Among childhood kidney diseases, the leading place is occupied by glomerulonephritis in children. Glomerulonephritis is usually called a whole group of diseases that manifest themselves as bilateral kidney damage in children and damage to the renal glomeruli (glomeruli). Glomerulonephritis is often called simply “nephritis”, this is not entirely correct, since nephritis is a general inflammation of the kidneys, and not just the glomeruli. In general terms, this is a very serious disease that requires long-term and proper qualified treatment.
Glomerulonephritis in children - what is it?
Glomerulonephritis is a group of renal disorders that can occur and manifest differently. The pathology is acquired. Often occurs in children of primary and school age (from 3 to 9 years). Rarely occurs in babies in the first years after birth. Boys are twice as likely to suffer from glomerulonephritis than girls.
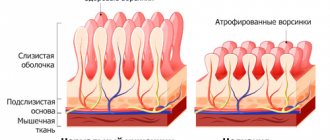
Glomerulonephritis refers to bilateral infectious and allergic kidney damage. The glomeruli are affected first. The disease then affects the entire tissue of the organ. Inflammation can spread to other body systems. Metabolism is disrupted. The kidneys lose their ability to filter plasma and decrease in size.
Classification
Depending on the cause, the disease is divided into:
- Bacterial (post-streptococcal glomerulonephritis in children);
- Parasitic;
- Viral;
- Immunologically determined;
- Immunologically unconditioned.
The disease can be primary or secondary. In the latter case, it occurs as a complication after another pathology. The disease is also classified according to its current. Acute glomerulonephritis in children is characterized by a clear clinical picture. The simultaneous presence of edema, hypertension and nephrotic symptoms.
Chronic glomerulonephritis in children develops a year after infection. Its appearance is fraught with serious consequences. Without appropriate treatment, the baby's condition will only worsen. Therapy is prescribed based on the main symptoms. With glomerulonephritis with nephrotic syndrome in children, especially in the acute period, there is a high risk of renal failure.
Depending on the affected area, the pathology can be diffuse or focal. Acute diffuse glomerulonephritis in children is an infectious-allergic disease that affects not only the glomeruli, but also the parenchial tissue directly. The tubules are practically not affected. This disease is a consequence of taking medications, poisoning, mechanical injuries, and allergic-type desensitization.
The hematuric form of glomerulonephritis in children differs from the others in the absence of age limits and the presence of blood in the urine. In addition, swelling of the kidneys and hypertension are observed. There are two types: recurrent and slowly progressive. There is also a classification of glomerulonephritis in children by localization (extracapillary and intracapillary).
There are many kidney diseases. Some of them are characterized by similar clinical manifestations, for example, pyelonephritis and glomerulonephritis. In the first case, the calyces of parenchial organs are affected in children. If a young patient is diagnosed with these diseases, there is no need to panic. Glomerulonephritis in children is completely curable, the main thing is to comply with all the requirements of the attending physician.
Causes
Various reasons lead to the development of renal pathology:
- Poor nutrition.
- Heredity.
- Untreated infectious diseases.
- Incorrectly selected treatment regimen.
The disease is not caused by infection, but by the body's response to it. Glomerulonephritis often appears after a child has had scarlet fever, tonsillitis, influenza, chronic tonsillitis, pneumonia, or measles.
The disease can be triggered by severe hypothermia, consumption of allergens, certain groups of antibiotics, sulfonamides, prolonged exposure to the sun, and vaccinations.
Mechanisms involved in the formation of glomerulonephritis:
2. Cellular components of inflammation (lymphocytes, as well as monocytes, polymorphonuclear cells, etc.) under the influence of chemotactic factors are concentrated in the glomerulus and directly damage the capillary wall, which is accompanied by endothelial detachment.
3. The mesangium can synthesize proteins that regulate catabolic processes in the matrix, and also affect the structure of the glomerular basement membrane in children.
4. Fibronectin (high molecular weight glycoprotein, present in body fluids and in the extracellular matrix).
5. The interaction of various immune mediators changes the synthesis of eicosanoids by the endothelium, mesangial cells of the glomerulus, and resident macrophages. Eicosanoids have an autoregulatory effect on mesangial cells; they can cause intraglomerular vasoactive effects, glomerular hypertension, and a proinflammatory reaction.
6. Endothelial cells in a normal state provide an eucoagulant state.
7. Mononuclear leukocytes participate in the infiltration of the glomeruli of the kidneys, promote the production of interleukin-1, which enhances the proliferation of mesangial cells. Interleukin-1, tumor necrosis factor, lymphotoxin have a procoagulant effect and stimulate cell growth.
8. Stimulation of macrophages by interleukins leads to mesangial proliferation.
9. In the pathogenesis of glomerulonephritis, a disorder in the hemostatic system (activation of coagulation processes up to the syndrome of disseminated intravascular coagulation) is the link between impaired immunity and inflammation.
The most reasonable interpretation of glomerulonephritis as a disease characterized predominantly by bilateral immune-mediated inflammation of the kidneys and primary damage to the glomeruli, caused by an imbalance of the regulatory mechanisms of immunocompetent cells and cells that predetermine a genetic predisposition to the development of the disease (HLA antigens B8, B12, B35, DR2 are associated with increased possibilities of formation immune complexes antigen-antibody, insufficient functional activity of macrophages, as well as a certain sensitivity to nephritogenic strains of streptococcus).
There are primary (actually primary diseases of the glomeruli of the kidneys) and secondary (in some systemic diseases) glomerulonephritis.
Primary glomerulonephritis in the clinic is manifested by nephritic, urinary, pure or mixed nephrotic syndromes, and morphologically by the following changes:
— Extracapillary with crescents;
| Forms of glomerulonephritis | Activity of the renal process | Kidney function status |
| Acute: - With acute nephritic syndrome; — With nephrotic syndrome; — With isolated urinary syndrome; — With nephrotic syndrome, hematuria, hypertension | The period of initial manifestations. The period of advanced clinical manifestations. Period of reverse development. Transition to chronic glomerulonephritis | Without renal dysfunction. 3 impaired renal function. surge arrester |
| Chronic: - Nephrotic form; — Hematuric form; — Mixed form | Period of exacerbation. Period of partial remission. Period of complete clinical and laboratory remission | Without renal dysfunction. 3 impaired renal function. Chronic renal failure |
| Subacute (malignant) | 3 impaired renal function. Chronic renal failure |
Symptoms
The disease usually occurs acutely in children. The following symptoms are characteristic of glomerulonephritis:
- Pain in the lumbar area.
- Swelling of the face, especially in the eyelid area.
- Hypertension.
- Reducing the daily amount of urine excreted.
- Urine takes on a dark rusty color.
- Headache.
The state of health deteriorates sharply and rapidly. The most dangerous is the rapidly progressing form of acute glomerulonephritis. Then the following manifestations are added to the general symptoms:
- Presence of flakes in urine.
- The appearance of blood clots in urine.
- The presence of a large number of protein bodies in the urine.
It happens that the pathology occurs hidden. Then most of the signs described above are not observed in the child. The disease can only be recognized during a preventive examination and testing.
Main symptoms and methods of treatment of acute glomerulonephritis
The signs of this disease almost always appear very clearly, so it is incredibly difficult to miss this disease.
As a rule, in the acute phase the disease is accompanied by the following symptoms:
- general weakness, including muscle weakness;
- increased fatigue, inability to perform usual activities, excessive drowsiness;
- strong thirst;
- a gradual decrease in urine output during the day;
- change in color of discharge;
- noticeable swelling that starts from the face and spreads to the lumbar region and lower extremities;
- headache;
- nausea and vomiting;
- blurred vision;
- simultaneous increase in upper and lower blood pressure. This symptom may indicate a possible transition of the disease to the chronic stage. If the situation does not return to normal within 3-4 months, and hypertension persists, despite all the measures taken, most likely, acute glomerulonephritis was followed by complications, and this disease took a chronic form.
Acute glomerulonephritis can provoke other complications, namely:
- acute renal or heart failure;
- intracerebral hemorrhage;
- preeclampsia or eclampsia;
- cerebral edema.
That is why, in order to prevent the development of such complications, treatment of this disease should begin immediately after the first signs of the disease are detected. As a rule, if the child himself does not complain to his parents about changes in his condition, mom and dad begin to suspect something is wrong based on the change in the color of the baby’s urine.
Diagnostics
Glomerulonephritis is characterized by symptoms similar to pyelonephritis. Therefore, the disease is difficult to diagnose. To make an accurate diagnosis, the following studies are carried out:
- Urine and blood tests.
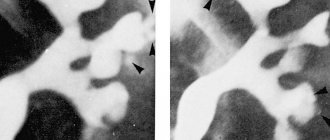
- Ultrasound of the kidneys.
- Radioisotope angiorenography.
- ECG.
- Doppler ultrasound.
- Kidney biopsy.
- Samples of Reberg, Zimnitsky.
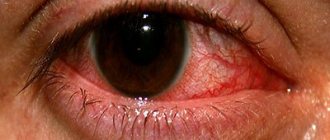
The fundus of the eye is also examined using a special device. Based on the diagnostic results, the doctor selects effective therapy.
Treatment
To treat glomerulonephritis, medication and traditional methods are used. The latter can only be used as a supplement to the main therapy with pharmaceutical drugs. The child is usually hospitalized in a hospital. Bed rest and a special diet are indicated.
If renal pathology is caused by infection, then a course of antibacterial drugs . If the cause is chronic tonsillitis, then tonsillectomy is indicated three months after the completion of the acute stage of the disease. The steroid hormones Dexamethasone and Prednisone are also used. If glomerulonephritis does not go away for a long time, corticosteroid hormones are prescribed. In parallel, vitamin therapy is used.
Spa treatment methods are also beneficial for the child. For example, sanitation of chronic foci of infection, mud applications, balneotherapy.
Etiology
Causes of glomerulonephritis in children that have an allergic rather than infectious basis:
- bites from poisonous insects or snakes;
- foreign proteins;
- drug overdose;
- poisoning by chemicals, namely mercury or lead;
- administration of vaccines or serums;
- plant pollen.
In addition, the development of inflammation in the renal glomeruli can be affected by:
- hereditary predisposition;
- autoimmune diseases;
- systemic lupus erythematosus;
- sudden climate change;
- prolonged hypothermia or, conversely, overheating of the child’s body;
- cystitis, pyelonephritis and other infections in the genitourinary system;
- hemorrhagic vasculitis;
- childhood rheumatism;
- previously suffered acute respiratory viral pathologies, in particular, pneumonia and tonsillitis, impetigo and scarlet fever, pharyngitis and streptoderma;
- hypovitaminosis;
- asymptomatic carriage of streptococci, for example, on the skin.
It must be taken into account that in some cases it is not possible to find out what caused glomerulonephritis in a child.
Mechanism of development of glomerulonephritis
The main risk group includes children of preschool and primary school age categories; less often, the disease is diagnosed in children in the first 2 years of life. It is noteworthy that boys suffer from the disease several times more often than girls.
Diet
To speed up the healing process, you need to follow a special diet that promotes urination and improves metabolic processes in the kidneys. The child should limit salt and liquid intake. You need to eat 6 times a day.
Allowed to eat:
- Salt-free cornbread.
- Protein omelet.
- Porridge.
- Vegetable soups.
- Lactic acid products.
- Vegetable oils.
- Milk.
- Vegetables.
- Pasta.
- Fruits.
The following products are prohibited:
- Fish, mushroom, meat sauces and broths.
- Refractory fats.
- Pickles.
- Smoked meats.
Prognosis and complications
The prognosis of glomerulonephritis depends on the timeliness and effectiveness of therapy. If treatment is started on time, the diet and doctor’s instructions are followed, then recovery occurs quickly. Ignoring the symptoms of the disease and lack of proper therapy can lead to serious complications. For example, to:
- Brain edema.
- Kidney failure.
- Preeclampsia.
- Intracerebral hemorrhage.
- Eclampsia.
- Problems with the heart.
What complications can the disease cause?
If the diagnosis of acute glomerulonephritis in children was not carried out on time, then the disease becomes chronic, which is fraught with serious consequences and complications. In the future, the child may suffer from renal eclampsia, uremia, nephrotic encephalopathy, renal and heart failure. He may also experience bleeding in the brain, severe convulsions and seizures, and swelling of the lungs.