Chronic gastritis
Chronic gastritis
is an inflammation of the gastric mucosa that occurs under the influence of bacterial, chemical, thermal and mechanical factors. The consequence of gastritis is a disruption of the digestive process (decreased appetite, heartburn, belching, nausea, a feeling of heaviness and dull pain in the stomach after eating), deterioration in general condition, fatigue, and a feeling of tiredness. The disease is diagnosed using gastroscopy, biopsy examination, and laboratory tests. Treatment includes pharmacotherapy, diet, and physical therapy.
General information
Chronic gastritis (CG) is an inflammation that is long-lasting and recurrent. The result of a long course of the inflammatory process is degeneration of the mucosa, pathological changes in its structure, and atrophy of cellular elements. The glands in the submucosa cease to function and are replaced by interstitial tissue. If at the beginning of the disease the decrease in secretion and peristaltic activity of the stomach is little expressed, then in the later stages of chronic gastritis these symptoms intensify.
In the structure of stomach diseases, chronic gastritis occupies about 80-90%. The most common variant of hCG is associated with Helicobacter pylori infection (80%), the autoimmune form accounts for 10-15%, the remaining etiological variants account for 5%.
Causes
The modern theory of the development of the most common chronic gastritis type B (antral bacterial gastritis) indicates as the cause of its occurrence the bacterium Helicobacter pylori, which inhabits the human stomach and duodenum. More than eighty percent of adults in the world are affected by Helicobacter. Infection rates in developing countries are slightly higher than in developed countries. Most often, this form of gastritis occurs in residents of Latin America and Asia. The incidence of chronic gastritis of this type does not depend on gender; the risk of development increases with age. In clinical practice, risk factors for the development of chronic gastritis are distinguished: external and internal.
External factors:
- eating disorders
(irregular meals, poor quality food, insufficient chewing, snacking on the go), bad eating habits (eating large amounts of spicy, fried, sour, smoked foods), eating very hot or very cold foods; - insufficiency of chewing function
(dental diseases, lack of teeth, decreased mobility of the temporomandibular joint); - regular consumption of alcoholic beverages
(alcohol promotes increased secretion of gastric juice, and a high concentration of ethanol directly affects the wall of the stomach, causing irritation of the mucous membrane); - a long history of smoking
, especially regular smoking on an empty stomach, contributes first to hyperacidosis, and later to a decrease in the secretion of mucosal glands and a deterioration in its protective properties (in addition, nicotine increases vascular tone, spasming small capillaries, which impairs blood circulation in tissues, including wall of the stomach); - Iatrogenic chronic gastritis is caused by prolonged use of drugs
, the most common is gastritis caused by drugs from the group of non-steroidal anti-inflammatory drugs; - occupational factor
(harmful production): gastritis most often develops when working in conditions of high dustiness and the presence of a suspension of harmful substances in the air.
Internal factors:
- chronic inflammation of the oral cavity, upper respiratory tract, lungs;
- endocrine disorders (hyper- and hypothyroidism, diabetes mellitus, disorder of corticosteroid synthesis);
- metabolic disorders (gout, insulin resistance, enzymatic deficiencies of various kinds);
- respiratory and circulatory disorders leading to tissue hypoxia (pulmonary and cardiovascular failure);
- insufficiency of the excretory system, leading to a high content of nitrogenous compounds in the blood - products of catabolism (with a decrease in the excretion of these substances by the kidneys, they begin to be released through the walls of the gastrointestinal tract, damaging the mucous membrane);
- chronic pancreatitis, hepatitis, cirrhosis of the liver and other diseases of the digestive organs contribute to pathological changes in the functioning of the gastric glands, the altered environment damages the mucous membrane and leads to chronic inflammation, and disturbances of intestinal motility can cause reflux gastritis (inflammation of the mucous membrane in the pyloric area caused by the reverse reflux of bile from the duodenum);
- autoimmune conditions: immunity disorders characterized by the production of antibodies to the body’s own tissues (the targets for autoantibodies are the parietal cells of the mucosa, which are responsible for the synthesis of hydrochloric acid, gastric mucoproteins, as well as the gastroprotective component of gastric mucus - Castle factor).
Description of the disease
This is a disease that is characterized by a long course and the development of morphological changes in the gastric mucosa:
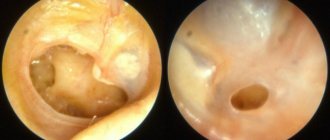
To enlarge the picture, click on it.
- increased round cell infiltration;
- violation of epithelial regeneration;
- replacement of normal glands with connective tissue;
- gradual atrophy of epithelial cells.
Chronic gastritis occurs with progressive structural changes in the mucosa and disturbances in its functionality. Inflammation of the mucous membrane affects the nature of the secretion of pepsin and hydrochloric acid.
Chronic gastritis of the stomach is observed in approximately 40–80% of the total population. This inflammation is dangerous for the development of complications such as ulcers and cancer.
This stomach disease is provoked by a variety of reasons. For a long time, the etiology of chronic gastritis was not studied. Now experts have identified the main causes of chronic gastritis, which are divided into external and internal.
External causes of pathology include:
- violation of chewing function;
- non-compliance with diet;
- eating disorder;
- eating junk food;
- smoking;
- taking medications for a long time;
- eating too hot/cold food;
- drinking alcohol.
The internal reasons are as follows:
- metabolic disorder;
- the presence of prolonged pathologies of the digestive system (liver cirrhosis, pancreatitis, hepatitis);
- the presence of long-term diseases of the oral cavity, which are characterized by inflammation;
- the presence of endocrine diseases (thyroid pathology, diabetes mellitus);
- kidney dysfunction.
Also, inflammation of the gastric mucosa can be provoked by the following groups of factors:
- Microbial (Helicobacter pylori).
- Non-microbial (all of the above factors).
- Unknown.
Stomach disease and pancreatitis in adults most often affect the body at the same time. Sometimes pancreatitis causes the inflammation in question, or, on the contrary, pancreatitis occurs against the background of this pathology.
Chronic gastritis in children and young people is most often caused by the bacteria Helicobacter pylori. They penetrate the body through kisses, hygiene items, dishes, and an insufficiently disinfected endoscope. A child can become infected in public places, in the family circle (if family members have bacteria).
The pathogenesis of chronic gastritis is as follows:
- There is a violation of the protective barrier of the mucous membrane and apical membranes of the integumentary epithelium.
- There is damage to the superficial layers of the mucous membrane. Initially, the process of inflammation covers the pyloric gastric region.
- The number of glandular cells and glands of the organ decreases. Their structural and functional changes occur.
- Cellular infiltrates from lymphocytes are formed.
- The process of inflammation affects the deeper layers of the mucosa. Dysregenerative, degenerative disorders occur, which provoke the development of atrophy of the glandular apparatus.
- The proximal gastric sections are involved in the inflammation process, and atrophy of the mucous membrane increases. There is rapid progression of antral disease.
- The process of mucus production increases, and damage to the overlying gastric sections occurs. These processes indicate chronic gastritis type B.
- If the disease progresses, erosions form on the mucous membrane. This is how the pathology turns into a new type of disease - chronic erosive gastritis. This pathology is characterized by the presence of multiple eroded areas on the mucosa. If not treated promptly, an ulcer develops.
When it comes to the morphological classification of the disease, different scientists have proposed their own classification. So WM Weinstein identified 3 forms:
- erosive;
- non-erosive;
- specific.
In the domestic medical literature, the classification of Ts. G. Masevich is recognized. He identified the following types:
- superficial (early stage, which can be detected by gastroscopy);
- without atrophy, but with damage to the glands;
- atrophic (characterized by atrophy of specialized cells inside the deepest layers of the mucosa);
- atrophic-hyperplastic (due to the atrophic process, the ridges on the mucosa change their shape, their height increases, and corkscrew-shaped convoluted pits appear between them);
- hypertrophic (it is characterized by the process of thickening of the mucous membrane, proliferation of its epithelium).
They also distinguish between active and inactive types of the disease in question. Signs of activity include diffuse lymphoplasmacytic infiltration with an admixture of eosinophils, many polynuclear leukocytes, severe edema, vascular congestion, erosion formation, and destructive processes of epithelial change.
Taking into account the secretory function of the stomach, scientists have identified the following forms:
- with increased secretory function;
- with reduced secretory function;
- with secretory insufficiency.
The activity of the disease is manifested in the infiltration of polymorphonuclear neutrophils into the mucosal epithelium. This indicator has the following degrees:
- At this degree, moderate leukocyte infiltration of the gastric mucosal plate was noted.
- This degree is characterized by the capture of the mucous plate of the organ, its fossa.
- In the third degree, there is pronounced infiltration of the lamina propria + epithelium.
Classification
Chronic gastritis is classified in terms of:
- anatomical location of the inflammation zone
(antral or fundal gastritis); - origin
(bacterial, autoimmune, endogenous, iatrogenic, reflux gastritis); - histological picture
(superficial, atrophic, hyperplastic); - state of secretory function
(hypacid - decreased secretion, hyperacid - increased secretion, with normal secretory function).
- chronic gastritis type A
– primary autoimmune gastritis of the fundus of the stomach (fundic); - gastritis type B
- antral gastritis of bacterial origin; - type C
– reflux gastritis.
There are also specific chronic gastritis, such as radiation, allergic, lymphocytic, granulomatous. According to the stage of the chronic process, gastritis can be in the phase of remission or inflammation.
Symptoms of chronic gastritis
The most common symptoms of gastritis are a feeling of heaviness, pressure in the epigastrium after eating, nausea, heartburn, and maybe a dull aching pain.
Often there is an unpleasant taste in the mouth and an appetite disorder. On examination, there was moderate pain in the anterior abdominal wall in the area of the stomach projection. In the first stages, the secretory function of the stomach can remain within normal limits, or increase or decrease. As the disease progresses, the secretion of the glands, as a rule, decreases, and the acidity of gastric juice decreases.
Hyperacid chronic gastritis is usually a superficial inflammation of the mucous membrane, without affecting the glands and their atrophy. Characteristic of young people, more common in men. With such gastritis, the pain is often severe, similar to an attack of peptic ulcer; patients often complain of heaviness in the stomach after eating, heartburn and sour belching. There is also increased production of gastric juice at night.
With gastritis of autoimmune etiology, symptoms of macrocytic anemia associated with vitamin B12 deficiency are initially noted. Subsequently, hematological symptoms (weakness, tachycardia, tinnitus, dizziness) are joined by manifestations from the gastrointestinal tract (loss of appetite, weight loss, intestinal disturbances, soreness of the tongue may be noted) and neurological disorders (weakness, darkening of the eyes , numbness in the limbs, mental lability).
Diagnostics
Diagnosis of chronic gastritis includes the following stages: history taking and external examination, physical examination, endoscopic diagnosis (gastroscopy), laboratory tests of blood and gastric juice. During the interview, attention is paid to the patient’s lifestyle, eating habits, alcohol consumption and smoking. A gastroenterologist identifies complaints and determines the nature of the dynamics of symptoms. On physical examination, pale skin may be noted (especially characteristic of autoimmune gastritis with anemia), coating on the tongue, bad breath, and upon palpation - pain in the abdominal wall in the epigastrium.
- FGDS.
The endoscopic picture gives an idea of the localization of inflammation, its severity and depth. To clarify the diagnosis and exclude malignancy, a biopsy of the mucous membrane is taken from various parts of the stomach. The acidity level of gastric juice is determined (pH-metry). - Laboratory diagnostics.
A blood test may show signs of anemia, which may be a sign of autoimmune gastritis. In this case, the blood is tested for the presence of autoantibodies. Also significant in the diagnosis of chronic gastritis is the level of gastrin, pepsinogen (the ratio of pepsinogen I and pepsinogen II) in the blood, and the content of vitamin B12 in the serum. To establish H. Pylori infection, a bacteriological examination, a breath test, and PCR diagnostics are performed.
Helicobacter pylori
Doctors often diagnose the appearance of a disease against the background of the activity of this bacterium, which, according to recent research, has already infected almost 50% of all people on earth. It was first opened back in 1982. This bacterium can also cause peptic ulcers, adenocarcinoma and lymphoma of the stomach. Once in the human body, Helicobacter pylori passes freely through the digestive system. Acid has absolutely no effect on it. After this, it can easily penetrate through the protective mucous membranes and reach the epithelial cells of the stomach. After this, the bacteria settles there.
Helicobacter pylori waste products provoke intense inflammatory processes. However, doctors have many questions about the fact that this bacterium has infected a large number of people, but the diagnosis of chronic gastritis gives a positive result only in a small number of patients.
This is explained by the fact that some people are simply genetically vulnerable to the activities of Helicobacter.
Treatment of chronic gastritis
Treatment of chronic gastritis includes actions in several areas: lifestyle correction (getting rid of bad habits, eating according to a diet), pharmacological therapy, physiotherapy, herbal medicine, as well as sanatorium treatment courses to consolidate remission.
For patients suffering from chronic gastritis with high acidity, diet No. 1 is recommended, and for hypoacid gastritis, diet No. 2 is recommended. It is recommended to eat small amounts often and avoid foods that irritate the mucous membranes in your diet.
Medicines for the treatment of gastritis.
- Drugs that reduce the secretion of hydrochloric acid
(H2-histamine receptor blockers, proton pump inhibitors). Histamine receptor blockers include drugs of the famotidine group. Proton pump inhibitors (omeprazole and drugs from its group) block the secretion of the gastric glands most effectively, which are also necessarily used in eradication measures against H. Pylori. - Antacids
bind hydrochloric acid and reduce the activity of pepsin. These drugs include: aluminum phosphate, a combination drug that contains aluminum hydroxide, magnesium hydroxide, and sorbitol. - Gastroprotective drugs
. These include bismuth preparations, which have enveloping and astringent properties, as well as a preparation of aluminum hydroxide in combination with sucrose octasulfite, which is used in the treatment of erosive gastritis and has, in addition to the main gastroprotective properties, the ability to be adsorbed, an antacid effect and an antiulcer effect. - Enzymes.
To regulate digestion in the treatment of chronic gastritis, enzyme preparations are used, and antispasmodics are used to relieve spasms and normalize peristalsis. - Antimicrobial drugs.
When infected with H. Pylori, antibacterial drugs are used for eradication: broad-spectrum antibiotics, metronidazole, nitrofurans.
Physiotherapeutic techniques are appropriate after acute symptoms subside and during remission. Methods used for chronic gastritis include electrophoresis, phonophoresis, EHF, and balneotherapy.
Treatment of autoimmune gastritis
Therapy for autoimmune gastritis has its own characteristics. Since in the treatment of this type of chronic gastritis the goal is most often to stimulate rather than reduce the secretory activity of the mucous membrane, substances that increase the acidity of gastric juice are used: succinic and citric acid, vitamin C and PP, plantain juice. The diet includes foods rich in acids (cranberries, citrus fruits, kefir, sauerkraut). These drugs and products that stimulate the synthesis of hydrochloric acid are prescribed for use on an empty stomach with reduced secretion, but not with complete achlorhydria.
To stimulate regeneration processes in the gastric mucosa, agents are prescribed to regulate tissue metabolism (inosine, rosehip and sea buckthorn oil, steroids and anabolics). Just as with other types of chronic gastritis, enzyme preparations and gastroprotectors are prescribed in therapy, and probiotics (preparations and products containing cultures of lacto- and bifidobacteria) are used to improve digestion. For autoimmune gastritis, vitamin B12 must be included in therapy to treat concomitant megablastic anemia.
Plant products
The pectins contained in these products protect the gastric mucosa from toxic substances. In addition, they remove them from the body, thereby reducing the likelihood of putrefactive processes developing. Fiber, which is also one of the components of any plant product, is involved in the removal of cholesterol.
To prevent peptic ulcers, doctors recommend drinking cabbage juice. It contains a variety of minerals and vitamins. In this case, it is better to exclude sauerkraut from the diet. People with high acidity know that consuming it leads to quite unpleasant sensations in the stomach. You should also not include pickled cucumbers in your diet. Tomatoes, even fresh, have an adverse effect on the gastric mucosa.
Stomach pain can be relieved with potato juice, which contains starch, proteins, pectins, and carotene. Carrots, which are best used in the form of puree, also occupy an important place in dietary nutrition. This dish is digestible well and contains a number of useful substances.
Pumpkin is indispensable for the prevention of gastritis, especially with high acidity. Fruits should be included in the menu in pureed form. Doctors recommend using quince as an enveloping agent. Apples with high acidity are allowed, but only sweet varieties.
Forecast
Patients with chronic gastritis should undergo preventive examinations twice a year in order to take timely measures for treatment and improve the quality of life. Patients at high risk of malignancy (autoimmune, atrophic gastritis, metaplasia and mucosal dysplasia) should undergo regular endoscopic examination.
Chronic gastritis, with proper clinical observation and treatment, does not lead to a significant deterioration in the quality of life and a reduction in its duration. A less favorable prognosis if mucosal atrophy is noted. Complications of chronic gastritis can pose a possible danger to life.
The prospects for the course of autoimmune gastritis are determined by the degree of pernicious anemia. With severe anemia, the prognosis is unfavorable and there is a risk to life. Also, with this form of gastritis, mucosal dysplasia often develops and carcinoids form.
Prevention of gastritis of the stomach with drugs and folk remedies
Everyone knows that any disease is better to prevent than to treat. This also applies to gastrointestinal diseases. Preventing gastritis of the stomach is not as difficult a task as it seems at first glance. Prevention of gastritis is divided into primary and secondary, and each type includes various measures. There are special medications for the prevention of chronic gastritis. Well-known remedies for the prevention of gastritis are Omez and De-nol, but you should know how to use them correctly. Prevention of exacerbation of gastritis also plays an important role.
Low acidity
Prevention of this disease is aimed at activating the functioning of the stomach. Gentle foods should be included in the diet. With low acidity, coffee is allowed, not strong and preferably with milk. You should eat low-fat fermented milk products, soft-boiled eggs, and steamed omelettes. Seafood is known to be extremely healthy. They should not be excluded from the diet of a person suffering from gastritis. But, of course, they should not be too spicy and salty.
For gastritis, regardless of acidity, it is necessary to eat first courses. When preventing diseases of the gastrointestinal tract, low-fat vegetable and meat broths are allowed. An indispensable component of the diet is a variety of jelly. You can drink berry and fruit juices, but only those that are not made from sour varieties.
According to generally accepted opinion, bananas are absolutely useless in terms of their nutritional qualities. But for gastritis, it is advisable to include this southern fruit in the diet, because it quite effectively coats the gastric mucosa. The same can be said about pasta, which is not popular among adherents of strict diets. When preventing chronic gastritis, such dishes can be consumed. Of course, not Carbonara pasta, flavored with an impressive amount of seasonings. Salty and spicy foods should be excluded from the diet of a person suffering from gastritis first of all.
Tablets for the prevention of gastritis
Prevention of gastritis as the most common gastrointestinal disease has two phases - primary and secondary. Primary prevention of gastritis should prevent the development of the disease in healthy people. However, if it was not possible to avoid the disease, after the attack is relieved and the acute stage is over, secondary prevention of gastritis is necessary, that is, taking measures to prevent the recurrence of an attack of inflammation and the transition of the disease to a chronic form.
Sometimes preventing relapses of gastritis involves taking medications prescribed by a doctor. Pharmacological agents are required only if there is a high risk of relapse. They can only be recommended by a gastroenterologist after examination and laboratory tests. The most commonly used drugs for the prevention of gastritis.
Sometimes preventing relapses of gastritis involves taking medications prescribed by a doctor.
Proton pump inhibitors - tablets for the prevention of gastritis
These medications reduce the production of gastric juice. In most cases, Omeprazole is prescribed for the prevention of gastritis with a tendency to high acidity. It is also applicable in the case of bacterial origin of the disease as part of the complex eradication of Helicobacter Pylori.
You can use direct analogs of the medicine, for example, Omez for the prevention of gastritis. There are also generics - substances that are identical in their effect, but with differences in composition. Such remedies include Emanera; this medication is also suitable for the prevention of gastritis.
Bismuth preparations - tablets for the prevention of gastritis
This group of drugs forms a thin film on the mucous membranes and erosions, which protects the surfaces from damaging factors and the effects of gastric juice. De-nol is considered the best option for the prevention of gastritis.
Enzymes and antibiotics - tablets for the prevention of gastritis
Enzymes are necessary for normal functioning of the pancreas and proper digestion. Effective enzymes - Creon, Panzinorm, Mezim, Festal. The fight against Helicobacter Pylori and the prevention of gastritis is carried out using antimicrobial drugs to which this microorganism has shown sensitivity - Clarithromycin, Amoxicillin, Metronidazole, Tetracycline.
Treatment
We have already looked at a disease such as chronic gastritis, what it is, what kind of disease it is, how to diagnose it, now let’s move on to methods of treating it. Treatment of this gastric pathology directly depends on the cause of its occurrence.
If the disease is caused by Helicobacter pylori, treatment should begin with antimicrobial therapy. The specialist may prescribe one of many treatment regimens for gastric pathology, which include:
- antibiotic therapy;
- taking bismuth preparations (“Ventrisol”, “De-nol”);
- taking PPIs (drugs Emanera, Nolpaza, Omez, Pariet).
If the patient has focal atrophy of the gastric mucosa, treatment is prescribed during the period of exacerbation. Such gastric pathology should be treated according to the following scheme:
- replacement treatment of gastric secretory insufficiency;
- phytotherapy;
- replacement treatment for decreased pancreatic function;
- taking medications that improve tissue nutrition and accelerate tissue healing.
Prevention of exacerbations of gastritis
Prevention of exacerbation of gastritis should be considered primarily as prevention of acute gastritis. Prevention of acute gastritis consists of preventing food intoxication, poisoning with industrial and household poisons. Sanitary control over technological processes during culinary processing of food products eliminates food poisoning.
To prevent exacerbation of gastritis, it is necessary to carefully and promptly treat various acute and chronic inflammatory diseases. These diseases include primarily inflammatory diseases of the abdominal organs: colitis (inflammation of the large intestine), cholecystitis (inflammation of the gallbladder), appendicitis (inflammation of the appendix). In addition, timely treatment of inflammation of the middle ear (otitis media), inflammation of the maxillary sinuses (sinusitis), etc. is of no small importance.
It is necessary to wage a decisive fight against alcohol abuse, especially homemade alcoholic drinks. Moonshine contains many harmful compounds - fusel oils; they have an extremely adverse effect on the gastric mucosa, causing its acute inflammation.
Stopping smoking is also a necessary element in the prevention of gastritis. Under the influence of smoking, the gastric mucosa initially thickens significantly and then atrophies. You should not eat stale food or undercooked food; You should not overuse hot seasonings. Gastritis is an inflammation of the gastric mucosa, accompanied by disturbances in its secretory and motor functions.
For the prevention and treatment of exacerbation of gastritis, it is recommended:
The main principle of preventing the occurrence of gastritis is the organization of proper nutrition.
- Do not drink water while eating: true thirst will appear 2 - 3 hours after eating. You need to quench your thirst in small portions and only with fresh water. Fruit waters, juices, natural juicy fruits, kvass - all this is food, not drink;
- Never eat desserts, fruits, sweets, or pastries after meals: at this time they are harmful and not only will not bring any benefit, but will also lead to fermentation of everything you ate before.
Prevention of chronic gastritis
Primary prevention of chronic gastritis has not been developed. Preventing the development of chronic gastritis largely depends on the timely detection and proper treatment of the diseases that cause it.
For patients with chronic antral gastritis, it is advisable to carry out preventive courses of treatment with antisecretory drugs in the autumn-spring, and for patients with secretory insufficiency - replacement therapy. In order to prevent exacerbations of reflux gastritis, it is recommended to eat frequent small meals, avoid large meals, prevent stool retention, flatulence, exercise with abdominal tension, and not wear a tight belt.
Endoscopy
This is one of the most common methods for diagnosing chronic gastritis. In this case, the doctor conducts an examination of the upper region of the digestive tract. For this, a special device is used - an endoscope. It is a long flexible tube with a tiny camera at the end. The doctor and nurse carefully insert the endoscope into the patient's throat, reaching the esophagus, stomach and, if necessary, the small intestine.
Thanks to this, a specialist can rule out a large number of diseases with similar symptoms. Thus, differential diagnosis of chronic gastritis in children and adults is also performed. This helps to exclude peptic ulcers, hernias and much more. The doctor carefully examines the condition of the stomach from the inside. Not a single picture will allow you to get such a clear picture as such a differential. diagnosis of chronic gastritis.
During the examination, the doctor may even take tissue samples. For example, if he notices that some area looks too suspicious, he can pinch off a small piece of material. The tissue obtained in this way is sent for laboratory diagnosis of chronic gastritis. This procedure also has its own name - biopsy. Thus, in the course of one study, you can obtain comprehensive information and perform two manipulations at once. However, you need to understand that such a differential diagnosis of chronic gastritis is an unpleasant procedure. It is especially difficult for children to bear it. But despite this, you need to overcome yourself, since after such a study you can get the most accurate diagnosis.
Prevention of exacerbations of gastritis in children
One of the most common digestive pathologies at school age is gastritis. It is typically characterized by a combination of a number of unpleasant symptoms that significantly disrupt the normal life of children - appetite disturbances, abdominal pain, nausea and problems with stool.
To normalize digestion, eliminate all unpleasant symptoms and ensure proper digestion and assimilation of food components, comprehensive treatment is necessary, the basis of which is diet and individually selected medications. In addition, during the remission stage, complete prevention of inflammatory processes is necessary.
As the process fades, relapses are prevented and the restoration of the gastric epithelium is stimulated. Courses of mineral waters (warm, without gas) and physiotherapeutic treatment, as well as dietary correction and physical therapy are shown. Sanatorium-resort treatment is also indicated for prevention; it allows you to achieve stable remission for several months or years.
Seaside resorts and southern regions are especially good for rehabilitation, with the presence of mineral springs with low-mineralization water used for drinking. Prevention of exacerbations is carried out in the autumn and spring periods under the supervision of a doctor through dietary correction and herbal medicine, taking a course of vitamins and general strengthening measures.
Gastritis of the stomach prevention
The main principle of preventing gastritis is following the rules of personal hygiene and organizing proper nutrition. It is necessary to take care of the completeness of the diet - do not starve, but also avoid overeating, refuse fast food on the go and dry food.
Give preference to fresh products, do not store them for a long time to avoid contamination by bacteria and microorganisms. Thoroughly wash all berries, fruits, vegetables, herbs, eggs, raw meat and fish under running water before cooking, and also follow the rules for storing food separately in the refrigerator.
Individual prevention of exacerbation of gastritis also involves eliminating foci of infection. Moreover, we are talking not only about the treatment of acute infectious diseases, but also about chronic processes such as sinusitis, tonsillitis, cholecystitis, pancreatitis, hepatitis, colitis, tuberculosis or caries. It is also important to take care of relieving neuropsychological tension using non-medicinal means, learning to overcome stressful situations, and avoiding depression, excessive fatigue and lack of sleep, because all this directly affects the functioning of the stomach.
Regular medical examination using instrumental examination methods and following the gastroenterologist’s prescriptions are very important. Treatment courses should be repeated in spring and autumn to prevent relapse. It is necessary to pay attention to the identification and treatment of all concomitant diseases of the gastrointestinal tract, cardiovascular and endocrine systems, acute infections, and various pathological conditions that are not directly considered diseases.
Long-term use of medications that irritate the gastric mucosa or, conversely, suppress the secretion of gastric juice, should not be allowed. Take any medications strictly as prescribed by your doctor, without self-medicating or using the advice of traditional medicine - this should become an unshakable rule for all those suffering from gastrointestinal disorders.
Regular medical examination is very important for gastritis.
Avoid occupational hazards to avoid toxic or irritating effects on the stomach. This includes work in hot shops, inhalation of silicate, cotton, coal and metal dust, and absorption of alkali vapors and fatty acids in the process of soap making, candle production, margarine production, painting work, etc.
Primary prevention of gastritis
Primary prevention is aimed at preventing the disease. This is facilitated by maintaining immunity, creating favorable living conditions, including good nutrition 4-5 times a day, physical activity, sports, a positive psycho-emotional state, sound sleep 7-8 hours a day.
It is very important to monitor your health, treat any diseases in a timely manner, carefully maintain oral hygiene and regularly visit the dentist. Considering the extreme prevalence of Helicobacter pylori, it is necessary to take care to exclude the possibility of infecting your body with this spiral-shaped bacterium, which lives on the gastric mucosa, attaching to the villi of the epithelium. In 80% of cases, it creates conditions for the development of peptic ulcer disease. A test for antibodies to Helicobacter pylori can now be taken in some private laboratories to refute or confirm its presence.
This is especially true for those who live or work in close proximity to carriers of this infection. For example, if someone in your family has already been diagnosed with peptic ulcer disease, you need to constantly adhere to preventive measures. So, you should not share the same cutlery, dishes, or towels with the patient. You should also refrain from kissing to reduce the likelihood of transmitting the infection to healthy family members, especially children.
Secondary prevention of gastritis
Secondary prevention of gastritis involves a course of Helicobacter pylori eradication, which is mandatory for all Helicobacter pylori-positive patients with chronic gastritis.
Prevention of exacerbations of reflux gastritis involves multiple meals in small portions (5-6 times a day), exclusion of overeating and causes that may be accompanied by an increase in pressure in the abdominal cavity (constipation, flatulence, tight belts, significant physical activity accompanied by muscle tension in the anterior abdominal wall ).
Secondary prevention of gastritis involves a course of Helicobacter pylori eradication
Patients are recommended sanatorium-resort treatment with the use of mineral waters, nutritional therapy, balneo- and climate therapy, and physiotherapeutic methods of treatment. Patients with gastritis need clinical observation with preventive examinations 2 times a year, selection of treatment and determination of further tactics for the use of therapeutic measures.
Prevention of gastritis with folk remedies
To prevent gastritis, it is important for people with gastrointestinal diseases to follow a diet. Fried, salted, smoked dishes and canned food are excluded from the diet. For breakfast, it is advisable to eat well-cooked oatmeal, semolina or rice porridge. To start the digestion process and protect the stomach mucosa from external factors, it is useful to drink a glass of warm water with the addition of honey on an empty stomach.
An effective way to prevent gastritis and many other diseases is rosehip decoction. The berry is a leader in vitamin C, iron, and magnesium content. These elements are important for the smooth functioning of digestion and protection against microbes. For 1 liter of water take 3-4 tablespoons of fruits. To preserve its beneficial properties, rose hips are dipped in water brought to a boil. After boiling, reduce the heat to minimum. Rose hips are placed when there are no bubbles on the surface. Preparation time for the decoction is 30 minutes. After this, the drink is covered with a lid and left to steep for an hour. The healing decoction is drunk between meals.
source
Prevention of all types of gastritis
A proper diet will help keep the microflora in order.
So, paying attention to the prevention of chronic gastritis, it is important to note that a number of preventive measures for this disease completely coincide with similar measures, but with respect to the acute form of the disease. In general, all types of gastritis can be prevented in two ways:
- The first is public prevention. The essence of this procedure is that government agencies monitor how all food products are produced on the territory of the Russian Federation and whether their quality meets what is necessary for the normal functioning of the gastrointestinal tract of the residents of our country.
- The second is individual prevention. In the same event, each patient with gastritis must personally carry out some preventive measures that should minimize all risks of exacerbation of gastritis.
Read: Diet and proper nutrition for high acidity
If the first type of prevention does not require the participation of the person suffering from the disease at all, but for the second, the responsibility lies entirely with him. In order to comply with basic preventive measures of an individual nature, it is necessary:
- Stick to some diet. No strict restrictions are required, but you will have to give up fast food, large amounts of fried, half-raw and fish foods. In addition, it is important to minimize the intake of spices as much as possible, because in any form this food product greatly irritates the gastrointestinal mucosa, and this can already aggravate any form of gastritis. The ideal nutritional option in the presence of chronic or acute gastritis is to alternate liquid and dry foods in the diet.
- Monitor the quality of products. Prevention in this regard is to try not to eat food of questionable production or origin. That is, it is better not to risk consuming possibly expired food or food made from low quality raw materials.
- Organize the most correct diet. There are no particular difficulties in this - it is enough to eat small meals, 4-7 times a day. This approach to nutrition stabilizes the level and secretion of gastric fluid, which minimizes the risk of re-inflammation of the gastrointestinal mucosa.
- Carefully monitor the amount of food you eat. It is, of course, possible to undereat, but overeating is, in principle, unacceptable. Try to eat proportionate portions and do not go hungry for long periods of time.
- Eat food following a certain technique. This means that you need to eat in a calm environment, chewing your food thoroughly and slowly. Otherwise, the risk of re-exacerbation of gastritis increases by 10-15%.
- Limit your consumption of alcoholic beverages. Everything is simple here - don’t abuse alcohol, and especially don’t drink low-quality surrogate. Such phenomena not only irritate the gastrointestinal mucosa, but can also cause chemical burns, which is very dangerous not only for gastritis.
- Quit smoking or “smoking” as correctly as possible. It's no secret that tobacco smoke is the worst enemy of any mucous membrane. Fortunately, it practically does not reach the stomach, but still there is some contact. In order to minimize it in the presence of gastritis of any form, it is advisable to completely quit smoking. Otherwise, you should stop “smoking” on an empty stomach, while eating or immediately after it, and also give up flavored cigarettes and reduce the amount you smoke.
- Avoid contact with chemical compounds in the form of smoke or vapors. The essence of the effect of such things on the gastrointestinal mucosa is completely similar to tobacco smoke. Considering this nuance, any person suffering from gastritis is simply obliged not to come into contact with chemicals and poisons in the form of vapors, as this is guaranteed to aggravate the inflammation of the mucous membrane of his stomach.
Read: History of gastritis: why do doctors create it and what does it include?
Note: if the disease in your particular case is accompanied by purulent formations or phlegmon in the stomach, it is important to supplement the prevention of gastritis with timely and adequate neutralization of their exacerbations.
By ignoring such a preventive measure, you can personally provoke a relapse of an unpleasant pathology.