What is exophthalmos
The disease manifests itself as bulging eyes. As the pathology develops, the eyeballs protrude slightly forward. In rare cases, they move from the eye sockets not only forward, but also to the side. In this case, the diameter does not change, the pupil does not visually enlarge. This symptom is caused by swelling of the soft tissues of the eye: they swell and “push” the eyeball forward.
Swelling of the orbital tissue occurs due to inflammation, including those caused by ophthalmological diseases. In the final stages of the pathology, the eyes begin to pulsate. Exophthalmos is rare. Bulging eye syndrome affects both children and adults.
Exophthalmos (bulging eyes)
- Pain in the eyes
- Protrusion of eyes
- Double vision
- Inability to completely close eyelids
- Limitation of eye mobility
- Swelling of the eyelids
- Redness of the eyes
- Loss of vision
- Pulsation in the eye area
- Decreased vision
- Dry eyes
Exophthalmos or bulging eyes is a pathology of the eyeball in which it protrudes forward beyond the level of the orbit, and sometimes to the side. Typically, this condition is a symptom of other diseases - ocular or non-ocular, therefore, if exophthalmos appears in a person, one should urgently consult a doctor and undergo examinations to determine the causes of the development of the disorder.
- Causes
- Symptoms
- Diagnosis and treatment
This pathology is popularly called bulging eyes, and it can be a congenital feature of a person. At the same time, congenital exophthalmos is bilateral in nature and is characterized by unexpressed symptoms, while acquired exophthalmos can be either unilateral or bilateral, and its manifestations are quite clearly expressed. Bug eyes can progress over years, with increasing symptoms, or develop in just a few weeks, and both men and women of any age, and even children, can suffer from the disease.
Redness of the eyes.
Why is eye protrusion dangerous?
If corrective measures are not taken in a timely manner, the disease leads to complete blindness. The tumor increases in size and constantly puts pressure on the optic nerve, which leads to its atrophy. At the first symptoms of the disease, including visual ones, you must immediately contact an ophthalmologist.
Another negative factor is that exophthalmos is not an independent syndrome. It serves as a sign of endocrine, immune and inflammatory diseases, delay in which can lead to complications, including infertility and disruption of vital organs.
Treatment
The treatment regimen is determined based on the causes of this disease, as well as the degree of its severity. If the cause of development is hormonal in nature, then correction of hormone levels is carried out by prescribing glucocorticosteroid drugs. If the disease is inflammatory, antibacterial and anti-inflammatory therapy is used; in severe cases, surgery is performed. In cases where the oncological cause of the disease is established, chemotherapy, radiation therapy, and surgery are used in treatment.
Types of exophthalmos
Before treatment, it is necessary to carry out differential diagnosis. To choose the right complex, you need to determine what triggered exophthalmos.
According to the clinical picture:
- Unilateral. Only one eyeball protrudes.
- Bilateral or binocular. Eye protrusion is observed on both sides.
By nature of occurrence:
- Imaginary. Diagnosed with congenital asymmetry, abnormal enlargement of the eyes caused by another disease.
- True (non-specific). It can be traumatic, varicose or inflammatory. The tissues swell, begin to increase in size, and pulsate.
- Hypothalamic-pituitary. Refers to hormonal forms. The hypothalamus and pituitary gland produce large amounts of hormones.
Articles on the topic
- Anisocoria of the pupils in children and adults
- Release of bile into the stomach - signs, drugs and treatment methods
- The second stage of alcoholism - causes, detoxification and therapy
Exophthalmos - Description, Causes, Treatment
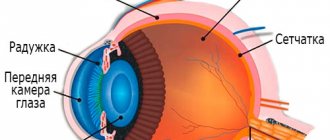
Exophthalmos is a protrusion of the eyeball forward. The cause of exophthalmos is swelling of orbital tissues, mainly in the retrobulbar space, and an increase in their volume. This pathological condition can be observed against the background of inflammation, eye injury, volumetric processes, and neurodystrophy.
Among the factors provoking exophthalmos, local and general ones are distinguished. The most common are hydrocephalus, toxic diffuse goiter, hypothalamic syndrome, diseases of the paranasal sinuses, etc.
Exophthalmos can be true or false.
Prevention of exophthalmos
The main rules of prevention are a healthy lifestyle and giving up bad habits. The daily diet should contain the required amount of vitamins and microelements. If you suspect the development of ophthalmological diseases, an examination by a doctor is required. After a full examination, the correct treatment is prescribed.
How does bulging eyes manifest in humans?
Pulsating exophthalmos is accompanied by a strong displacement of the eyeballs forward and to the side (rarely). In addition, the following symptoms are characteristic:
- pulsation of the eyeballs during visual examination;
- white gap between the eyelid and the iris;
- darkening of the skin of the eyelids;
- difficulty closing the eyes in severe cases of the disease;
- dryness, constriction of the pupils, feeling of sand;
- difficulty moving the eyes, pain when trying to look to the side;
- active double vision, rapid deterioration of vision;
- headaches caused by pressure on a nerve;
- painful reaction to light;
- increased fatigue, frequent dizziness, drowsiness;
- drying, corneal atrophy.
The disease occurs in three stages:
- First degree. Visually, symptoms do not appear.
- Second degree. Movement is complicated, strabismus (squint) develops.
- Third degree. There is no way to close the eyelids.
Types of bulging eyes
Types of exophthalmos are classified as follows:
- unilateral (the disease affects only one eye);
- bilateral (protrusion of both organs of vision is observed);
- axial (protrusion occurs only relative to the central visual axis and the eyeball does not shift to the sides);
- true (pathology developing in diseases of endocrine origin, which occurs in acute or chronic forms);
- imaginary (the eyeball protrudes due to congenital ophthalmological pathologies such as asymmetry of the orbits or glaucoma, as well as severe myopia and abnormalities in the structure of the skull).
Causes of eyeball enlargement
Exophthalmos is not an independent disease, but a complication caused by other pathologies. The most common reasons:
- Hydrocephalus is an accumulation of fluid in the brain.
- Graves' disease (endocrine ophthalmopathy) is a disorder of the thyroid gland, characterized by tremor and tachycardia.
- Oncological diseases of the orbit, brain and cerebellum.
- Thrombosis and aneurysm of cerebral vessels.
- Sinusitis, other pathologies of the nasal sinuses.
- Injuries to the eye shell.
Risk factors for developing pathology
Exophthalmos is a rare symptom, but for people at risk, it is better to periodically visit an ophthalmologist and carry out all the necessary examinations.
Be sure to visit a neurologist periodically. It is recommended to take an X-ray of the brain after any injury, even minor.
Risk factors for developing the disease are as follows:
- smoking;
- poor diet, iodine deficiency;
- lesions of the ocular membrane of a traumatic nature;
- physiological protrusion of the eyes;
- exophthalmos suffered in the past.
Forms of the disease
Keep in mind! Exophthalmos can manifest itself in one of the following forms:
- Pulsating . The disorder occurs as a result of traumatic brain injuries, eye injuries, and aneurysms of the vessels of the visual organs. A distinctive feature of the disease is the patient’s sensation of pulsation in the affected eye.
- Thyrotoxic . It occurs as a side symptom of Graves' disease and mainly develops in both eyes, although with a possible delay in one of the visual organs. The mobility of the eyeballs in this case is usually not impaired even with strong protrusion of the eyeballs. This form received its name because of thyrotoxicosis, which is a contraction of the muscle located in the inferior orbital fissure. This contraction, in turn, occurs when the tone of the sympathetic nervous system increases. In this case, the patient experiences widening of the palpebral fissure, which leads to the appearance of a strong protrusion of the eyes.
- Edema . This form of exophthalmos appears due to immune pathologies, which result in an autoimmune attack of the eyes and disturbances in the functioning of the thyroid gland. In this case, protrusion occurs sharply, and the patient experiences visual impairment due to the development of swelling in the tissues of the eye (in particular, people with this form of the disease complain of double vision). The pathology can be either unilateral or bilateral, while endocrine lesions may not be observed. Most often, this type of disease develops not against the background of pathological changes, but due to intoxication, radiation, and even severe stress experienced.
Treatment of exophthalmos
If edematous exophthalmos is of a traumatic nature, the patient is indicated for canthotomy. The outer corner of the eye and the commissure of the eyelids are incised to temporarily widen the palpebral fissure. Using surgery, doctors remove tumors, “set” displaced bones, and get rid of foreign bodies.
For the hypothalamic-pituitary form, therapy is carried out with thyreostatics ( Thiamazol. Propylthiouracil ) and hormones. The choice of means depends on the gender of the patient and the cause of hormonal imbalance. During treatment, it is necessary to carry out maintenance procedures: regularly moisturize the eye shell using special drops with the effect of artificial tears.
If unilateral exophthalmos is caused by autoimmune pathologies, ophthalmopathy, therapy with glucocorticoids ( Betameson, Prednisolone ) is prescribed.
In addition to protruding eyes, the disease that caused a similar syndrome is treated - cancer, thyroid dysfunction, and so on.
In rare cases, radiotherapy is used. A pressure bandage may be applied to the affected eye. The most radical method is ligation of the carotid artery. Exophthalmos is treated only by doctors - an ophthalmologist and an endocrinologist. Self-medication is dangerous to health!
Causes of exophthalmos
With endocrine ophthalmopathy, disturbances in the functioning of the human immune system are observed. The subcutaneous fatty tissue of the eye orbits swells, and the same happens to the muscles of the eyeball. If the disease begins to be treated at this stage, then significant improvement can be achieved and the eyeball can be returned to its physiological position.
As the pathology progresses, the extraocular muscles become injured and scar tissue forms on them. Such changes are irreversible.
In Graves' disease, against the background of autoimmune thyroiditis, retrobulbar tissue is damaged. The body's own antibodies attack not only the thyroid tissue, but also the tissue of the orbit. Proof of this theory of the development of exophthalmos is the high level of antibodies to thyroid-stimulating hormone receptors.
Antibodies to the muscles of the oculomotor system will be produced in the body more if it is influenced by the following risk factors:
- Emotional shock.
- Past viral infections.
- Poisoning of the body.
- Impact of radiation on the body.
- Genetic predisposition to the development of thyroid diseases.
An inflammatory process occurs inside the orbit against the background of exophthalmos. When fatty tissue is involved, or the patient develops vascular vasculitis, the eye orbits bulge forward due to mechanical pressure on them.
Rare causes that can provoke exophthalmos include:
- Dacryoadenitis.
- Tumors of benign nature.
- Cancerous tumors.
- Skull injuries with bone displacement and hemorrhage into the orbital cavity.
- Phlebeurysm.
- Angiopathy.
Prognosis and prevention
Even with proper treatment, exophthalmos returns. Therefore, patients with an appropriate entry in the medical record must:
- Regularly visit an ophthalmologist or neurologist.
- Adjust your diet. The diet should contain foods rich in vitamins and microelements.
- Treat all problems associated with blood vessels and varicose veins in a timely manner to prevent the disease.
- Do not cause inflammatory eye diseases, including bacterial infections of the orbits.
- Carry out regular self-examination and examination of the child to detect exophthalmos in the early stages.
Is it possible to protect yourself from exophthalmos in one eye? Causes of the disease
Unilateral exophthalmos is a pathological condition in which one eyeball noticeably moves forward , and the motor function of the visual organs deteriorates.
The patient also develops strabismus .
ontakte
Odnoklassniki
Exophthalmos of one eye develops due to injury to this organ. Especially if such damage was accompanied by hemorrhage on the cornea . In this case, the disease does not spread to the second eye.
Due to heredity, the disease may only affect one eye. If patients have protrusion of one visual organ, then there is a high probability of developing exophthalmos in their children or grandchildren.
Abnormal development of the skull in the upper part and only on one side. Then exophthalmos is expressed from birth or infancy and grows over the years.
In some cases, a disease of one eye becomes only the initial stage of an illness that affects both organs of vision. Then the reasons are:
- inflammatory processes in the body;
- disturbances in the functioning of the endocrine system (for example, the appearance of goiter);
- paralysis of the eye muscles;
- fungus or parasitic cysts;
- vascular disorders.
Reference! The cause of exophthalmos is asymmetry of the face or some part of the skull. Such a deviation may be invisible to the naked eye and not show itself in any way for decades. The disease will begin to bother you only at the age of 40-45.
Symptoms of unilateral pathology
The patient has a forward displacement of one eye, noticeable during a routine examination. It causes discomfort, reduces visual acuity, and does not allow the eye to move freely in the socket.
Attention! Due to the inability to completely close the eyelid, the cornea is left partially unprotected, damaged or dried out. occurs .
intraocular pressure increases , which is accompanied by disturbances in the vascular system and the appearance of a red eye effect. Due to the pressure placed on the orbit, the optic nerve is compressed and atrophies. This causes a sharp deterioration in vision, up to complete blindness.
Photo 1. The main symptom of exophthalmos is a noticeable displacement of the eyeball forward, while it is impossible to completely close the eyelid.
The patient suffers from constant tearing from one eye and feels a cutting pain, especially in bright light. The person also experiences general weakness, insomnia, and psychological disorders. The body's metabolism and water-salt balance and normal thermoregulation are disrupted.
Treatment
The success of treatment of exophthalmos depends on the correctly identified cause of the pathology and the degree of its development. Medicines can be prescribed not only by an ophthalmologist, but also by other attending physicians - to provide a complex effect and get rid of the preconditions of the disease.
Medication
If the cause of the disease is disruption of the endocrine system, the doctor prescribes microdoses of iodine and Mercazolil.
The duration of such therapy is determined in accordance with tests showing the level of thyroid hormones, and is at least 2 weeks .
During this treatment, the patient constantly undergoes examinations, which allows us to determine the exact duration of therapy and its effectiveness.
Taking medications containing corticosteroids will help relieve the main symptoms of the disease. is prescribed daily for 6-7 days at the rate of 1 mg per kilogram of weight.
Then the patient is gradually transferred to taking this drug every other day and in this form for a month.
If exophthalmos has led to inflammatory processes in the orbit, the person is prescribed broad-spectrum antibiotics: streptomycin sulfate or others.
Admission is carried out for 2 weeks simultaneously with anti-inflammatory drops.
Such treatment, as prescribed by a neurologist, is accompanied by the use of sedatives, vitamins, and infusion of glucose solution to maintain the overall health of the body.
The socket or orbit is the bony container for the eye..The anterior part of the orbit contains the eyeball, and the posterior part contains the optic nerve and muscles. ,blood vessels, nerves And fatty tissue .Orbital inflammation.
1. Orbital phlegmon
. This is a purulent inflammation of the orbital tissue.
Main etiological reasons:
1. Infections of the paranasal sinuses.
2. Inflammation of adjacent structures: chronic purulent dacryocystitis, infection of the facial and dentofacial area.
3. Post-traumatic phlegmon, which usually develops within 48-72 hours after injury. In some cases, typical clinical symptoms may be masked by trauma-related retrobulbar hematoma.
4. Postoperative phlegmon. May complicate surgery for retinal detachment, strabismus, dacryocystorhinostomy, and orbital surgery.
Pathogens of orbital phlegmon
.
Streptococcus, staphylococcus, Haemophilus influenzae, etc.
Clinical signs
include rapid onset, headache, fever, orbital pain, nausea, and in some cases general weakness. Pain in the eye increases with movement of the eye or pressure on it. The eyelids are swollen, hyperemic, warm to the touch and painful on palpation. Chemosis of the conjunctiva is noted. On the part of the eye - proptosis. Eye movements are limited and painful. In the early stages, visual acuity may be reduced.
Possible complications:
1. Intracranial complications include meningitis, cerebral abscess and cavernous sinus thrombosis. Signs of cavernous sinus thrombosis: swelling of the skin of the eyebrows, forehead. Enlarged veins on the forehead. Bilateral exophthalmos with complete immobility of the eyeballs, which is associated with lesions in the cavernous sinus of pairs 3, 4, 6 (n. oculomotorius, n. abducens, n trochlearis). In the cavity of the cavernous sinus, 1 branch of the trigeminal nerve is affected - absence of the corneal reflex. Possible: congestive disc, thrombosis of the central retinal vein, thrombosis of the orbital veins. Cerebral symptoms and meningeal symptoms appear.
2. Subperiosteal abscess (this is relatively rare with pathology of the paranasal sinuses, but can also occur after injuries and in the postoperative period).
3. Ocular complications (keratopathy, increased IOP, obstruction of the central retinal artery or vein, optic neuritis).
Treatment of
orbital cellulitis
is an emergency requiring hospitalization.
1. Intensive antibiotic therapy (parenteral and local therapy with broad-spectrum antibiotics). Antibiotics of various groups are used in large doses. Penicillin group - amoxicillin, ampiox, oxacillin.. First generation cephalosporins - cefazolin, cefamezin, second generation - cefamabol, third generation - cefatoxime, cephabol, claforan. Antibiotics of the macrolide group - sumamed, macropen, rulid. Fluoroquinolones – ciprofloxacin, nolitsin, ofloxacin
2. Sulfonamides - biseptol, sulfadimethoxine, sulfalene.
3. Analgesic and anti-inflammatory drugs to reduce pain and fever.
4. Osmotherapy (40% glucose solution IV)
5. Vitamins
Surgical treatment: should be used in cases of no effect of antibiotics, decreased vision, or the presence of an orbital or subperiosteal abscess. A through incision should be made according to the abscess when it is located under the skin or conjunctiva. In most cases, it is necessary to open and drain the orbit in the lower outer sections. Mandatory opening of infected paranasal sinuses.
Other types of orbital inflammation: orbital osteoperiostitis and tenonitis.
2. Orbital periostitis
- inflammation of the periorbital periosteum. The surrounding bones may become involved and orbital osteoperiostitis may develop. This may develop as a result of injury or infection of surrounding structures.
The clinical picture can take two forms.
Anterior orbital periostitis - this involves the orbital margin and is characterized by severe pain and swelling in the area of inflammation. Once a subperiosteal abscess has formed, it often ruptures at the surface of the skin.
Posterior periostitis is characterized by deep orbital pain, exophthalmos, and slight limitation of eye mobility. Sometimes there may be anesthesia of the skin of the eyelids and cornea.
3. Tenonitis
is an inflammation of Tenon's capsule, usually unilateral. It is characterized by pain that increases with movement of the eyeball, moderate exophthalmos, moderate chemosis and swelling of the eyelids.
The main etiological factors are inflammation of the ocular structures, damage to Tenon's capsule, postoperative tennonitis.
Principles of treatment of inflammatory diseases of the orbit
1. Intensive therapy with antibiotics, which are mentioned above (subconjunctival, retrobulbar and systemic administration).
2. Analgesics and anti-inflammatory drugs.
3. Surgical drainage
4. Physiotherapeutic treatment.
Exophthalmos.
Exophthalmos (Exophthalmos or proptosis) is defined as a displacement of the eyeball anteriorly from the orbital rim.
It can be one-sided or two-sided.
Causes of bilateral exophthalmos
:
1. Congenital anomalies of the skull (tower skull, craniofacial dysostosis)
2. Inflammatory conditions (Mikulicz syndrome and the last stage of cavernous sinus thrombosis)
3. Endocrine exophthalmos (thyrotoxic or edematous)
4. Tumors
5. Systemic diseases (amyloidosis, Wegener's granulomatosis)
Causes of unilateral exophthalmos
:
1. Congenital conditions (cyst, dermoid, orbital teratoma)
2. Trauma (orbital hemorrhages, foreign bodies)
3. Inflammatory diseases of the orbit (orbital phlegmon, abscess, thrombophlebitis, cavernous sinus thrombosis)
4. Orbital cysts
5. Orbital tumors (primary, secondary or metastatic)
Orbital tumors.
Orbital tumors are not very common. These include primary, secondary and metastatic tumors. The classification includes vascular tumors, lacrimal gland tumors, cysts, neural tumors, epithelial and some others.
The main signs of orbital tumors:
Progressive exophthalmos. The degree of exophthalmos depends on the location and size of the tumors. May range from moderate to pronounced. At the same time, there is a restriction in eye movement.
Decreased visual acuity, diplopia, and central scotoma are often observed. Ophthalmoscopy may show papilledema, optic nerve atrophy, retinal hemorrhage, and sometimes retinal detachment. In the last stage, IOP may increase and a corneal ulcer may develop.
Another sign of orbital tumors is the absence or decrease in reposition of the eyeball during palpation (palpation should be performed to assess the compressibility of the tumor).
X-ray examination of the orbit is one of the most important studies. In some cases, it is very useful to use orbital venography, carotid vasography, radioisotope diagnostics, scanning, ultrasonography and magnetic resonance imaging.
It is very important to determine the type of orbital tumor - benign or malignant. The rate of tumor growth may vary. Benign tumors
grow more slowly than malignant ones.
The main benign tumors of the orbit: dermoid cysts, capillary hemangioma, osteoma.
Capillary hemapgioma is the most common tumor of the orbit and periorbital region in children. It appears as a lump in the front of the orbit and tends to increase in size when stressed or screamed. Hemangiomatous tissue may be seen in the conjunctival fornix when the eyelids are everted.
Cavernous hemangioma is the most common benign orbital tumor among adults. The tumor is usually located in the retrobulbar space in the muscular infundibulum.
Dermoid cysts are developmental tumors that result from germinal displacement of the epidermis to a subcutaneous location. They manifest themselves as a limited neoplasm in the superotemporal or superonasal part of the orbit. Displacement of the eyeball is not noted, since they are located in front of the orbital septum. This tumor does not extend deep into the orbit and is not associated with bone defects.
Treatment for benign tumors is usually surgical. Surgical removal of the tumor is performed using orbitotomy. Since the tumor is easily accessible, its complete removal is possible.
Malignant tumors
: sarcoma, cancer.
Rhabdomyosarcoma is a highly malignant tumor of the orbit that develops in the extraocular muscles. It is the most common primary orbital tumor among children, usually occurring before the age of 15 years. Sometimes clinical manifestations resemble an inflammatory process. It can develop in any part of the orbit.
The cancer is usually a metastatic orbital tumor that spreads hematogenously to the orbit from a distant primary site (lung, breast, prostate, thyroid, and rectum). In some cases - from the skin of the eyelids, conjunctiva, lacrimal ducts.
Treatment:
1. Radiation therapy in combination with general treatment.
2. Chemotherapy
3. Surgical treatment – orbital exenteration
Superior orbital fissure syndrome
The superior orbital fissure is located between the lesser and greater wings of the sphenoid bone. Many vessels and nerves pass through the superior orbital fissure: the superior orbital vein, oculomotor, abducens and trochlear nerves, the first branch of the trigeminal nerve. When the apex of the orbit is involved in the case of an orbital tumor, retrobulbar hematoma, or foreign bodies, the typical picture of superior orbital fissure syndrome develops. It includes: moderate or severe exophthalmos, partial or complete ptosis, general ophthalmoplegia, mydriasis, paralysis of accommodation, anesthesia in the area of innervation of the first branch of the trigeminal nerve.
Treatment depends on the cause of the syndrome.
Diagnostics
Exophthalmos is diagnosed during an ophthalmological examination, during exophthalmometry, when the localization of the eyeballs is assessed using special mirrors.
As an addition, computed tomography or magnetic resonance imaging may be prescribed to clarify changes in the orbit that can cause exophthalmos.
In addition, confirmation of the diagnosis requires laboratory tests to establish the behavior of the immune system in relation to its own tissues and organs, as well as the level of thyroid hormones, because the main cause of exophthalmos is often endocrine ophthalmopathy.
Symptoms
Before describing the symptoms of a pathology such as bulging eyes, you should understand what forms of it are found in modern medical practice. There are four such forms.
The first is imaginary exophthalmos , which develops due to structural anomalies of the skull and orbit, as well as due to congenital pathologies such as glaucoma or severe myopia.
The second form is true goggle eyes . It is spoken of in cases where the disease is caused by endocrine disorders or tumor-like and inflammatory processes in the orbit.
The third form is intermittent . It occurs when a person tilts his head - this occurs as a result of damage to the vessels of the orbit, for example, with varicose veins.
The fourth form of such a pathology as bulging eyes is pulsating . It is manifested by a pronounced pulsation of the eyeball, which at its peak strongly protrudes forward, and then returns to the confines of the orbit. This condition occurs in people who have an orbital aneurysm or suffer from cavernous sinus thrombosis.
Separately, you should pay attention to such a pathology as edematous exophthalmos . This disease develops mainly in people after 40 years of age and has a malignant course, characterized by severe symptoms with impaired mobility of the eyeball and a decrease in the quality of vision, up to its complete loss due to compression of the optic nerve by edematous tissue. Develops with diffuse toxic goiter as a consequence of hormonal imbalance in the body.
Edematous exophthalmos is expressed by severe protrusion, even dislocation, as well as excessive pain syndrome - the pain in some cases cannot be relieved even with narcotic drugs. Treatment of such a disease should be surgical - in most cases, decompressive trepanation of the orbit is indicated in order to return the eye orbit to its place and stop pain and other severe manifestations.
Symptoms of the disease depend on the stage - a barely noticeable protrusion does not cause discomfort to a person and may not even be visible to the naked eye and can only be determined using special instruments. When bulging eyes are pronounced, it gives a person not only physical, but also psychological discomfort, since the eyes are in plain sight, and others always pay attention to them when communicating with a person, which is why the patient experiences awkwardness and other negative feelings. Therefore, the sooner a person seeks medical help, the faster he can cure the disease and return to normal life.
If the disease is advanced, exophthalmos progresses and the following symptoms develop:
- swelling of the eyelids;
- decreased vision;
- redness of the sclera;
- double vision.
Another symptom characteristic of bulging eyes is the inability to close the eyelids, which causes the conjunctiva to dry out and develop inflammatory-dystrophic changes in it.
In cases where the patient has unilateral exophthalmos, there is a high probability that it is caused by a tumor in the orbit. Restricted mobility of the eyeball or its complete absence is a characteristic sign of tumor pathology. If the pathology is not cured at this stage, compression of the optic nerve may occur, resulting in symptoms such as impairment, and then complete loss of vision without the possibility of recovery.