How to recognize tuberculosis in a child
Tuberculosis is a disease that is very difficult to treat.
To avoid complications, it is important to promptly detect the presence of tubercle bacilli in the body. Parents should closely monitor the child's health. Tuberculosis of various organs occurs. But most often the lungs are affected by Koch's bacillus. In the early stages, the symptoms of the disease are often very mild. In addition, the course of the disease is similar to tuberculosis as a common viral infection. This greatly complicates the situation.
Parents do not attach much importance to cough and fever and try to cure the child on their own. This leads to serious consequences.
There are a number of signs that raise suspicion of pulmonary tuberculosis:
- Fluctuations in body temperature;
- Chills;
- Hyperhidrosis, which usually manifests itself during sleep. The back and palms most often sweat;
- Loss of appetite;
- Nervousness and insomnia;
- Hyperactivity followed by apathy;
- Severe cough producing large amounts of sputum. The appearance of mucus with blood is especially dangerous;
- Fast fatiguability;
- Shortness of breath and pain in the chest area;
- Weight loss for no apparent reason;
- Paleness of the skin;
- Enlarged lymph nodes.
The manifestation of the above symptoms does not necessarily indicate infection with Koch's bacillus. But these signs are a reason to contact a specialist who will conduct the necessary clinical studies and prescribe appropriate treatment.
Signs of pulmonary tuberculosis
In the initial stage of development, it is not always possible to detect tuberculosis, because its indicators are similar to a common cold, and you feel constant fatigue.
A person experiences a feeling of lethargy and powerlessness.
Appetite disappears, mood worsens, any experience can be accompanied by anxiety and irritability.
In the evening, slight trembling appears, sleep is disturbed, and profuse sweating occurs.
The temperature stays at the border of 37.5-38 degrees Celsius and does not decrease; a dry cough manifests itself, overwhelming at night and in the morning.
Primary signs can be expressed all at once or one at a time.
At the first symptoms, a person’s appearance begins to change, the face becomes emaciated and pale.
The cheeks noticeably hollow out, an unhealthy blush appears, and the natural shine disappears from the eyes. Noticeable weight loss occurs.
In the initial stage, these symptoms are not so pronounced, but in people with chronic tuberculosis they are immediately noticeable.
Temperature is one of the most obvious signs. If it does not decrease within 30 days (37-38 0C), there is no doubt - this is a reliable sign of tuberculosis.
A temperature above 39 0C is febrile and occurs at the last stage of the disease, when a large number of foci of inflammation form in the lungs.
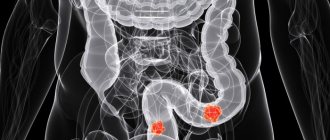
Forms and signs of extrapulmonary tuberculosis
The tuberculosis bacillus, along with the lungs, affects the liver, kidneys and other organs. In most cases, children are diagnosed with tuberculosis of the lymph nodes. The disease begins abruptly. The temperature suddenly rises. Then a cough appears.
In general, the symptoms of the disease resemble bronchitis. A reason to sound the alarm is an increase in lymph nodes. When palpated, the child does not experience pain. There is an increase in a whole group of nodes.
With kidney tuberculosis, children are bothered by lower back pain and problems with urination. Infection of the intestines with Koch's bacillus is accompanied by vomiting, diarrhea, lack of appetite, and pain in the navel.
Particularly dangerous is tuberculous meningitis, which most often occurs in children under 5 years of age. If the disease is not detected at an early stage, serious complications may develop, including death. The disease affects the state of the nervous system and brain activity of the child. If treated incorrectly, the child becomes infantile and mental retardation is diagnosed.
Forms of the disease
Tuberculosis manifests itself in different forms, the degree of development and manifestation depend on this. The incubation period can last for a year. When it is short, it means that damage to internal organs is active and the body cannot resist the infection.
Classification of tuberculosis bacillus:
- intoxication. It appears during the primary period of formation of foci of infection. Accompanied by general malaise and frequent headaches. In the evening, there is an increase in body temperature to 37.5 degrees;
- primary pulmonary tuberculosis complex. An inflammatory process forms in the tissues of the pulmonary system;
- damage to the intrathoracic lymph nodes. During treatment, hyaline appears in them, and dead cell tissue is replaced with calcifications;
- congenital form. In practice, it is quite rare, and indicates that an infection occurred during pregnancy;
- bronchoadenitis. Visceral thoracic lymphs are affected. The child has difficulty breathing. Possible suffocation, constant severe cough;
- miliary appearance. Acute form of tuberculosis, problems with capillaries arise;
- infiltrative tuberculosis infection. An inflammatory process appears on the patient’s lungs, and infiltrates form.
In addition to these varieties, there are the following forms:
- meningitis;
- tuberculosis of the lungs and kidneys;
- infection of bones and joints.
Relationship between age and disease symptoms
You can encounter Koch's wand at any age. Infection occurs especially often at the age of 2-5 years, when the child begins to actively contact the world. In newborns and infants, tuberculosis is not diagnosed so often. Depending on age, the course of the disease may be different.
The most dangerous is infantile tuberculosis. In children aged 2 to 5 years, the disease progresses very quickly and is especially difficult to tolerate. The infection often spreads to several organs at once. The nervous system is especially affected. This course of the disease is explained by reduced immunity and incompletely formed lung tissues.
Childhood tuberculosis in patients aged 5 years and older has a more favorable course. Most often only the lungs and lymph nodes are affected. The symptoms of the disease are similar to acute respiratory viral infections or bronchitis. Death at this age is unlikely. However, only timely initiation of treatment will help quickly cope with the disease.
From the age of 11, the child’s social circle expands. As a result, the risk of catching the tuberculosis bacillus increases. Additional factors contributing to infection in adolescents are hormonal changes, changes in the body, and in some cases, bad habits.
Adolescent tuberculosis is often accompanied by mild symptoms. This leads to the disease becoming chronic.
Diagnosis and analysis for tuberculosis
I would like to note that diagnosing tuberculosis is difficult because the symptoms may resemble other diseases.
Testing for tuberculosis in children is carried out using the Mantoux test with 2 units of the drug; preventive fluorography is done at the age of 15 and 17 years.
Comprehensive diagnostics is carried out in an anti-tuberculosis institution and includes the following steps:
- Compiling an anamnesis;
- Assessment of the dynamics of Mantoux samples;
- Physical examination;
- Instrumental and laboratory examination.
Chest X-ray allows you to trace changes in the lungs and intrathoracic lymph nodes. Sometimes an additional tomography of the thoracic region (linear or computer) is performed.
Using bronchoscopy, signs of endobronchitis, deformation of the trachea and bronchi are detected and swabs are obtained for research.
Various biological media are analyzed (blood, urine, sputum, etc.).
At the dispensary, children with signs of tuberculosis are additionally checked for infection using the Mantoux test, Diaskin test, Pirquet test, and Koch test.
Clinical diagnosis of the disease
Due to the fact that the signs of tuberculosis are similar to the symptoms of colds and viral diseases, it is impossible to determine the presence of Koch’s bacillus in the body at home.
Only a doctor can make an accurate diagnosis after conducting a series of studies in the clinic.
- Laboratory examination of sputum for the presence of pathogenic bacteria. It should be noted that even a negative result does not guarantee the absence of the disease.
- Fluorography. X-rays of the lungs using special equipment are permitted only for children over 15 years of age
- X-ray. The procedure is prescribed to clarify the condition of the organs in cases where the diagnosis is already known.
- Bronchoscopy is the most accurate examination that allows you to examine the inner surface of the lungs. The procedure is complex and unpleasant and is prescribed in exceptional cases.
- Tuberculin diagnostics. People call it the Mantoux test. Allowed for children from 2 years old. A special drug is injected under the skin. The state of health is judged by the body’s reaction after 2-3 days. Tuberculin diagnostics are regularly carried out in children's educational institutions. Some parents refuse the test, thereby exposing their child to the risk of late detection of the disease.
Definition of disease
School-age children are usually susceptible to the disease. There is one main way to combat tuberculosis - the Mantoux test. It makes it possible to determine the infection in the child’s body.
The difficulty in identifying the disease is that parents often do not notice the symptoms, which the initial stage of tuberculosis practically does not show. This is due to the fact that in the modern world, people's employment has increased significantly, so many things remain unattended. And although this applies to the child’s health, signs such as fatigue and lack of appetite often go unnoticed, since they are also characteristic of healthy children.
In the first days of life after birth, children are vaccinated against pulmonary tuberculosis. It allows you to avoid serious consequences of the disease, as well as identify it at the initial stage of development. Starting from the age of six, the child is given Mantoux, the reaction of which reveals the presence or absence of infection in the child’s body. This check is performed every year. If a tuberculosis bacillus is present in the body, a Mantoux reaction is observed. Its signs are redness and itching at the injection site, as well as an increase in the diameter of the spot. When such symptoms are detected, a repeat Mantoux test is done. In a similar situation, the child is sent for an examination, which is carried out by a TB doctor.
https://youtube.com/watch?v=g89X_Hj2yP8
Prevention of tuberculosis in children
The main method of preventing infection with tubercle bacilli is BCG vaccination. Vaccination is carried out in the maternity hospital in the first days of the baby’s life. This procedure has some contraindications. However, in most cases it protects the child from infection. If infected, the disease occurs in a milder form. Preventing the development of tuberculosis also contributes to a balanced diet, adherence to work and rest schedules, and hygiene.
Parents are responsible for caring for the health of the child. Early detection of signs of tuberculosis and its timely diagnosis guarantees a complete recovery and the absence of complications.
Diagnostic methods
The main method for diagnosing tuberculosis is a tuberculin test. This method allows you to identify an infectious or post-vaccination reaction. To detect tuberculin allergy using this method, the intensity of the reaction and the timing of its manifestation are taken into account. Within a year after BCG vaccination or revaccination, doctors suspect tuberculin allergy. If the reaction intensifies over time or is positive after negative reactions, the child is suspected of being infected.
A carefully collected medical history, including all possible contacts with those infected with Koch's bacillus, is very important. The most accurate method for determining infection is the Mantoux test.
Express diagnostic methods (PCR) and clinical blood tests are used.
Mantoux test
The reaction to the Mantoux test is checked 48–72 hours after administration. If an induration with a diameter of 10 mm occurs, the presence of infection in the body is confirmed. If the diameter of the induraate is 5–10 mm, the reaction is regarded as doubtful. Less than 5 mm - no infection. Children who have been vaccinated with BCG are given a Mantoux test once every 12 months, and those who are not vaccinated - once every 6 months.
Sometimes false negatives occur. In case of any doubtful result, the child is referred for a consultation with a TB specialist and additional tests, including an X-ray of the lungs.
This method has a number of contraindications. If at the time of determining the test the child has inflammation on the skin or exacerbation of chronic diseases, the Mantoux test will have to be postponed.
Mantoux test
Blood analysis
A clinical blood test is not very informative and is used in combination with other methods. There is a noticeable increase in leukocytes and band neurophils in the blood, which indicates the presence of inflammation.
PCR diagnostics
Molecular genetic testing is a method for quickly determining the DNA of the causative agent of tuberculosis. Sowing the material helps a special apparatus determine the presence of infection. A positive result in this case does not indicate a child’s illness and requires additional diagnostics. A child may be a bacteria carrier at the time of PCR diagnosis, but not get sick.
In the early stages
Detection of tuberculosis in the early stages is facilitated by regular Mantoux tests, positive reactions to which indicate infection of the child with Koch's rod (except for cases of a false positive result, which is why children are referred for additional examination). The following symptoms are also observed (more often they indicate a primary tuberculosis complex):
- lethargy, headaches, insomnia;
- poor appetite, weight loss, infants slowly gain weight;
- constant elevated temperature (during the week – 38° and above, then 37-38°);
- sometimes cough;
- difficulty breathing, shortness of breath.
Since such symptoms are characteristic of many infectious diseases of the respiratory system, a diagnosis is made only after additional research. Thus, with tuberculosis, a general blood test shows a sharp increase in ESR, and on a chest x-ray, thickening of the roots of the lungs and the accumulation of cellular mass in them become noticeable. After 3 weeks, such compactions in the lung tissues acquire clear contours.