Main symptoms:
- Abdominal pain
- Watery stool
- Headache
- Dizziness
- Bile in stool
- Exhaustion
- Foul-smelling stool
- Intestinal bleeding
- Fever
- Chills
- Fever
- Increased sweating
- Diarrhea
- Vomit
- Weakness
- Mucus in stool
- Nausea
- Liver enlargement
- Enlarged spleen
Campylobacteriosis is an infectious gastroenterological disease. The causative agent of the infectious process is Campylobacter bacteria. However, it should be noted that in some cases the causative agent of campylobacteriosis takes a generalized form, which leads to damage to other organs and is accompanied by septicemia.
Online consultation on the disease “Campylobacteriosis”.
Ask a question to the experts for free: Infectious disease specialist.
- Etiology
- Pathogenesis
- Classification
- Symptoms
- Diagnostics
- Treatment
- Prevention
Diagnostic measures are based on a physical examination of the patient, laboratory tests and endoscopic examination of the stomach. Treatment is complex - drug therapy with a mandatory diet.
This disease has no clear restrictions regarding gender and age. Consequently, campylobacteriosis is diagnosed in both children and adults. However, it is noted that school-age children are at risk. The peak incidence occurs in the hot season - from June to September.
With a localized form of the disease, the prognosis is favorable; complications are observed only in people with concomitant chronic diseases.
Disease
Campylobacteriosis is a disease caused by infection with the bacterium Campylobacter.
- Symptoms of the disease usually develop 2-5 days after infection with the bacterium, but can take 1-10 days to develop.
- The most common clinical symptoms of Campylobacter infections are diarrhea (often with blood in the stool), abdominal pain, fever, headache, nausea and/or vomiting. Symptoms usually last 3 to 6 days.
- Campylobacteriosis is rarely fatal and tends to occur only among very young children, the elderly, or people already suffering from another serious illness such as AIDS.
- Complications such as bacteremia (the presence of bacteria in the blood), hepatitis, pancreatitis (infections of the liver and pancreas, respectively), and spontaneous abortion have been reported with varying degrees of frequency. Post-infectious complications may include reactive arthritis (painful joint inflammation that can last several months) and neurological disorders such as Guillain-Barré syndrome, a polio-like form of paralysis that in rare cases can lead to respiratory and severe neurological dysfunction.
Treatment of the disease
Treatment of campylobacteriosis is only comprehensive - taking medications is combined with a special diet and daily regimen.
The medicinal part of treatment involves taking the following medications:
- antibiotics;
- sorbents;
- antidiarrheal;
- antispasmodics;
- enzymes;
- substances for correcting intestinal dysbiosis.
Enzyme preparations
In addition, the patient must adhere to a diet that includes the following recommendations:
- exception - fatty, spicy, fried, too salty, marinades, smoked meats, canned food;
- alcohol and surrogates are prohibited;
- food should be light and low-calorie;
- drink plenty of water - still mineral water, weak herbal tea, green tea, rosehip decoction;
- eating should be frequent (4-5 times a day), but with a time interval of 2.5-3 hours;
- dishes should have a liquid or puree consistency;
- The optimal cooking mode is steaming or boiling.
The gastroenterologist provides a specific list of permitted and prohibited products individually, depending on the current clinical picture, the etiology of the disease and the characteristics of the patient’s body.
If a localized form is diagnosed in a mild or moderate stage, then no complications are observed, the patient’s recovery occurs in 10-12 days, but this depends on the individual characteristics of the body.
Sources and transmission of infection
Campylobacter species are widespread among most warm-blooded animals. They are often found in food animals such as poultry, cattle, pigs, sheep and ostriches, and in pets including cats and dogs. In addition, these bacteria have been found in shellfish.
It is believed that the infection is transmitted mainly through food - through meat and meat products that have undergone insufficient heat treatment, as well as through raw or contaminated milk. Contaminated water or ice is also a source of infection. A certain proportion of cases of the disease are caused by contact with contaminated water during recreational activities.
Campylobacteriosis is a zoonosis - a disease transmitted to humans from animals or animal products. Most often, carcasses or meat become contaminated with Campylobacter from feces during slaughter. However, Campylobacter rarely causes disease in animals.
The relative importance of each of the above sources to the overall burden of disease is unknown, but consumption of contaminated, undercooked poultry meat is thought to be a major contributor. Because outbreaks associated with a common source of infection account for a fairly small percentage of cases, the vast majority of cases are reported as sporadic, with no clear pattern.
Therefore, assessing the significance of all known sources of infection is extremely difficult. In addition, the widespread prevalence of Campylobacter makes it difficult to develop infection control strategies throughout the food chain. However, countries that have implemented targeted strategies to reduce the prevalence of Campylobacter in live poultry have seen similar reductions in human cases.
The causative agent of campylobacteriosis
Campylobacter
The pathogen belongs to the genus Compylobacter and is represented by 3 species - C.jejuni, C.coli, C.lari, etc., causing acute intestinal disease (acute intestinal disease) with a similar clinical course. These are gram-negative, spirally curved rods that have specific structural features that are responsible for the symptoms:
• does not form spores or capsules, but has a capsule-like shell, which determines resistance in the external environment and to the action of phagocytosis. • There are flagella, their number reaches 5, this ensures their high mobility with corkscrew/helical/forward movements and, as a consequence of this, rapid generalization of infection. • Energy is obtained from amino acids, and this can play a role in the formation of intoxication, since such a competitive method of energy consumption leads to disruption of protein metabolism. • Long-term growth on nutrient media makes diagnosis difficult, because the pathogen forms colonies within 2-4 days. • Ability to form hydrogen sulfide – this contributes to the formation of flatulence. • Cytotoxin damages the intestinal mucosa. • Enterotoxin causes diarrhea syndrome (diarrhea). • Lipopolysaccharide of the cell wall is an endotoxin that becomes harmful only after the death of bacteria, and this component contributes to intoxication.
Campylobacter resistance:
In the environment, at room temperature, it persists for 1-5 weeks, the same periods of stability when the pathogen is found in food products, tap and waste water, milk, and also in biological waste. At sub-zero temperatures it persists for several months.
High temperatures (50°C), direct UV and air, drying, high and low pH values, and disinfectants in working concentrations have a detrimental effect. Sensitive to macrolide antibiotics, metronidazole, nalidixic acid.
High susceptibility to campylobacteriosis in persons with weakened resistance, immunodeficiency, severe concomitant pathology, after gastrectomy and treatment with immunosuppressants. People working in the agricultural industry are also at high risk. The prevalence is geographically very high and occurs on all continents, which is associated with the intensification of livestock production, increased international trade in animal feed and increasing urbanization. The seasonality of the disease is recorded throughout the year, but the maximum increase in incidence is in June-August, and the minimum is in the winter months.
Prevention methods
There are a number of strategies that can be used to prevent illness caused by Campylobacter bacteria:
- Prevention is based on control measures at all levels of the food chain, from agricultural production to food processing, production and preparation, both commercially and domestically.
- In countries without adequate sanitation systems, it may be necessary to disinfect faeces and fecal-contaminated products before disposal.
- Measures to reduce the prevalence of Campylobacter in poultry include strengthening biosecurity to prevent environmental transmission of Campylobacter to farmed birds. This control measure is only feasible if the birds are kept indoors.
- Good hygienic slaughter practices will reduce fecal contamination of carcasses, but will not guarantee the absence of Campylobacter bacteria in meat and meat products. To keep contamination to a minimum, training of slaughterers and raw meat producers in hygienic food handling and preparation is essential.
- Preventative measures to protect against infection in the home kitchen are similar to those taken to protect against other bacterial foodborne illnesses.
- The only effective method of killing Campylobacter in contaminated food is a bactericidal treatment such as heat (eg, cooking or pasteurization) or irradiation.
WHO activities
In collaboration with other stakeholders, WHO strongly advocates the important role of food safety as a key component of ensuring access to a safe and nutritious diet. WHO develops policies and recommendations covering the entire food chain from production to consumption, drawing on a range of expertise and experience in different areas.
WHO works to strengthen food safety systems in an increasingly globalized world. Establishing international food safety standards, improving disease surveillance, educating consumers and training food handlers in safe food handling are among the most important ways to prevent foodborne illnesses.
In collaboration with the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (OIE) and the WHO Collaborating Center at the University of Utrecht, WHO published The global view of campylobacteriosis in 2012.
- Global overview of campylobacteriosis - in English
WHO is strengthening the surveillance capacity of national and regional laboratories for foodborne pathogens such as Campylobacter and Salmonella.
- Global Foodborne Infections Network (GFN) - in English
In addition, WHO promotes comprehensive surveillance of antimicrobial resistance in food chain pathogens by collecting human, animal and food samples and analyzing data from different sectors.
- WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance (AGISAR) - in English
WHO, together with FAO, provides assistance to Member States by coordinating international efforts for early detection and response to foodborne disease outbreaks through a network of national authorities in Member States.
- International Food Safety Authorities Network (INFOSAN)
In addition, WHO carries out scientific assessments that serve as the basis for international food standards, principles and recommendations for the prevention of foodborne illnesses developed by the FAO/WHO Codex Alimentarius Commission.
- Codex Alimentarius Commission
Symptoms
Clinical manifestations of the local form of pathology:
- Campylobacteriosis begins with severe intoxication, which is manifested by fever, chills, hyperhidrosis, myalgia, weakness, and cephalgia.
- A few hours after the febrile period, diarrhea appears. Bowel movements become more frequent up to 15 times a day. Feces are usually liquid greenish with an unpleasant odor, streaks of blood, lumps of mucus and pus. Copious loose stools are often replaced by rare, mucous stools called rectal spit.
- Dyspepsia occurs in every fourth patient - vomiting, nausea, flatulence, heaviness and discomfort in the epigastrium.
- Cramping abdominal pain is a constant sign of infection. It worsens before defecation, has a paroxysmal nature and is localized near the navel.
- Signs of dehydration are: dry skin and mucous membranes, oliguria, short-term convulsions.
This is how a mild local form of pathology develops, which resolves within 7-9 days. In this case, the infection does not spread beyond the gastrointestinal tract.
Clinical manifestations of the local form resemble a banal foodborne toxic infection. When patients treat themselves and do not visit doctors, the disease progresses and becomes a generalized form. In advanced cases, diarrhea becomes profuse, feces contain many pathological impurities, and signs of dehydration with convulsions and meningism occur.
- Spondyloarthritis,
- Bloating and expansion of the colon,
- Bleeding from the lower digestive tract,
- Serous peritonitis,
- Dehydration,
- Hypovolemic shock
- Persistent kidney dysfunction
- Pneumonia,
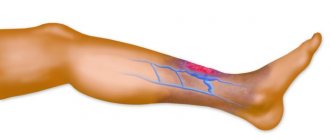
- Thrombophlebitis,
- Acute appendicitis.
A generalized form of infection occurs in exhausted and weakened individuals with mental disorders and severe somatic diseases - chronic liver pathology, endocrinopathies, tuberculosis infection, autoimmune diseases, cancer of various localizations, AIDS.
Clinical symptoms of the pathology:
- Persistent fever up to 40°C and above,
- Profuse sweat
- Shaking chills
- Sudden weight loss
- Severe dyspepsia,
- Blackout,
- Hypotension,
- Painful abdominal cramps
- Diarrheal syndrome,
- Hepatosplenomegaly,
- Anemia,
- Maculopapular rash on the skin.
Chronic campylobacteriosis has a protracted and sluggish course in people with immunosuppression. Patients complain of low-grade fever, loose stools, and painful sensations in the epigastrium. They refuse food and lose weight. General signs of pathology are often accompanied by inflammation of the conjunctiva, cornea, pharynx, and vagina.
Bacteria carriage is a subclinical form of the disease in which there are no characteristic symptoms and which can only be detected using laboratory tests.
Recommendations for the public and travelers
The following recommendations will help ensure safety while traveling:
- Ensure that food is properly cooked and is still hot when served.
- Avoid consuming raw milk and products made from raw milk. Drink only pasteurized or boiled milk.
- Avoid drinking ice unless it has been made from safe water.
- Only consume ice if it is made from safe water.
- If there is any doubt about the safety of water, boil it or, if this is not possible, disinfect it using a reliable, slow-release disinfectant (usually available from pharmacies).
- Wash your hands thoroughly and use soap frequently, especially after handling pets or farm animals, or after using the toilet.
- Wash fruits and vegetables thoroughly, especially when consuming them raw. If possible, remove the peels from vegetables and fruits.
- Safe food guide for tourists
Diagnosis of campylobacteriosis
Diagnosis is often impossible due to diverse and nonspecific symptoms, therefore, if suspected, laboratory methods are used:
• bacteriological and bacterioscopic - using these methods, the pathogen is determined in feces, blood, CSF (cerebrospinal fluid) and other biological materials. • Serological methods: RIF (immunofluorescence reaction), RSK (complement fixation reaction), ELISA (enzyme-linked immunosorbent assay), RPHA. Using these methods, the qualitative and quantitative determination of antigens and antibodies is determined.
Recommendations for food handlers and preparers
WHO has formulated the following recommendations for food handlers:
- Persons involved in food processing and preparation, both professionally and at home, should exercise vigilance when preparing food and observe good hygiene practices related to food preparation.
- Food handlers and food preparers who experience fever, diarrhea, vomiting, or noticeable infected skin lesions should report it to their employer immediately.
- The WHO brochure The Five Keys to Safe Food provides the basis for educational programs for preparing food handlers and consumers. These principles are especially important for preventing food poisoning. The five principles are as follows:
- keep clean
- separate raw from cooked
- carry out thorough heat treatment
- store food at safe temperatures
- use clean water and clean food raw materials.
- Five Essential Principles of Safe Food