Classification
It would seem that in the context of modern medical advances and mass immunization, the problem of parenteral hepatitis should not exist at all. But I regularly encounter patients who did not even know that they had such an infection, and yet they pose a huge danger not only to the population, but also to their loved ones.
Any information is perceived much easier when it is organized. Therefore, first of all, I would like to introduce you to the main classifications.
Parenteral hepatitis can be divided as follows:
- By etiology:
- viral hepatitis B (HBV);
- type D (delta, possible only in the presence of type B antigens);
- type C;
- mixed hepatitis (mixed infection, for example, B+C);
- unspecified;
- By phase/stage:
- exacerbation;
- remission;
- By clinic:
- icteric form (cytolytic or cholestatic). It occurs most often and is characterized by the appearance of corresponding staining of the skin and mucous membranes due to the increased content of bilirubin in the blood;
- anicteric. With this variant of hepatitis, there are no manifestations of hyperbilubinemia, the disease is nonspecific (indigestion, weakness, increased fatigue);
- erased, innaparent (no symptoms, biochemical parameters are normal, but there are markers of hepatitis);
- subclinical (asymptomatic form, but markers of viral hepatitis are detected in the blood in combination with changes in biochemical parameters);
- By duration:
- acute course (up to 3 months);
- prolonged (over 3 months);
- recurrent (with exacerbations), cyclical;
- chronic (more than 6 months);
- By activity:
- mild;
- medium-heavy;
- heavy;
- malignant (fulminant or fulminant).
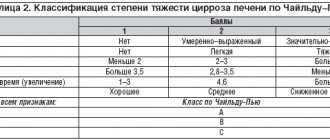
According to modern standards, when formulating a diagnosis, I always indicate whether there are complications (coma, cirrhosis of the liver, chronic hepatitis, carcinoma).
Tasks and goals of prevention
To prevent viral hepatitis from spreading, epidemiology and prevention must be followed.
Epidemiological surveillance performs the following tasks:
- Informational.
- Diagnostic.
- Managerial.
Epidemiologists do all this work. After analyzing the situation and collecting information, diagnostics are carried out and emergency decisions are made. A forecast of morbidity and a plan for the development of programs that will reduce the number of cases are also drawn up.
I would like to note that the goal of hepatitis prevention is to reduce the risk of infection when:
- Carrying out surgical interventions.
- During hemodialysis.
- During blood transfusion.
And also reduce the spread of viral hepatitis A and reduce the number of cases.
Viral hepatitis B and D
Parenteral hepatitis caused by type B virus (HBV) is an anthroponotic disease that leads to inflammatory damage to liver cells. That is, only people can get sick from it. Moreover, only 10-100 particles are enough for infection, which are very stable in the environment.
I would like to emphasize that the hepatitis B virus is prone to mutations (it has more than 60 strains and 8 genotypes). Its high prevalence is dangerous not only for the population, but also for states as a whole.
Identification of viral hepatitis D (HDV) is possible only if there is co- or superinfection against the background of existing HBV. The modes of transmission and preventive measures for them are the same, except that a vaccine against HDV has not yet been developed.
Transmission routes
The source of HBV and IOP can be a patient with acute or chronic form, as well as a virus carrier.
Infection occurs through the following parenteral routes (hence the name of this group of hepatitis):
- sexual (traditional, anal and even oral sex, as well as the use of shared intimate devices). Viral particles are found in blood, semen and vaginal secretions;
- from mother to fetus in utero or during childbirth;
- artificial (during transfusion of blood products, using shared syringes, going to the dentist or nail salon, operations, poor quality piercing, home tattoo).
Symptoms
In my practice, the cyclic course of HBV is more common. The incubation period (time from the onset of infection to the appearance of the clinic) is 40-180 days (2-4 months). If there is co-infection with the delta agent (AD), it is reduced to 3-10 weeks, and subsequent clinical manifestations are more severe.
Typically, symptoms develop over the following periods:
- Pre-icteric (initial) – 1-5 weeks. There may be any prodromal signs of infection, which, unfortunately, are not specific: a feeling of weakness, indigestion (nausea, bad taste), abdominal discomfort (usually on the right), increased body temperature more than 38oC, sleep problems, rashes, muscle pain . Sometimes dark urine and light-colored feces are noticed. Objectively, the liver and/or spleen may be enlarged.
- Jaundice – 2-6 weeks. The liver continues to increase in size, feces are discolored, and urine is dark. The main symptom is the same coloring of the skin, sclera and mucous membranes (clearly visible in the oral cavity and conjunctivae). With increasing intoxication due to damage to hepatocytes, weakness increases, appetite is lost, and cases of fainting are common.
- Convalescence (recovery) – up to 6 months. The condition gradually improves, jaundice disappears and laboratory parameters normalize. Otherwise, the process becomes chronic.
Although we most often record the icteric form of HBV, epidemiological data indicate the predominance of anicteric and erased variants. People in the absence of severe symptoms simply do not go to the doctor.
Diagnostics
Even if I observe a typical clinical picture of viral hepatitis B, I cannot make a diagnosis without laboratory confirmation.
For this purpose, the following standard and special studies are mandatory:
- Standard: general clinical analysis of blood and urine, biochemical parameters (ALT, AST, de Ritis coefficient, glucose, alkaline phosphatase, GGTP, total bilirubin and its fractions, assessment of coagulation);
- Special:
- determination of HBsAg, anti-HBc IgM, HBeAg, anti-HBc IgG, HBV DNA;
- serum markers of IOP – anti-delta IgM and IgG, HDV RNA;
- Additional (to exclude other etiologies or in case of an atypical form): protein fractions, ELISA/PCR for HIV infection, blood electrolytes, urine diastasis, ultrasound/CT/MRI of the abdominal organs, ECG.
Treatment
Hepatitis with parenteral transmission is usually treated comprehensively.
The following principles exist for the treatment of HBV (+/- IOP):
- Non-drug measures: dietary nutrition, bed rest (for moderate cases and worse), drinking plenty of fluids (at least 1.5-2 l/day).
- Infusion therapy (to reduce intoxication): polyionic solutions, glucose, Reamberin.
- Parenteral nutrition for patients in critical condition (they are usually transferred to the ICU - intensive care unit).
- Normalization of blood properties: plasma-substituting solutions, “Etamzilat”, “Vikasol”;
- Broad-spectrum antibiotics: cephalosporins (III-IV generations) and fluoroquinolones;
- For cholestasis: "Usrodex".
All those who have recovered from the disease must be under medical supervision for at least 6 months.
How hepatitis spreads
Viral hepatitis spreads through contacts. The routes of transmission and prevention should be known to everyone. The virus passes from a sick person to a healthy person.
The most common routes of infection:
- Conversation at close range.
- Through hands, hugs.
- Kisses.
- By airborne droplets. Sneezing, coughing.
- Sharing household items.
- Shared toilet.
- Insufficiently washed fruits and vegetables. Especially those that were fertilized with organic fertilizers.
- Poorly processed meat, fish with blood residue. Also clams and mussels.
- Contact with the blood of an infected person.
- Public transport, counters and handrails.
- An open reservoir with contaminated water.
- Contaminated tap water.
- Non-sterile syringes.
- Sexual contact with an infected person.
The virus survives in high ambient temperatures and in unsanitary conditions. The virus can survive in salt and fresh water for up to several months.
Viral hepatitis C
I think even people far from medicine have heard about viral hepatitis C (HCV), which is called the “gentle killer.” If, however, someone is not in the know, then I will explain that this form received such a romantic nickname due to its ability to be asymptomatic for a long time, and then rapidly develop and lead to cirrhosis of the liver or hepatocellular carcinoma.
The main source, as with other parenteral hepatitis, can be a person with a chronic form of HCV or a carrier (of which, by the way, more than 2 million are officially registered in the Russian Federation alone). The routes of transmission are the same as for HBV, but the risk of becoming infected through sexual contact is slightly lower.
Symptoms
During primary infection, acute HCV is formed, in more than 85% of cases in an anicteric form, without disturbing the person in any way. The incubation period is 2-26 (6-8 more often) weeks, but it is extremely rare to establish it.
The pre-icteric period may also be completely absent. Sometimes patients describe this as an episode of poor digestion (discomfort, frequent vomiting, feeling sick) or unexplained fatigue.
If jaundice is present, other clinical manifestations may be absent. Fatigue and mild abdominal discomfort persist. Less commonly – dizziness or itchy skin. In most patients, the liver becomes enlarged, sometimes along with the spleen. But overall the condition is satisfactory.
It is the predominantly mild course of hepatitis C that, paradoxically, leads to chronicity of the process and severe complications. People do not suspect the presence of infection for many years until irreversible changes occur in the liver.
Diagnosis and treatment
Diagnosis of HCV is based on the detection of IgG to viral proteins (anti-HCV) - most often this is sufficient for a preliminary diagnosis. Additionally, HCV RNA is determined qualitatively. Also, general and biochemical blood/urine parameters are assessed in a standard way, and ultrasound/CT is performed.
Taking into account the type of viral hepatitis (B or C), the severity of fibrotic changes is assessed, but this requires a biopsy followed by histological examination, which not all patients agree to.
Treatment of HCV is based on the following principles:
- Etiotropic therapy: latest generation antiviral drugs (Sofosbuvir, Daclatasvir, Velpatasvir, interferons, Ribavirin).
- Mode: bed (if acute), “gentle” diet;
- Symptomatic support (at the discretion of the doctor).
I want to tell you about such a case in my practice. The patient, 29 years old, was operated on in August 2020 for duodenal ulcer, after which there was a need for a blood transfusion (1200 ml). She came in at the end of September with complaints of yellowing of the skin and conjunctiva.
Objectively: the patient is adynamic, has low nutrition (thin, in simple terms), severe jaundice. Liver size + 2.0 cm, painless. Laboratory tests: high bilirubin concentration (320 µmol/l), increased ALT activity (6.1 µmol/hour/l), HBV markers – IgM to HBcorAg, HBsAg, HBeAg, HBV DNA.
Conclusion – acute viral hepatitis B, icteric form, severe. Infusion therapy, sorbents, and a gentle regimen were prescribed. The patient was discharged with complete regression of symptoms after being registered at the dispensary.
How is hepatitis class A transmitted?
The main factor in the transmission of the hepatitis A virus is unsanitary conditions, lack of clean water, and close contact with a person suffering from this disease, since the route of infection is fecal-oral. In this regard, doctors call hepatitis A a disease of unwashed hands and it is most often possible to become infected from a person who does not observe basic rules of personal hygiene.
The best prevention of hepatitis A is vaccination, after which immunity remains for a sufficiently long time, protecting against the disease for an average of six to ten years. Most often, children, educators and teachers in kindergartens/schools, workers in infectious diseases departments in city hospitals, as well as workers at water supply stations, and service personnel in public catering units are affected by the disease.
Unlike all other similar viruses, hepatitis A never becomes chronic, which is why it rarely poses a serious threat to the life of people who want to be treated (however, in advanced stages it can cause serious injuries) and in moderate forms the body copes with illness on its own. But during the healing process, it is necessary to maintain bed rest, diet, a healthy lifestyle and take medications that protect and restore liver tissue in order to avoid possible complications.
In particularly severe cases, doctors choose treatment methods aimed primarily at removing toxins from the body and providing the necessary biological material to restore the cells of the damaged organ. Vitamins and blood thinners are used, but the antiviral treatment needed to fight hepatitis B is not given.
Expert advice
On my own behalf, I would like to add a few banal tips, the neglect of which usually becomes the cause of infection.
Try to avoid promiscuous sex with strangers (at least use condoms). Follow the rules of personal hygiene, using only individual manicure devices, razors, and toothbrushes. When visiting a dentist, make sure that the instruments go through all stages of sterilization, and that the doctor is highly qualified. Share your opinion about the article or stories in the comments. It will be interesting for me to read and I will try to answer everyone.
At-risk groups
Anyone can become infected with hepatitis A. However, in children under 10 years of age, the symptoms are less pronounced; in the elderly and infants under 1 year of age, complications occur.
However, risk groups can be identified in adults. The main source of infection is human biofluid. Therefore, those who have unprotected sex and often change sexual partners, especially homosexuals, are at risk of becoming infected.
Possible factors for transmission of the virus are saliva of an infected person, semen, vaginal discharge. If they get on the skin or mucous membranes where there are microtraumas, the infection will enter the body. The concentration of the pathogen in saliva is minimal, but even a kiss or the use of someone else’s toothbrush can become factors in the transmission of the virus - it will penetrate through microcracks in the gums and ulcers on the mucous membrane. For the same reason, you should not share your razor; careful sterilization of manicure instruments and tattoo needles is important. Only 0.0005 ml of blood, invisible to the eye, can remain on the scissors, containing a large number of viruses.
This is interesting: Vaccination against hepatitis A for adults: vaccination scheme, vaccine effectiveness, up to what age it is given, contraindications and side effects
Another risk group includes:
- drug addicts;
- healthcare workers in contact with hepatitis patients;
- those who travel or live in regions where the incidence is high;
- children whose parents have hepatitis;
- persons who have undergone liver transplantation.
There is no need to stop communicating with sick relatives or friends. The hepatitis A virus is not transmitted by shaking hands, communicating, or touching a doorknob.