kidneys:
non-narcotic analgesics;
- antibiotics;
- sulfonamides;
- immunosuppressants;
- substances for chemotherapy;
- iodine, lithium;
- biological toxins, pesticides;
- heavy metals;
- medicinal herbs, herbicides;
- alcohol.
TIN develops as a result of metabolic disorders, namely:
- clogging of blood vessels with cholesterol;
- increased levels of uric acid in the blood.
The kidneys suffer due to the following systemic diseases:
- hepatitis;
- oncological diseases;
- diseases of the lymphatic system;
- anemia;
- myeloma;
- diseases of the genitourinary system;
- vasculitis;
- sarcoidosis;
- Sjögren's syndrome.
Infections that have a negative effect on the kidneys:
Source: https://alternativa-mc.ru/bolezni/ostryj-tubulointersticialnyj-nefrit.html
Prevention
Manifestations of interstitial nephritis can be prevented by following these recommendations:
- do not self-medicate, take medications only as prescribed and under the supervision of a doctor;
- adhere to a balanced diet;
- avoid hypothermia;
- drink plenty of fluids, especially clean water;
- to refuse from bad habits;
- treat infectious diseases in a timely manner.
It is also important to adhere to preventive measures to prevent infection with viral and fungal diseases.
The kidneys help eliminate toxic substances; the normal functioning of the entire body depends on their work. If not treated promptly, interstitial nephritis can cause serious health problems.
Author: Oksana Belokur, doctor, especially for Nefrologiya.pro