What is gluten
The concept of gluten is common to a number of cereal peptides. This gluten is an integral component of the grain shell, which ensures the elasticity of the dough. Gluten is used in the food industry as a thickener, stabilizer, and forming agent. Its increased content in the dough ensures the splendor of baked goods.
Gluten is found in various forms in cereals:
- wheat contains the protein gliadin;
- rye – secalin;
- barley – hordenine;
- oats - avenin.
They all have similar properties and are broken down by the enzyme type 2 transglutaminase. After processing, the structural formula of gluten changes and it acquires the ability to penetrate the intestinal walls. In healthy people, gluten is broken down, partially absorbed, and all residues are excreted from the body.
Why does intolerance occur?
The development of celiac disease is due to a genetic predisposition. This is proven by the prevalence of pathology between close relatives. The disease is based on an autoimmune process.
After digestion, gluten binds to blood proteins and comes into contact with specific antibodies. The reaction resembles an allergic one. The body recognizes the substance as foreign and threatening, and therefore tries to get rid of it as quickly as possible. Subsequently, the immune system looks for the source of harmful agents, which turns out to be the small intestine (this is where gluten comes from) and the defense mechanisms produce antibodies to the proteins of the intestinal smooth muscle muscles.
Due to the attack of one’s own tissues, the structure of the mucous membranes changes. The villi, which are supposed to trap toxins and move the food bolus, are smoothed out. As a result, even more “garbage” enters the bloodstream. The microflora changes, pathogenic microorganisms multiply, and the absorption capacity of the walls of the small intestine changes. Digestion and the general condition of the body suffer, and characteristic symptoms of enteropathy develop.
The longer a person with intolerance is in contact with gluten, the stronger the intestinal inflammation and the more intense the manifestations of the disease.
Peculiarities
Celiac disease can develop in various forms. With typical intolerance, symptoms appear in the first 2 years of a child’s life, after the start of complementary feeding and the predominance of foods from the “common table” in the diet.
Adults are prone to the atypical form. They show no signs of sensitivity in childhood. Symptoms of the disease do not indicate intestinal damage. They are caused by chronic lack of nutrients from foods.
The latent (hidden) form of celiac disease may not manifest itself throughout life and manifest itself only in old age, against the background of concomitant diseases. Moreover, antibody production is not always triggered by genes. The disease in a child can be caused by trophic disturbances during the prenatal period, intoxication of the mother’s body during pregnancy, or viral infections in the first months of life.
In adults, autoimmune intestinal damage is triggered by stress, poor diet, poisoning, bad habits, hormonal fluctuations and chronic pathologies of the gastrointestinal tract.
Causes
There are several reasons why celiac disease occurs in adults:
- Genetic predisposition: the appearance of this item on the list of possible causes is due to the frequent identification of relatives with similar problems in the patient. This disease is transmitted from mother to child with a probability of 1:10. However, carriers of the gene do not always become owners of such an unpleasant disease. A push is needed to activate the disease. A stressful situation, surgery, a viral infection, pregnancy - all this can trigger the onset of the disease.
- The presence of autoimmune pathology: scleroderma, diabetes mellitus, alopecia, arthritis - the presence of one of these diseases increases the risk of developing the disease.
- Congenital disorders of the small intestine: enzyme deficiency is a prime example of a disorder in which there is a risk of developing celiac disease.
Determining the cause guarantees the formation of a correct and effective treatment regimen.
What happens with celiac disease
The main problems of the pathology are intestinal inflammation, metabolic disorders, and disruptions in the functioning of the immune system. Inflammatory mediators in the epithelium of the small intestine provoke disturbances in peristalsis, a decrease in the level of immune defense, a lack of digestive enzymes, and inadequate breakdown of substances.
A lack of fatty, bile acids, proteins and carbohydrates, as well as improper absorption of vitamins and minerals, negatively affects metabolism as a whole. The body suffers from a lack of building materials, muscle weakness and blood disorders develop.
Antibodies spread throughout the body. They can attack not only the intestines, but also the cells of the liver, brain, and other organs. This is why the symptoms of celiac disease are extremely varied.
Forms of the disease
Celiac disease can develop in various forms. With typical intolerance, symptoms appear in the first 2 years of a child’s life, after the start of complementary feeding and the predominance of foods from the “common table” in the diet.
Adults are prone to the atypical form. They show no signs of sensitivity in childhood. Symptoms of the disease do not indicate intestinal damage. They are caused by chronic lack of nutrients from foods.
The latent (hidden) form of celiac disease may not manifest itself throughout life and manifest itself only in old age, against the background of concomitant diseases. The potential form means the presence of antibodies responsible for sensitivity, in the complete absence of symptoms of pathology. The disease may never appear.
Symptoms
Celiac disease can be asymptomatic!
Celiac disease may be asymptomatic (atypical form of celiac disease), and gastrointestinal symptoms may be mild or absent.
With this form, extraintestinal manifestations may be observed: osteoporosis, anemia, infertility, neurological symptoms, etc.
Characteristic symptoms are:
- Gastrointestinal symptoms:
flatulence, nausea, vomiting, loss of appetite, chronic diarrhea, profuse, foul-smelling stools. - General symptoms:
Weight loss, hypovitaminosis, anemia, fatigue, fatigue.
Consequences of the disease
A lack of nutrients in childhood leads to retarded mental and physical development; regular diarrhea is fraught with dehydration. Intestinal inflammation can result in the formation of tumors. Changes in metabolism lead to tissue degeneration throughout the body, the appearance of diabetes mellitus, and damage to the thyroid gland.
Autoimmune processes can spread to other organs. Symptoms of celiac disease significantly impair the patient's quality of life. His body weakens, chronic fatigue appears, his ability to work suffers, and his immunity weakens.
Women of childbearing age have problems conceiving and bearing a child. Even with a successful pregnancy, there is a risk of developmental defects in the fetus.
How does intolerance manifest itself?
The symptoms of celiac disease can be striking. As a rule, these are gastrointestinal signs (from the gastrointestinal tract). The set of syndromes is common for adults and children:
- Stool disorders . The patient alternates between constipation and diarrhea. In the first case, the stool is fragmented and contains undigested food particles, often light in color. After visiting the toilet, there is a feeling of incomplete emptying. With diarrhea, the stool is copious, liquid, with admixtures of fat. Frequent bowel movements (up to 5 times a day).
- Dyspepsia . Appetite decreases, after eating, flatulence, a feeling of heaviness in the stomach, and nausea appear. In rare cases, vomiting.
- Damage to other organs of the gastrointestinal tract . Against the background of celiac disease, reflux disease, gastritis, disturbances in gastric secretion and the production of pancreatic enzymes appear.
- Liver lesions . Metabolic disorders and autoimmune hepatitis often accompany celiac disease. Liver pathologies (steatosis, cirrhosis, hepatitis) develop asymptomatically and are detected in late stages, as complications of the underlying disease.
- Pain syndrome . Not observed in all patients. Most complain of periodic diffuse abdominal pain during exacerbation of the disease. Pain is often caused by complications.
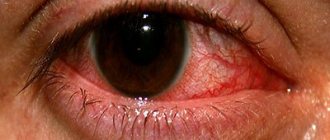
Celiac enteropathy may present with non-intestinal symptoms. The most common symptom is deterioration of the skin. The patient develops excessive dryness of the skin, often acne, and a tendency to dermatoses of various natures. Small blistering rashes are often found on the inner surface of the arms and thighs. The rash is located symmetrically on the body and is accompanied by itching.
Against the background of the disease, the functioning of the entire endocrine system changes. Often, autoimmune attacks spread to the thyroid gland. This causes infertility and problems with the gonads. Hormonal fluctuations can be a cause and consequence of the progression of celiac disease.
With gluten intolerance, vitamin D metabolism in the body is affected, which leads to impaired bone mineralization. Pathology predisposes to osteoporosis, excessive fragility of bone tissue, and the development of diseases of the musculoskeletal system.
In patients diagnosed with celiac disease, food allergies and bronchial asthma are more common. They may have problems with vision and hearing. Sometimes the nervous system suffers, problems with cerebral circulation, loss of coordination of movements, tremors, muscle weakness, nervousness, and causeless anxiety appear. Also, with intolerance, there is a tendency to extensive subcutaneous hemorrhages, periodontal disease and gingivitis, and stomatitis. A person’s stamina decreases, he gets tired quickly, and has difficulty withstanding physical activity.
Features of the course in children
Children with celiac disease differ from healthy children even in appearance. They have signs of dystrophy and constant lack of vitamins. Babies have a swollen belly, and their legs and arms look excessively thin. Young patients are prone to allergic skin reactions.
Children complain of abdominal pain. The stool contains not only fat, but also foam. Due to a lack of nutrients, the development of the musculoskeletal system is disrupted, signs of rickets appear, and the nervous system suffers. Such babies lag behind their peers in growth and development.
Important! Without proper treatment, celiac disease leads to exhaustion of the child's body, dehydration, and can be fatal.
Stages
Celiac disease is distinguished by stages, focusing on the severity of changes in the intestines. There are five of them in total:
- zero or preinfiltrative – the mucous membrane of the small intestine is not changed;
- first or infiltrative – inflammation develops, and a large number of lymphocytes are found in the biopsy;
- second or hyperplastic - the length of the intestinal villi does not change, but the crypts deepen;
- third or destructive - the villi atrophy partially (reversible process) or completely (irreversible changes);
- fourth or atrophic - the intestinal mucosa becomes thinner, erosions or tumors often form.
The stage of the disease is determined after examining a biopsy from the intestine. Without a biopsy, it is impossible to establish the nature and characteristics of changes in the epithelium.
Symptoms of celiac disease in adults
Although the disease is primarily associated with damage to the mucous membrane of the small intestine and the development of atrophy in it, in adults celiac disease manifests itself with mild symptoms from the gastrointestinal tract. An adult with celiac disease may experience:
- recurrent abdominal pain and diarrhea;
- anemia and weight loss for no apparent reason;
- unreasonable anxiety and irritability, prolonged depression and sudden mood swings;
- talking alone with oneself, performing actions atypical for a person, epileptic seizures;
- chronic fatigue syndrome - dizziness, increased sweating, paroxysmal shortness of breath, weakness and frequent headaches;
- anemia;
- female/male infertility, miscarriages;
- joint and muscle pain (in severe cases, osteoporosis and arthropathy develop, and fractures are common);
- secondary immunodeficiency - stomatitis, glossitis, dermatitis herpetiformis;
- multiple caries;
- constant thirst, every fourth patient develops type 1 diabetes;
- hemorrhages on the abdomen and limbs;
- intestinal bleeding (black stool); in advanced cases, lymphoma develops.
Can it leak hidden?
The latent form of celiac disease has mild symptoms. Intolerance causes low-grade inflammation in the intestines that does not manifest itself for years. Most of the symptoms are not associated with digestive disorders, and therefore are attributed to the patient himself (and even doctors) to temporary malaise, fatigue, and other diseases. The underlying cause remains unknown for many years. Often, complications are diagnosed first, and then celiac disease.
Useful information: Chronic pancreatitis: more than 10 symptoms, treatment (22 drugs) in adults, diet and surgery. What to do in case of exacerbation, attack of pancreatitis
Difficulties in diagnosis are also due to the variability of symptoms. Neurological disorders are much more often associated with pathologies of the nervous system rather than gastrointestinal diseases.
How is pathology diagnosed?
To diagnose celiac disease, a comprehensive examination is required. It consists of primary and secondary methods. The first include tests for specific antibodies (to gliadin, smooth muscle fiber proteins). The method is 97% specific for celiac disease and 93% reliable.
However, a positive result does not mean pathology. The presence of antibodies indicates a person's tendency to be gluten intolerant. The analysis can confirm sensitivity even if there are no symptoms of disease or organic changes in the intestines. This situation is observed in close relatives of a person with a typical form of celiac disease. They are recommended to be examined for quality monitoring of their health.
Secondary diagnostic methods include clarifying tests. With their help, the patient’s overall health condition is assessed, the presence of complications of the underlying disease, and enteropathy is finally confirmed. Additional diagnostic measures include:
- blood chemistry;
- Ultrasound of the liver, pancreas, spleen, thyroid gland;
- stool analysis;
- examination for helminthiasis;
- endoscopic examination of the esophagus, stomach, small intestine;
- intestinal biopsy (this study confirms the diagnosis);
- hormonal screening;
- pH-metry of the stomach;
- assessment of bone tissue condition;
- MRI of the intestine;
- colonoscopy;
- rectal biopsy.
All results are assessed as a whole. They provide additional information about the cause of the disease and help select high-quality comprehensive treatment.
Classification
| Explicit / classical | Clinical picture: clinic of enteropathy Laboratory diagnosis: positive serological tests, hyperregenerative atrophy (Marsh II-III) | |
| Atypical (nowadays more common than the typical form) | Clinical picture: manifestations of enteropathy are absent or minimal Laboratory diagnosis: atypical manifestations predominate - positive serological tests, hyperregenerative atrophy (Marsh II-III) | |
| Asymptomatic | Clinical picture: no clinical manifestations Laboratory diagnosis: positive serological tests, hyperregenerative atrophy (Marsh II-III) | |
| Potential (identification of this species remains debatable) | Clinical picture: no clinical manifestations Laboratory diagnostics: positive serological tests, positive genetic markers (HLA DO2/DQ8), mucosal architecture is not disturbed, the number of MEL is increased (Marsh I) | |
| Refractory (not typical for children) | Clinical picture: there are convincing clinical signs of celiac disease. Laboratory diagnosis: serological and histological signs of celiac disease, no response to gluten-free diet | |
Is there a cure for celiac disease?
Currently, there is no cure for the disease. Drug and auxiliary therapy help achieve temporary improvement in the patient's condition. The disease occurs with periodic exacerbations and relief of symptoms. Diet plays a significant role in the patient’s quality of life.
In the typical form, complete restoration of intestinal function is possible if a person completely eliminates gluten-containing foods from the diet. The diet is followed for life. In the torpid or refractory form, even diet is ineffective. The patient is prescribed medications, which also give only temporary results.
How appropriate are traditional methods of treatment?
Herbalists recommend that patients with celiac disease regularly use decoctions and infusions of medicinal herbs (thyme, chamomile, string, rose hips, currants, viburnum). In their opinion, such medications help relieve intestinal inflammation and reduce unpleasant symptoms.
Doctors and scientists say that traditional methods are not suitable for treating pathology. Herbs do not have the proper anti-inflammatory effect and do not affect the pathogenesis of the disease. In addition, with celiac disease the risk of allergies increases. With regular use of herbal preparations it increases.
The use of homeopathy, herbal medicines and plants should be agreed with your doctor.
Drug therapy
Treatment with medications is carried out for severe malabsorption syndrome and metabolic disorders. Therapy is symptomatic, aimed at improving the patient’s condition and optimizing the supply of nutrients to the body. With the help of medications, the intestinal microflora is corrected. For celiac disease the following is prescribed:
- enzymes (Creon, Pangrol, Panzinorm) - 1-2 capsules with each meal, to improve digestion and relieve stress on the pancreas;
- sorbents (Enterosgel, Atoxil) - prescribed to relieve intoxication of the body and remove toxins from the intestines;
- vitamins (B1, B6, nicotinic acid, folic acid, iron, calcium) - prescribed to optimize metabolism and replenish the deficiency of the most important nutrients;
- for disorders of the intestinal microflora, probiotics (Intetrix, Enterol, Bifilak) - to eliminate pathogenic flora and colonize beneficial ones;
- hepatoprotectors (Gepabene, Essentiale, Heptral) – if disturbances in the functioning of the hepatobiliary system are found, to optimize liver function;
- sedatives or antidepressants (prescribed on an individual basis if necessary).
Hormonal medications play a major role in the treatment of gluten intolerance. It is with their help that inflammatory processes in the small intestine are stopped and autoimmune reactions are suppressed. Hormones are prescribed if the body does not respond positively to the diet for 3 months. With their help, severe intestinal inflammation is stopped. For refractory celiac disease, hormone therapy is long-term. Most often, patients are prescribed Prednisolone for 1 week to 3 months. The drug is discontinued gradually.
The main thing is diet
Dietary nutrition is the basis in the treatment of celiac disease. In 90% of cases, the right diet helps to completely restore intestinal function and reduce autoimmune attacks.
Gluten and products containing it should be completely excluded from the menu of a person with celiac disease. The first on the list of prohibitions are cereals:
- wheat (and derivatives: flour, semolina, couscous, wheat groats, products with wheat starch);
- rye;
- oats;
- barley.
Gluten is found in many food products and may be included in the ingredients or listed as additives. This component is guaranteed to be present in:
- sausages;
- store-bought fermented milk products (yogurt, kefir, desserts, cheese curds);
- confectionery products;
- instant food products;
- sauces;
- semi-finished products.
Patients are advised to reduce their consumption of industrially processed foods as much as possible. Many cereals and desserts that should not contain gluten are contaminated with it during production. On the shelves of shops and supermarkets you should look for products with special marks: “gluten-free”, “suitable for celiac disease”. Gluten-free products are conventionally indicated by a crossed out ear of wheat.
Even without wheat and bread, the patient’s diet remains rich and varied. It can be used:
- homemade dairy products;
- all types of meat;
- eggs;
- rice, corn, amaranth, buckwheat;
- any vegetables and fruits.
To ensure a complete supply of nutrients to the body, it is recommended to adhere to a balanced diet and consume vitamin and mineral complexes.
Celiac disease treatment
Treatment of celiac disease in adults includes the following:
- For severe, long-lasting diarrhea, it is recommended to take antidiarrheal drugs, but this must be done with caution - do not take any coated tablets.
- In the case when the disease is already advanced, it is necessary to begin its treatment with intravenous administration of drugs containing nutrients into the body. At the same time, you need to switch to independent food consumption gradually and very slowly.
- It is necessary to additionally take medications with a high calcium content to avoid bone fragility.
- Drink multivitamin complexes, as well as preparations high in iron, vitamin B12 and D. It is recommended to drink folic acid.
- It is advisable to regularly see an allergist-immunologist.
- Due to the fact that a person with celiac disease is often exposed to stress and irritability, consultation with a psychotherapist may be required.
- Treatment for celiac disease must be accompanied by a strict diet.
- A patient who has been diagnosed with celiac disease must for the rest of his life abstain from foods made from wheat, rye, oats, semolina and barley. Wheat flour can be replaced with buckwheat, corn, rice or soy. Almonds and sorghum are also good substitutes - they can also be ground into flour.
- It is necessary to limit the consumption of sausages and smoked products, reduce the amount of canned food, chocolate, ketchup and mayonnaise consumed. You should not eat foods that are too salty, spicy or fatty. Drink less coffee and cocoa.
- It is prohibited to drink beer and eat foods that contain malt.
- Eat more meat, fish, potatoes, rice and fruits.
Improvement in intestinal health occurs after 4-5 months from the start of the diet. It may take one year or more for the body to fully restore the intestines.
Even after being completely cured, you should not forget that you must always follow a gluten-free diet.
If you follow all the specialist’s recommendations, you can achieve a standard of living at which a patient diagnosed with celiac disease will be no different from a completely healthy person.
Scientific research
The journal BMJ Open Gastroenterology published the results of cohort studies that compared the clinical features of celiac disease in patients with seropositive and seronegative types (with and without antibodies). Participants were selected based on characteristic symptoms, serological test data, and histological examination of small intestinal biopsies.
Celiac disease of the seronegative type is still the subject of debate among doctors and scientists. Some luminaries believe that the characteristic symptoms of the disease without a positive serological test are not a reason for diagnosing celiac disease. Another part believes that this is a separate type of disease.
According to information obtained during the selection of participants, abdominal syndrome was more pronounced in seronegative patients than in seropositive patients. People with genetically determined celiac disease (seropositive) had significant changes in the intestinal mucosa. Both groups were put on a gluten-free diet for a year.
Improvement in condition after starting the diet was noted in all patients. According to histology results, after a year, the intestinal mucosa was completely restored in seronegative patients (while in seropositive patients it did not). In such patients, the diet has a positive effect on metabolic processes and the degree of absorption of nutrients. They are much less likely to develop anemia and extraintestinal manifestations of celiac disease. After the gluten test, 25% of participants experienced an exacerbation of the disease (with increased symptoms and a clear deterioration in condition).
Research results indicate the need for a gluten-free diet for seronegative and seropositive patients. However, in the first case, diet may be the only method of treatment, and in the second - the main one, with the obligatory prescription of symptomatic and drug replacement therapy.
Diagnostics
Diagnosing celiac disease is quite problematic. In most cases, even the clinical picture does not give complete confidence that a person has celiac disease. After all, all the symptoms are easily confused with banal inflammatory processes in the gastrointestinal tract. In the sixties of the last century, several criteria were proposed that best characterize the disease:
- intolerance to gliadin (wheat gluten);
- the active phase of the disease is accompanied by atrophy of the villi of the intestinal mucosa;
- the mucous membrane is restored with a gluten-free diet;
- repeated introduction of gliadin into food leads to further villous atrophy.
Modern forms of diagnosis include serology, which indicates the presence of a number of specific antibodies in the blood. Next - endoscopy and biopsy of the intestinal mucosa. The latter test is often done in two stages: a biopsy is taken, and then the procedure is repeated after the patient has taken a dose of gluten. In some cases, a stool examination is performed.
To date, there is no single complete method for diagnosing the disease.
This is interesting!
In the world of scientists and doctors, celiac disease is considered a multifactorial disease. The increase in the number of patients is associated not only with genes, but also with environmental factors. It has been proven that intolerance occurs more often in children who were given early complementary foods with a predominance of gluten-containing products.
Today, there is unofficial statistics that 1 person out of 100 is sensitive to wheat protein. As a rule, these are patients with a latent course of the disease. The full clinical picture is much less common (1 case per 2000 people). Among the patients, children and women predominate. They are followed by older men (over 50 years old).
Causes
The causes of celiac disease can be divided into external and genetic
. External factors include excess gluten in food. But the role of genetic factors is currently well studied. Statistics and numerous studies indicate that this disease is ten times more common among relatives.
It can be argued that the disease is genetic, as it is caused by the presence of certain changes in some factors of the HLA set of genes, which are responsible for recognizing foreign molecules in the body. This is one of the most common causes currently identified, although it is not considered sufficient.
Forecast
The diagnosis of celiac disease makes adjustments to the patient’s lifestyle. He will have to monitor his diet and carefully “filter” the foods on his table. Otherwise, there will be no fulfilling life. If diet therapy and medications improve things, it is important not to provoke relapses. The more often they occur, the higher the risk of small intestinal cancer. Complications of the disease worsen the quality of life and prognosis for the patient as a whole.
If celiac disease is detected and its course is favorable, the patient should undergo preventive examinations annually. If the disease develops unfavorably, frequent examinations and long-term medication will be required.