Dyspepsia is a syndrome, i.e. a set of symptoms associated with disorders of the upper digestive system, namely the stomach, esophagus and duodenum.
Dyspepsia can be organic, i.e. associated with a physical defect or disease (ulcer, perforation, gastroduodenitis, etc.), as well as with impaired absorption of one or another type of substance. In the latter case, the disease is called functional dyspepsia, which is divided into fermentative, putrefactive and fatty forms.
Fermentative dyspepsia - impaired digestion of carbohydrates
When carbohydrates are not digested intensively enough, a condition called fermentative dyspepsia occurs.
The exact causes of this condition are not known, we can only state that this form of functional dyspepsia often develops against the background of diets rich in carbohydrates and coarse fiber. It is also believed that this syndrome is partly associated with insufficiently thorough chewing of food, i.e. with eating “on the run”, as well as with the constant consumption of carbonated (especially sweet) waters and energy drinks.
As a result of fermentation, a large amount of acids are formed in the intestines, irritating the mucous membranes and causing classic symptoms of fermentative dyspepsia.
Cold and carbonated drinks, sweet foods consumed in the heat, and stale food provoke an exacerbation. The intestines absorb the resulting toxins, making you feel worse and disrupting the normal digestion process (cyclical process).
If the pancreas does not work intensively enough (for example, in various forms of pancreatitis), then the secretion of amylase and other enzymes that break down sugars decreases.
Varieties
Clinicians divide dyspeptic disorders into two large groups:
- functional or simple dyspepsia . In this case, the symptoms of the disease appear in the presence of an exclusively functional lesion, for example, impaired motility in the digestive system. There are no organic pathologies. Often this form appears during pregnancy. It is important to carry out her treatment in a timely manner in order to stabilize the woman’s condition during this period;
- organic dyspepsia . In adults and children, this pathology manifests itself against the background of existing pathologies of the gastrointestinal tract. Its symptoms usually appear acutely and do not disappear over a long period of time. Without treatment, the clinic will only intensify, which can lead to irreversible consequences.
Types of dyspepsia
The following classification is based on the reasons that caused the symptoms of dyspeptic syndrome. Based on this, the following forms of pathology are distinguished:
- nutritional _ Symptoms appear when the diet is disrupted. This form has several more subspecies. Fermentative dyspepsia develops if a person abuses foods high in carbohydrates. Putrefactive - if protein products predominate in the diet. Fatty – when a large amount of fat enters the human body;
- dyspepsia, caused by insufficient secretion of enzymes involved in the digestion of incoming foods. There are four types - enterogenic, gastrogenic, hepatogenic and pancreatogenic;
- dyspepsia, which develops when the process of absorption of nutrients in the human intestine is disrupted;
- toxic dyspepsia . One of the most severe forms of pathology. Toxic dyspepsia manifests itself as a result of poisoning of the human body in the presence of purulent infections, acute surgical pathologies, as well as poisoning with toxic substances (for example, at work). This condition is especially dangerous during pregnancy. The symptoms are very pronounced and the intensity of their manifestation is constantly increasing. Treatment of toxic dyspepsia should be carried out as soon as possible;
- dyspepsia of infectious origin . This group includes two subspecies - salmonella dyspepsia and shigellosis. Progresses against the background of these intestinal infections.
Features of the disease
Most often, exacerbations of fermentative dyspepsia occur in the warm season, as well as when traveling to hot countries. This is due to a slight decrease in the secretory activity of the stomach and pancreas (in the heat, loss of water leads to a decrease in the activity of all glands). An additional factor that provokes fermentative dyspepsia is constant thirst - diluted digestive juices do their job worse.
Photo gallery: factors provoking fermentative dyspepsia
The process can be either acute or chronic. Anyone can have acute fermentative dyspepsia (overeating foods rich in carbohydrates), chronic dyspepsia is “tied” to individual metabolic disorders, enzyme deficiency.
If you constantly consume foods that provoke the disease, you can induce the development of a chronic form of fermentative dyspepsia.
Dyspepsia in young patients
Stomach or intestinal upset can occur at any age. So what is dyspepsia in babies? Often, the complex of symptoms of this disease is practically no different from the manifestations of the disease in adults. Discomfort, a feeling of heaviness, pain, bloating are the main signs of non-ulcer dyspepsia. In the case of the ulcerative “variant,” the pain will most likely become more frequent and go away only after the child eats a hearty meal. This is due to the fact that the stomach needs to be constantly filled so that it does not digest its own walls.
Among the causes of childhood dyspepsia are, in particular, impaired communication and coordination between the central nervous system and the gastrointestinal tract. This occurs during a period of intensive growth of the baby. The child’s nutrition plays an important role: he should not eat unhealthy, fatty foods or fast food. His diet should be balanced and contain only natural and “light” foods. Symptoms of dyspepsia can also arise against the background of emotional overload, depending on the situation in the family, team, and educational loads. Finally, scientists believe that heredity may also contribute to the onset of gastric dyspepsia at an early age.
Symptoms of fermentative dyspepsia
As a rule, dyspepsia is accompanied by pain in the upper abdomen and a feeling of discomfort. Depending on the nature of the food and the type of disorder, the process may include belching, bloating, nausea and vomiting.
These manifestations occur spontaneously and periodically. Often the cause of exacerbation is an error in diet (instant noodles, spicy dishes, etc.). Most often, these symptoms go away on their own and do not require medical intervention.
Photo gallery: symptoms of the problem
Unfortunately, if a person ignores metabolic disorders and does not follow a diet, then the frequency of pain, heartburn and vomiting increases, which can significantly reduce the quality of life.
Pain may decrease somewhat after defecation. The stool is loose, frequent, light yellow in color, may bubble and have a pungent odor. Diarrhea up to 4 times a day, there is no blood in the stool, since only the upper intestines are affected. Partially digested fruits and vegetables can be seen in the stool.
All this is accompanied by rumbling in the stomach, flatulence (gas), and a feeling of heaviness after eating.
Severe headaches begin from the constant absorption of toxins, especially in people prone to vascular spasms. Irritability and nervousness appear, and labor productivity drops.
When palpating the abdomen, bloating is immediately detected, rumbling and splashing are heard in the paraumbilical area (around the navel).
Reviews and results
Dietary nutrition for intestinal dyspepsia, according to customer reviews, helps improve intestinal function: reducing spasms, bloating, pain (colic), and normalizing stool.
- “... Complaints of flatulence, bloating against the background of frequent bowel movements. I went to the hospital, but they didn’t find anything special about me. They recommended going on a diet. I noticed that when I practice dietary nutrition, everything quickly returns to normal, on average, after 2-3 weeks, but as soon as I switch to my usual diet, everything starts again. It is probably necessary to undergo a more thorough examination in a paid clinic or, in addition to the diet, take folk remedies in the form of herbal decoctions or preparations based on them”;
- “... Cramps in the intestines and bloating for almost 2 months. At the same time, there is no bowel disorder. I went to the clinic and got tested. The doctor told me to follow a diet and prescribed Espumisan. To prepare dietary dishes, I purchased a multicooker. Everything cooks very quickly and turns out delicious. I excluded all fatty foods, sausages, flour, and sweets. For now I eat boiled chicken and fish, boiled and pureed vegetables. I eat little by little, I try to eat separately, that is, I don’t mix meat and cereals and bread into one meal. I take a decoction of chamomile and dill water. The condition is gradually improving. I think it’s better to watch your diet than to suffer with cramps.”
When to see a doctor
Constant dyspeptic symptoms on the background of a balanced diet. If this happens, then fermentative dyspepsia in one way or another “flowed” into a chronic form, or, even worse, into a functional one. As a result of careless attitude to health, fermentative dyspepsia can lead to reflux disease (reflux of gastric contents into the esophagus with burns to the latter), gastritis, gastroduodenitis, and nonspecific ulcerative colitis.
Constant fermentation provokes a lot of inflammatory processes, which is the foundation for the development of chronic inflammatory diseases.
If dyspepsia is accompanied by shortness of breath, vomiting, or severe sweating, you should consult a doctor.
If the stool turns black, it is better to go straight to the surgeon (intestinal bleeding).
Diagnosis of fermentative dyspepsia
After examination and questioning, the doctor in such cases may prescribe the following procedures:
- fibroesophagogastroduodenoscopy (FGDS). The endoscope is inserted through the esophagus and stomach into the duodenum. The entire surface of the mucous membrane is examined, and it is possible to take samples from suspicious areas (biopsy). This study makes it possible to distinguish fermentative dyspepsia from organic forms of the disease;
- contrast radiography. A barium suspension is injected into the stomach, which eliminates peptic ulcer disease, incl. erosion of the mucous membrane of the stomach and duodenum;
- Ultrasound examination of the abdominal organs. It is performed to exclude an oncological component, pancreatitis, and gallstones.
Stool examination allows you to analyze the efficiency of food digestion, the presence of inflammatory diseases of the digestive system, giardiasis, and helicobacteriosis.
Functional dyspepsia (including the fermentative form of the disease) is diagnosed only in the absence of organic changes in the stomach and intestines. Symptoms of fermentative dyspepsia must manifest themselves for at least 3 months over the entire past year. The doctor also asks the patient about the connection between symptoms and the frequency of bowel movements and diets used.
Stomach upset - causes and symptoms
Gastric dyspepsia accompanies many other diseases. Some of them turn out to be a serious threat to health and life, so long-term symptoms of dyspepsia should not be underestimated. Dyspepsia can manifest itself in the course of peptic ulcers, gastric and esophageal tumors, gastric reflux, cholangitis and pancreatitis. It can also be caused by taking certain medications (including antirheumatic drugs, iron and potassium supplements, antibiotics). Tobacco smoke is a provocateur of dyspepsia (people suffering from this disease should immediately quit smoking), and poor nutrition and psychological background worsens the situation. To reduce or completely prevent pain, it is necessary to pay attention to lifestyle and environmental factors in addition to proper therapy.
Most people are very familiar with the classic symptoms of dyspepsia. What is it: just pain, poisoning or really a disease? Knowing exactly how the disease manifests itself will help answer this question. A patient may be said to have dyspepsia if at least two of the following symptoms persist for a long time:
- epigastric pain;
- feeling of heaviness and fullness in the stomach after eating;
- belching;
- nausea, vomiting;
- lack of appetite;
- heartburn.
General principles of therapy
Treatment is strictly individual, since the causes of functional types of dyspepsia can differ significantly.
First of all, a strict diet is prescribed, excluding coarse and difficult to digest foods. Meals should be fractional (5-6 times a day).
For the first two days of illness, it is generally recommended to fast and drink only weak (not hot) tea without sugar.
To support the patient’s body, up to 1 liter of glucose (5%) or saline solution per day can be administered.
Subsequently, milk, brown bread and carbonated drinks are excluded.
Most often, gastroenterologists recommend diet No. 4a. After some time, easily digestible carbohydrates begin to be introduced.
The treatment is combined with classic folk recipes - infusion of chamomile flowers, oregano, caraway and dill.
Alcohol and smoking are contraindicated; it is recommended to stop taking anti-inflammatory drugs after consulting a doctor (ibuprofen, diclofenac, indomethacin). In such cases, the only exception may be a minimum dose of acetylsalicylic acid if there is a high risk of blood clot rupture.
All functional dyspepsia are easily provoked by severe stress, so during exacerbations the patient is advised to rest and take sedatives.
An obligatory component of treatment is the restoration of normal intestinal flora. For this purpose, certain probiotics are prescribed (Linex, Rotabiotic, Bifiform, etc.).
Selection of symptomatic remedies for fermentative dyspepsia
Some patients benefit well from proton pump inhibitors, which are prescribed to reduce stomach acidity - esomeprazole (Nexium), omeprazole (Omez).
To normalize motility, prokinetics are used, for example metoclopramide (Cerucal) or domperidone (Motilium).
With massive infiltration of the mucous membrane by Helicobacter, doctors conduct courses of anti-Helicobacter therapy. This type of treatment includes 2 antibiotics and a proton pump inhibitor or H2 blocker (ranitidine, for example).
Antidepressants are prescribed when fermentative dyspepsia is combined with stress or mental illness.
With a competent approach and an experienced doctor, the disease goes away completely in half of the patients within a year. It is worth noting that without visiting a doctor, but with the correct tactics of the patient (diet, regimen, herbal medicine), in 30% of cases there can be a spontaneous cure.
There is no specific prevention of fermentative dyspepsia. The best way to avoid illness is to eat a balanced diet and respond to any prolonged symptoms of intestinal disorders by consulting a doctor promptly.
Timely treatment, adherence to diet and nutrition, treatment of concomitant diseases - these are the necessary conditions for recovery from fermentative dyspepsia. If any unusual symptoms appear, as well as if existing ones worsen, immediate consultation with a specialist is necessary.
wikifamily.ru
Dyspepsia is the term used to describe digestive disorders. Depending on the cause of intestinal dysfunction, a distinction is made between dyspepsia associated with dysfunction of certain parts of the digestive system and insufficient secretion of digestive enzymes (intestinal, gastric, pancreatic, hepatic), and dyspepsia associated primarily with nutritional disorders (fermentation, putrefaction and fat, or soap). ).
The cause of nutritional dyspepsia is poor nutrition. Fermentative dyspepsia occurs with the predominant consumption of carbohydrates (honey, baked goods, sweets, grapes, legumes, cabbage, etc.), when their digestion is disrupted. Also, the development of fermentation flora in the intestines occurs when consuming kvass and other fermented drinks. The cause of putrefactive dyspepsia is excessive consumption of proteins (fatty lamb, pork), as well as as a consequence of eating stale meat products. Fatty dyspepsia is caused by excessive consumption of slowly digested, especially refractory, fats (pork, lamb).
Symptoms of fermentative dyspepsia include flatulence, rumbling in the stomach, gas formation, frequent, slightly colored liquid foamy stools with a sour odor.
and scatological examination, a large number of starch grains, crystals of organic acids, fiber, and iodophilic microorganisms are determined. The stool reaction is sharply acidic. There are acute and chronic forms of fermentative dyspepsia. Acute occurs when switching to unusual foods or excessive consumption of plant fiber. Chronic develops from the acute form with prolonged consumption of carbohydrate foods.
Putrefactive dyspepsia is characterized by impaired digestion of proteins and their putrefactive decomposition mainly in the large intestine. It can occur in people who have the habit of eating quickly, or with a large intake of protein foods, as well as as a result of a sharp decrease in the secretory function of the stomach and pancreas. Patients experience diarrhea; in chronic cases, it is persistent. With putrefactive dyspepsia, there is bloating of the abdomen, belching of gases with the smell of rotten eggs, feces are dark brown, liquid or mushy with a sharp putrid odor, riddled with gas bubbles. Intoxication phenomena (general weakness, headaches, etc.) may be observed. Microscopic examination of stool reveals creatorrhea. The reaction of feces is sharply alkaline.
Fatty dyspepsia is extremely rare, usually when eating large amounts of fat in people with diseases of the liver, biliary tract or pancreas; characterized by poor breakdown and absorption of fats. With fatty dyspepsia, the stools are light, abundant, neutral or alkaline. A scatological examination reveals in them a large amount of undigested neutral fat (in the form of drops), crystals of fatty acids and their insoluble salts.
Pancreatic dyspepsia is associated with exocrine pancreatic insufficiency due to chronic pancreatitis, tumors, etc. Low intake of pancreatic lipase, amylase and trypsin into the intestine leads to disruption of the digestive system. The patient feels rumbling in the intestines, flatulence, loss of appetite, sometimes colic in the abdomen, and also profuse “pancreatogenic” diarrhea (fatty stool), steatorrhea, amilorrhea, creatorrhoea.
Prevention and treatment of dyspepsia is compliance with the correct diet - prescribing a diet. It is also necessary, first of all, to treat the underlying disease that caused dyspepsia (chronic gastritis, pancreatitis, etc.).
Diet for dyspepsia
For each type of dyspepsia, there are dietary features. However, there are general recommendations that should be followed for this disease.
- Meals should be 4-6 times a day, at least. You need to eat often, but little by little. This is the basic principle of any diet.
- You need to be careful not to eat too much at night, but also not to go hungry during the day.
- Eating is done in a quiet environment; you should not watch TV or read while eating.
- A separate point is smoking. It should be remembered that it further worsens the patient’s condition with dyspepsia.
- The diet must include first courses - soups, broths.
- If possible, avoid eating artificial food additives, preservatives, and flavorings.
- It is not recommended to drink too cold water or eat very hot foods.
- The therapeutic diet should not include flour yeast products, rice, tomato paste, juices, raw vegetables and fruits. Drinking should include water, weak tea, and in no case carbonated water.
For fermentative dyspepsia, easily digestible carbohydrates are excluded from the patient’s diet and a protein-rich diet is prescribed. People eat broths, fish soup, boiled meat, fish, cottage cheese, butter, and unsweetened tea.
If the patient has putrefactive dyspepsia , meat is excluded from the menu. The food prescribed is cereals, decoctions of rice, semolina, crackers, white bread, butter, river fish, and apples. Then the diet includes yesterday's wheat bread, low-fat meat or fish broths and soups, dry cookies, lean veal, chicken, turkey, rabbit, lean fish (pike perch, bream, cod, perch, navaga), potatoes, zucchini, whole eggs, jelly , jellies, mousses, souffles from sweet varieties of berries and fruits.
For fatty dyspepsia, it is necessary to replace all animal fats with vegetable fats and reduce their amount.
For dyspepsia, adsorbent, vitamin medications are recommended; for violations of the exocrine functions of parts of the digestive system, enzyme preparations (pancreatin, festal, abomin, pepsin, etc.), hydrochloric acid; for pain, painkillers; and also treat dysbiosis.
doctornet.ru
Home » List of diseases » Dyspepsia
Ask your question
Symptoms
During fermentation, organic acids, carbon dioxide, and hydrogen are formed, which irritate the intestinal mucosa and increase motility. Feces attract water into the intestinal lumen and liquefy. Pathology occurs at any age. Characteristic symptoms appear after eating foods rich in carbohydrates.
Intestinal manifestations
Intestinal symptoms occur with dyspepsia of any severity.
- cramping pain in the abdomen, which decreases after the passage of gas and bowel movements;
- watery, foamy, light yellow stools more than 2 times a day;
- lumps in stool;
- sour smell of stool;
- feeling of fullness, bloating;
- The release of gases is practically odorless.
Extraintestinal manifestations
Insufficient digestion of carbohydrates reduces the absorption of glucose, galactose, and fructose. Fermentative dyspepsia without treatment leads to chronic inflammation in the intestines with disruption of all its functions. A deficiency of fats, proteins, vitamins, and microelements develops.
Symptoms:
- weakness;
- irritability;
- dizziness;
- weight loss in adults, insufficient weight gain in infants;
- dry skin;
- fragility and change in the shape of nails;
- hair loss.
Types of disorder
Diet for indigestion is a must!
This sensitive organ responds with negative reactions to a variety of reasons that disrupt its functioning. Depending on the category to which your stomach upset falls, an effective diet is recommended.
Digestive disorders in gastroenterology are classified into the following types:
- organic disorders,
- functional disorders.
The causes of organic disorders are considered to be bad habits and poor nutrition. The functioning of the stomach is disrupted by a sedentary lifestyle, prolonged forced sitting during work, alcohol and smoking abuse, and a large amount of spicy food in the diet. All these factors irritate the mucous membrane, destroying beneficial microflora and disrupting digestion.
Food is not completely digested, stagnation of food, its fermentation causes pain in the stomach and irritation. To cleanse the body of toxins, diarrhea occurs. In this case, fortification of food and diet help normalize digestion.
Functional indigestion is caused by gastrointestinal diseases and their consequences: gastritis, peptic ulcer, hernia, reflux esophagitis. In this case, it is impossible to do without a full examination and long-term treatment, consisting of a complex of various drugs. In this case, the diet will help compensate for the negative effects of medications and obtain useful substances for a full metabolism.
Causes
Fermentative dyspepsia is caused by two groups of reasons: enzyme deficiency and malnutrition.
Enzyme deficiency
Pancreatic amylase in the duodenum breaks down complex carbohydrates - polysaccharides into oligo- and disaccharides. Under the action of enzymes in the small intestine, monosaccharides are formed from them, which are then absorbed into the blood.
Intestinal enzymes have substrate specificity, each of them converts only a certain disaccharide: lactase breaks down lactose (milk sugar), maltase - maltose, invertase - sucrose, etc. Disruption of one enzyme leads to intolerance to a particular product. In Russia, lactase deficiency (milk intolerance) occurs in 15% of the adult population and 18% of children under one year of age. Against the background of intestinal diseases, intolerance to several carbohydrates develops.
Causes of enzyme deficiency:
- heredity;
- pancreas pathology;
- bacterial and viral intestinal infections;
- helminthiases;
- chronic enteritis;
- Crohn's disease;
- food allergies;
- long-term parenteral nutrition.
Eating disorder
When the intake of carbohydrates from food exceeds the capabilities of the body's enzyme systems, some of the undigested components undergo fermentation. Dyspepsia occurs when eating large amounts of high-carbohydrate foods:
- whole milk;
- infant formula;
- dairy products;
- fresh vegetables and fruits;
- baking;
- sweets;
- mushrooms;
- potato;
- kvass, beer;
In older people, enzyme activity decreases, and even a small error in nutrition can lead to fermentative dyspepsia.
How to eat during an acute period
The first, in the form of light soups, should be present every day.
In the first 1-2 days after the onset of an exacerbation, it is not recommended to eat at all. Allowed to take 1.5-2 liters of liquid. This can be tea with or without lemon, rosehip infusion, and almost no sugar is used.
By the middle of the second day, you can switch to a gentle diet, consisting of slimy soups, pureed porridges, jelly with white bread croutons.
Soufflés made from pureed lean meat, fish, milk creams, soft-boiled eggs, and milk are acceptable. Sauces and spices, fermented milk products, fresh bread, fresh fruits, confectionery, cocoa, coffee, and carbonated drinks are completely excluded. Salt is used to a minimum when preparing dishes.
This diet eliminates irritation of the walls of the stomach and its mucous membrane, and does not cause increased production of gastric juice. Gastroenterologists do not recommend staying on this diet for long and, at the first opportunity, switching to an expanded diet with a large number of permitted foods.
Diagnostics
Diagnosis of fermentative dyspepsia and its causes is carried out by pediatricians, therapists, and gastroenterologists.
Clinical and laboratory methods
- Anamnesis collection, examination . To make a preliminary diagnosis, typical complaints, indications of intolerance to specific foods, improvement in well-being after eliminating them from the diet, family history, acute and chronic diseases of the digestive system are important.
- Coprogram. With fermentative dyspepsia, the feces have an acidic reaction. The analysis results reveal unchanged fiber, starch grains, and lactic acid.
- Bacteriological examination of feces - the amount of iodophilic flora increases: yeast fungi, clostridia, cocci.
- Feces for worm eggs - vegetative forms and protozoan cysts, eggs of intestinal parasites are revealed.
- Stool analysis for carbohydrates is prescribed to diagnose lactose intolerance in children who do not receive complementary foods.
- Load test with disaccharides - after taking milk sugar or sucrose, the level of glucose in the blood is determined. An insufficient increase in the indicator indicates a decrease in lactase or invertase activity.
Instrumental methods
- Hydrogen test - measures the concentration of hydrogen in exhaled air. An increase in the rate is associated with bacterial fermentation in the colon.
- X-ray with contrast. The patient is given a drink of barium with lactose or sucrose and a series of photographs are taken. Accelerated movement of contrast through the intestines indicates enzyme deficiency.
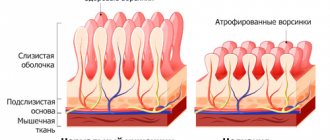
- Biopsy of the mucous membrane of the small intestine - determine the content of enzymes in the resulting material. Using research, they find out which enzyme is missing.
- Endoscopic diagnostic methods. FGS and colonoscopy reveal chronic intestinal diseases, which can lead to fermentative dyspepsia.
- Ultrasound – diagnosis of the causes of pathology; clarify the structure, size and pathological changes of the abdominal organs.
Treatment
The goals of treatment measures are to reduce symptoms and normalize the functioning of the digestive tract.
Nutrition
Diet correction is a prerequisite for successful treatment of fermentative dyspepsia.
Basic principles
- The diet is prescribed individually; if a particular enzyme is deficient, carbohydrates that it should break down are excluded from the diet.
- For dyspepsia due to diseases of the digestive system, a diet is recommended in accordance with the diagnosis.
- All patients are prohibited from foods that increase gas formation and rough foods.
- In severe cases, carbohydrates are completely eliminated for 3-4 days and the proportion of protein products in the diet is increased.
- They recommend split meals: small portions up to 6 times a day.
- Cooking methods: boiling in water or steaming, baking in the oven.
Grocery list
| Recommended | Forbidden |
In the first days of treatment:
After 3-4 days:
|
|
Children under one year of age with lactose intolerance are prescribed low-lactose and lactose-free mixtures: NAN lactose-free, Nutrilak lactose-free plus, Nutrilon premium lactose-free, etc.
Medicines
- Enzyme preparations. If the functioning of the pancreas is disrupted, medications containing pancreatic enzymes are prescribed: Creon, Mezim forte. If fermentative dyspepsia is associated with lactase deficiency, Lactazar is recommended.
- Carminatives are a group of drugs that reduce flatulence and facilitate the passage of gases: Espumisan, Bobotik, Plantex.
- Antispasmodics - reduce the tone of intestinal smooth muscles, have an analgesic effect: Buscopan, No-shpa, Duspatalin.
- Enterosorbents - bind and remove toxic products and gases from the intestines that are formed during fermentation, fix the stool: Smecta, Neosmectin, Polysorb, activated carbon.
- Antidiarrheals - reduce peristalsis, reduce the frequency of bowel movements: Imodium.