What is cirrhosis
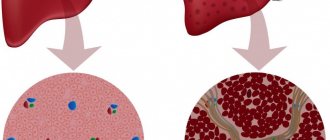
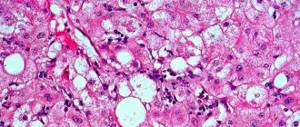
Liver cirrhosis is a total damage to the organ, in which functional liver cells - hepatocytes - die, and fibrous tissue forms in their place. Fibrous deposits result from activation of stellate cells. The function of stellate cells is to protect the organ from the inflammatory process. By protecting hepatocytes with fibrous fibers, it is possible to limit the pathological process and prevent the spread of suppuration to the entire organ. However, with cirrhosis of the liver, stellate cells grow everywhere, chaotically, thereby disrupting the structure of the organ. Replacing dead hepatocytes, fibrous fibers form entire nodes that do not perform liver functions. In fact, such a replacement leads to complete paralysis of all liver functions - it cannot secrete bile, does not neutralize toxins in the body, does not regulate hormonal levels, and does not participate in the digestion process.
Cirrhosis of any etiology significantly affects human health. The patient’s quality of life deteriorates, he suffers from complications of the disease, and with the development of the last stage of cirrhosis, the patient’s death occurs.
The most important functions of the liver
First of all, I would like to say what the liver is. This is an organ consisting of specific lobules, which include hepatocytes (liver cells), between which the bile ducts are located, and in the center is the central vein. The slices resemble a “honeycomb” in appearance. In liver cirrhosis, it is instead of such lobules that fibrous tissue is formed.
The liver is a kind of factory for processing harmful products and synthesizing substances necessary for the life of the body.
The most important functions of the liver are:
- detoxification. Neutralizes harmful substances (indole, skatole) formed inside the body or coming from outside;
- synthetic. Participates in the creation of proteins (globulins, albumins), carbohydrates, fats necessary for the full functioning of all living things;
- formation of coagulation factors. Necessary to stop various bleedings;
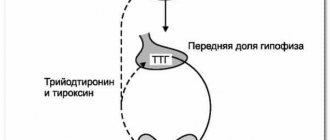
- is a storage (depot) for vitamins (D, E, K, A, etc.), glycogen (needed for the synthesis of glucose, which is a nutrient for the brain and other organs), some hormones;
- in the fetus it is a blood-forming organ.
Statistics
The disease is quite common throughout the world. Symptoms of liver cirrhosis are diagnosed more often in men, but more so in the female half of the population. More than three hundred thousand patients die from cirrhosis every year, but mortality statistics in this regard are not stable. Over the past decade, mortality has increased by 12 percent. There is also a high rate of people suffering from alcoholism who have pathology in the latent stage, when external signs of cirrhosis have not yet appeared.
The first causes and symptoms of liver cirrhosis in women and men are more often diagnosed over the age of forty years.
Causes of the disease
The most commonly diagnosed causes of cirrhosis are the following disorders:
- damage to the organ by hepatovirus, as a result of which hepatocytes - liver cells - suffer;
- alcohol abuse for ten years or longer, and what is important is not so much the dose of alcohol and its strength, but the regularity of its intake and the presence of ethyl alcohol in the drink;
- the patient has autoimmune diseases;
- pathologies of the biliary tract, both congenital and acquired;
- increased pressure in the portal vein;
- stagnation of blood circulation in the liver;
- hereditary metabolic disorders;
- poisoning with toxic substances;
- work in hazardous conditions;
- long-term use of certain medications;
- Rendu-Osler disease (pathological thinning of the capillaries).
Despite such an impressive list of causes of liver cirrhosis, about forty percent of cases remain etiologically unclear - it is not possible to find out the cause of the pathology. Such cirrhosis is called cryptogenic, and it is assumed that the disease could be caused by a violation of the rules of rational nutrition or previous infectious diseases.
Etiological prerequisites for development
For cirrhosis to occur, a combination of two or more causes is necessary. Statistics show that most often it is a previous viral hepatitis + alcoholism. But other combinations are also possible.
- Alcoholism - changes in the liver are observed in 35% of people suffering from alcoholism. The influence of this factor in etiology is proven by the improvement in organ function after stopping alcohol consumption.
- Viral hepatitis B and C cause the disease in ¼ of cases. Untreated hepatitis is dangerous not only for the patient himself, but also for those around him due to the ability to cause viral carriage.
- Diseases of the biliary tract - up to 1/10 of the occurrence in all cases are explained by long-term chronic diseases of the gallbladder, duct dyskinesia, cholelithiasis. First, the bile ducts are blocked, then the liver cells are destroyed.
- Toxic hepatitis - most often associated with prolonged contact with industrial toxic substances (dyes, insecticides, concentrated acids, salts of heavy metals) or with the damaging effect of drugs on liver cells.
- Irreversible changes occur in the decompensation stage of chronic heart failure. They are caused by stagnation of venous blood in the inferior vena cava and further in the hepatic veins, ischemia of the liver tissue.
- Chronic infectious diseases (brucellosis, echinococcosis, toxoplasmosis) contribute to hepatitis and then cirrhosis.
- The cryptogenic variant is a dangerous form of the disease due to its speed of development and unknown causes. Patients are immediately candidates for liver transplantation upon diagnosis.
- Congenital malformations (absent or short bile duct) lead to cirrhosis in adolescence.
According to morphology
In 1974, at a medical congress in Acapulco, a morphological classification of liver cirrhosis was first proposed, which was recognized four years later by the World Health Organization. According to this classification, liver cirrhosis can be:
- small nodular - with the formation of fibrous nodes from one to three millimeters;
- large-nodular - when larger nodes appear that exceed three millimeters in size;
- incomplete septal form of cirrhosis – incomplete septa develop in the liver;
- mixed form of the disease - characterized by the presence of septa and nodes of various sizes.
By etiology
The classification is based on the etiology of the disease. According to this division, the following cirrhosis is distinguished:
- viral;
- drug;
- alcoholic;
- secondary biliary;
- congenital cirrhosis with hemochromatosis, alpha-one antitrypsin deficiency, tyrosinosis, galactosemia, glycogenosis;
- congestive cirrhosis caused by poor circulation in the organ;
- metabolic and nutritional cirrhosis;
- liver cirrhosis with an unknown cause of the disease, for example, primary biliary cirrhosis.
Stages
Depending on how cirrhosis of the liver manifests itself in men and women, there are several stages of cirrhosis.
In the first stage of liver cirrhosis, most patients do not experience any specific signs indicating the presence of the disease. The disease can be detected only through a thorough examination of the patient - a blood test, enzyme immunoassay, and ultrasound examination. Already at the first stage of the development of the disease, a blood test will show an increase in bilirubin in the blood, as well as a drop in the prothrombin index. The most reliable data can be obtained using a biopsy and liver tests, but in other cases the symptoms of cirrhosis may be erased, and research data may be controversial. Since at the initial stage of the development of the disease, even with the death of hepatocytes, the liver can fulfill its role in the body, this stage is called compensatory. At this stage of the development of the disease, patients do not feel a deterioration in their health, only occasionally they may complain of fatigue, decreased performance, and depression. Unmanifested cirrhosis is dangerous due to its hidden course.
However, despite the ability of the organ to compensate for violations, clinical syndromes in liver cirrhosis, provoked by pathology, are already beginning in the body. If left untreated, the disease will progress until the liver completely stops functioning.
Since at this stage of the disease patients do not go to the clinic, the patient detects liver cirrhosis during a random examination.
The second stage of liver cirrhosis is called subcompensated. This means that with the progression of the disease and the death of a significant part of the hepatocytes, the liver can no longer fully perform its functions and the first symptoms of liver cirrhosis occur. Already at this stage of the disease, patients begin to feel that some disturbances have occurred in their body. Patients suffer from apathy, lack of appetite, weight loss, nausea, and a feeling of heaviness in the right hypochondrium. At this stage of the disease, adult men show signs of gynecomastia - the mammary glands increase in volume, as the liver stops blocking the level of female hormones.
In a blood test, this stage of cirrhosis is manifested by a drop in albumin levels and a further decrease in the prothrombin index. If liver cirrhosis is treated successfully at the second stage, this gives encouraging prognoses for the outcome of the disease and its transfer to the compensated stage. With timely and proper treatment of the disease, following a diet and abstaining from alcohol, a person’s liver can work, although not at full capacity, but at least without complications for the body.
The third stage of cirrhosis is characterized by a critically low level of “live” hepatocytes that can function normally. At the same time, the so-called liver failure. At the same time, the symptoms of liver cirrhosis in women and men begin to appear more pronounced. The skin acquires a yellow tint of varying intensity, and the sclera also turns yellow. Pain in the right hypochondrium appears more and more often in the patient. At the third stage of the pathology, ascites occurs - accumulation of fluid in the abdominal cavity. The first signs of liver cirrhosis in women with ascites may more closely resemble the third trimester of pregnancy than pathology of the digestive organ.
A blood test shows a drop in the prothrombin index and a significant decrease in albumin levels. It is almost impossible to cure cirrhosis with medications at the third stage. Radical treatment - a liver transplant - will help, but in case of significant complications, doctors do not guarantee that the organ will take root and be able to fully perform its functions. Therefore, the issue of transplantation is considered in rare cases. If the disease is not treated, the final stage of cirrhosis occurs, in which the patient's health deteriorates sharply, patients fall into a coma or die from internal bleeding.
Already at the third stage of development of the disease, all the prerequisites are created for the appearance of complications - hepatic coma, malignant liver tumor (cancer), purulent peritonitis or pneumonia.
The fourth stage is called terminal. This means that the patient's life is at risk. At the moment, doctors do not know how to treat liver cirrhosis at this stage, so they can only give painkillers, organize relief of the manifestations of the disease, and care for the patient in the comatose stage. The question of whether cirrhosis of the fourth stage of the liver can be cured can be clearly answered in the negative, since it is not the cirrhosis itself that comes to the fore, but the complications that have developed against the background of cirrhosis. They cannot be cured
By Child-Pugh
Doctors Child and Pugh, during long-term observations of patients with cirrhosis, identified stages of liver cirrhosis with a survival prognosis linked to them. As practice shows, this classification has proven itself, therefore it is also used in the diagnosis of liver cirrhosis. The principle of classification is that for each complication and for each sign the patient receives certain points. Subsequently, the scores are summed up and the prognosis for the survival of such a patient can be determined.
Patients receive one point for the absence of ascites, bilirubin level less than 34 µmol/l, absence of liver failure and prothrombin index above 60 points.
Two points are given for ascites that can be eliminated, a bilirubin level of 34 to 50 μmol/L, an albumin level of at least 2.8, and mild hepatic encephalopathy that can be corrected. The prothrombin index should be between 40 and 60.
A patient will receive three points for ascites that cannot be treated, high bilirubin (over 50), a decrease in albumin below 2.8 and liver failure of the third or fourth degree. If the patient receives 5-6 points, then the one-year survival rate of such patients is one hundred percent and the two-year survival rate is 85 percent. The indicators deteriorate significantly when scoring from 7 to 9 points, but the most critical are 10-15 points, at which about forty percent will live another year after diagnosis, and only 35 percent of patients are promised two years of life.
The disadvantage of the Child-Pugh classification is that it does not take into account a lot of other parameters and does not correctly recognize cirrhosis of the liver. For example, to identify cardiovascular pathologies or portal hypertension, which can significantly distort the forecasts according to the table proposed by scientists.
Laboratory tests for suspected cirrhosis
If the attending physician suspects cirrhosis, then a whole range of diagnostic measures must be prescribed: laboratory and instrumental studies. Laboratory methods to determine the course of the pathological process include:
- clinical blood and urine test,
- blood chemistry,
- coagulogram,
- stool analysis to identify hidden impurities,
- testing of hepatitis virus markers.
None of these tests can reliably determine the presence and characteristics of pathology. For an objective and complete assessment of the patient’s condition, a comprehensive comprehensive study is necessary.
Deciphering the data obtained from laboratory studies allows us to determine the speed and characteristics of biochemical reactions occurring in the liver, the level of toxins, the time of their utilization and elimination. The presence of hepatitis viruses indicates an inflammatory process and allows us to determine the cause of the pathology. Analysis of stool can reveal a fairly common complication - internal bleeding due to varicose veins of the digestive organs.
General clinical blood test
A general clinical blood test for liver cirrhosis is mandatory and first of all. Quantitative indicators of the main elements of blood composition decrease. The erythrocyte sedimentation rate (ESR) increases with active inflammation. During the OAC, the following indicators are assessed:
- normal hemoglobin averages 140-150 g/l in the male body, and about 130 g/l in women; with cirrhosis, this figure decreases significantly, anemia is detected,
- the leukocyte level is normally 4.9*10^9/l, the pathological process leads to an increase in this indicator,
- the normal level of red blood cells is on average 4*10^12/l,
- the level of platelets in the blood is on average 200-300*10^9/l,
- the normal ESR ranges from 6 to 9 mm per hour.
The diagnosis of “cirrhosis” cannot be made solely based on the results of a general clinical blood test, but it gives a certain idea that a pathological process is occurring that causes deviations in the composition of the main body fluid.
Blood chemistry
Many biochemical processes take place in the liver: most of the protein structures necessary for the body, including enzymes, are formed in this organ. Pathological processes affect the speed and quality of the synthesis of these compounds. In general, the following changes are noted:
- the content of bilirubin increases, both its direct and indirect fractions,
- transaminase levels increase - AST and ALT,
- the content of alkaline phosphatase increases,
- gamma-glutamyl transpeptitase increases,
- the amount of gamma globulins and haptoglobins increases,
- the content of specific liver enzymes increases (nucleotidase, arginase and others),
- albumin content decreases,
- the level of prothrombin decreases, and the blood clotting time increases,
- cholesterol content decreases.
Let us consider in more detail the changes in these biochemical parameters for diagnosing cirrhosis.
Bilirubin
The bilirubin indicator characterizes the processes occurring in the liver. The substance bilirubin is essentially toxic to humans, and can be found in the body in two fractions: bound and free. One of the functions of the liver is to utilize it. An increase in bilirubin levels may indicate that organ function is reduced. However, in four out of ten people with cirrhosis, bilirubin remains normal.
Alkaline phosphatase
An increase in the level of alkaline phosphatase, a cellular enzyme in the liver ducts, indicates that these cells are being destroyed and the enzyme enters the bloodstream. Also, an increased level of this enzyme in the blood may indicate stagnation of bile inside the organ.
Gamma-glutamyl transpeptitase
This enzyme is necessary for normal amino acid metabolism. With cirrhosis, its level in the blood increases, which indicates that functional liver cells are intensively destroyed. If the indicator is considered in dynamics, then its consistently high level indicates the progression of cirrhosis. GGT levels may increase due to decreased liver function for reasons such as regular alcohol intoxication, high concentrations of toxic substances, including due to drug overdose.
ALT
Alanine aminotransferase is one of many enzymes produced by functional liver cells. Normally, it is present in the liver parenchyma, and enters the bloodstream in a small volume. With the massive death of hepatocytes, this transaminase becomes free and as a result ends up in the blood. A sluggish pathological process provokes a slight increase in ALT in the blood, approximately 2-5 times. A strong increase often indicates acute inflammation, in this case the values can range from 450-500 IU/l. When the pathology enters the stage of cirrhosis, the destruction of hepatocytes does not occur as intensely.
AST
Aspartate aminotransferase is a protein, an enzyme, the largest quantities of which are normally found in the myocardium, but is also present in the tissues of the liver, kidneys, and lungs. An increase in transaminase levels indicates that hepatocytes are being destroyed.
Normal levels of ALT and AST transaminases against the background of other abnormalities indicating cirrhosis indicate that the pathology has been occurring for a long time, and the total number of functional cells is already small.
Albumin
Albumin are blood proteins produced by the liver. In a healthy person, albumin makes up about half of the total blood protein. Liver pathologies can significantly reduce the production of these compounds. The organ can no longer synthesize a sufficient amount of albumin. Normally, they are contained in the blood in amounts from 35 to 50 g/l.
Gamma globulins
Gamma globulin belongs to proteins that perform a protective function. Produced by the liver. Normally, blood plasma contains from 10 to 22% gamma globulins. Cirrhosis provokes an increase in the content of immunoglobulins in the blood plasma.
Prothrombin index
Blood clotting occurs under the influence of certain substances, proteins produced during biochemical reactions in liver cells. With the mass death of hepatocytes, the production process of these proteins is disrupted, which leads to poor coagulation. Therefore, if the doctor suspects the presence of cirrhosis, then the so-called INR (international normalized ratio) or prothrombin index (PTI) is calculated. The test compares the rate at which a patient's blood clot forms with a reference rate. In a healthy person, the prothrombin index is from 1 to 1.5. With cirrhosis, this number increases.
Serum iron
The study of this indicator helps in identifying one of the possible provoking factors of cirrhosis. If a patient has a rare genetic pathology characterized by impaired iron metabolism, then this element begins to accumulate in cellular structures. Excess iron in functional liver cells leads to intoxication and disruptions in their functioning, which can cause the development of cirrhosis.
Types of cirrhosis
Types of liver cirrhosis are distinguished by the degree of compensation of the body. Varies:
- compensated cirrhosis - with the disease, the liver copes with its functions, although it performs it to a limited extent;
- subcompensated - the organ can no longer perform all its functions, but with this type of cirrhosis serious complications have not yet developed;
- decompensated cirrhosis - in this type of disease the liver is no longer functional, severe complications rapidly develop, and death occurs.
Prevention and prognosis
Prevention of the disease consists of limiting alcohol consumption, adequate and timely treatment of viral diseases that contribute to the development of cirrhosis. An active lifestyle and proper, balanced nutrition are also recommended.
Alcoholic cirrhosis develops rapidly with continued alcohol consumption and leads to life-threatening complications. Patients with ascites have a survival prognosis of about 3–5 years. When abdominal venous bleeding occurs in the first episode, the survival rate is 30 to 50%. In the vast majority of cases, hepatic coma leads to death - 90–100% of cases.
Cirrhosis is an incurable liver disease , but if treatment is started in the early stages and bad habits are eliminated, the prognosis is relatively favorable.
How it manifests itself
Signs of liver cirrhosis in men and women are practically the same. Patients at the initial stage of the disease feel weak, they develop apathy, and their performance decreases. As the disease progresses, characteristic symptoms appear; how to recognize cirrhosis:
- bleeding gums, spontaneous nosebleeds;
- weight loss;
- decreased concentration;
- daytime sleepiness;
- insomnia at night;
- loss of appetite;
- bloating;
- jaundice;
- atypical color of stool and urine;
- stomach ache;
- swelling of the lower extremities and hands;
- accumulation of fluid in the abdominal cavity;
- manifestation of spider veins under the skin;
- palmar erythema, or hepatic palms;
- in men - gynecomastia;
- splenomegaly;
- aching pain in the right hypochondrium;
- nausea and vomiting, stool upset;
- itching on the skin;
- male sexual impotence;
- smoothing the surface of the tongue.
Viral cirrhosis of the liver
The disease can develop as a result of viral hepatitis B, C and. Infection with these viral infections occurs through the blood, sexually (hepatitis B), and they can also be acquired in utero from the mother.
Most often, symptoms appear in the last stages. However, there are a number of symptoms that may signal the disease.
- lethargy, loss of strength (affect performance);
- the liver increases in size and becomes denser;
- the patient experiences weight loss, nausea (sometimes to the point of vomiting);
- aching nagging pain in the liver area.
If the viral form develops into liver failure, then the symptoms rapidly change, the patient’s condition sharply worsens:
- weight drops significantly;
- swelling of the limbs appears;
- vomiting, diarrhea and constant nausea;
- nervousness, sleep problems, loss of performance due to weakness;
- itching of the skin;
- yellowness is pronounced on the skin, as well as yellowness of the eyeballs;
- problems with blood pressure and heart rate;
- bleeding is observed from the mucous membranes of the mouth, in the gastrointestinal tract, and at the injection site.
Complications
With pathology, severe complications develop due to disruption of the organ. One of the most severe injuries is hepatic encephalopathy. Encephalopathy is a disease that develops under the influence of poisons and toxins on the brain that are not neutralized by the liver. It manifests itself as muscle disorders, the intellect suffers, which causes confusion. In extreme cases of encephalopathy, the patient falls into a coma.
The most common cause of death is internal bleeding from large blood vessels. They develop due to impaired blood flow and the creation of pressure in the blood vessels. Typical signs of this pathology are pale skin, cold sweat, possible vomiting with blood from the stomach, and with prolonged bleeding, patients lose consciousness.
Infections can most often occur against the background of ascites - the fluid becomes a favorable environment for the occurrence of purulent peritonitis and pneumonia. When such complications occur, patients die from sepsis within a few days.
A complication of cirrhosis is hepatocellular carcinoma, a malignant neoplasm that is fatal.
What are the causes of cirrhosis?
The main reasons for the development of cirrhosis are:
- Alcohol abuse. Men whose daily dose of 100% alcohol exceeds 100 milliliters for several years are at risk.
- People who live with hepatitis C or B develop liver cirrhosis in 25% of cases.
- Cirrhosis is also often caused by chronic autoimmune hepatitis.
- Dysfunction of the urinary system. If obstructions to the passage of bile appear in the bile ducts, this can provoke biliary cirrhosis.
- Poisoning by toxic substances (food, chemical, radiation)
- Taking pills that are hard on the liver, such as steroids.
- Long-term advanced diseases of the circulatory system.
- Buddy-Chiari disease, in which the liver capillaries become smaller.
- Operations in the intestinal region.
- Sarkaidosis
- Infection of the body with parasites.
In every fifth case of cirrhosis, the cause of the disease cannot be determined.
Diagnostics
The disease can be diagnosed using modern methods: biochemical and general blood tests, ultrasound, biopsy, enzyme immunoassay. A visual examination of the patient and collection of anamnesis are of great diagnostic importance. Magnetic resonance imaging, computed tomography, and elastometry methods are also used. The doctor knows how to determine liver cirrhosis and its stage, who will compare all the patient’s test results and will monitor the patient, monitor how liver cirrhosis develops.
Diagnosis of cirrhosis
To make a diagnosis, you can additionally do:
- general blood test (decrease in platelets, hemoglobin);
- biochemical analysis - liver tests (increased ALT, AST, alkaline phosphatase, bilirubin, thymol test); creatinine and urea to assess kidney condition;
- coagulogram. To assess the state of the blood coagulation system;
- markers of viral hepatitis;
- feces for occult blood - to diagnose bleeding from various parts of the gastrointestinal tract;
- alpha-fetoprotein - for early diagnosis of cancerous degeneration;
- ultrasound of the abdominal organs to assess the condition of the liver, spleen, free fluid in the abdomen, etc.;
- fibrogastroduodenoscopy to assess the condition of the esophageal veins;
- sigmoidoscopy to examine hemorrhoidal veins;
- scintigraphy - determines the number of functioning liver cells.
Treatment
Treatment of the disease involves several directions. First of all, it is necessary to eliminate the root cause of the disease that caused cirrhosis. When the unfavorable factor is eliminated, the liver will no longer be negatively affected and the destruction of the organ can be stopped.
After this, it is necessary to take care of the restoration of hepatocytes, which must function fully even for the cells that died during cirrhosis. For this purpose, special medications are taken.
Patients must be prescribed a diet and a healthy lifestyle.
Eliminating the causes of illness
With alcoholic cirrhosis of the liver, the patient must completely abstain from alcoholic drinks of any strength and in any quantity, since this contributes to the development of the disease. The patient undergoes detoxification therapy to remove toxins formed over years of drinking alcohol.
If cirrhosis is a consequence of viral hepatitis, then treatment of the underlying disease with modern drugs Sofosbuvir, Daclatasvir and Ledipasvir is indicated, which have a very good effect in the stage of compensated cirrhosis.
In case of drug-induced cirrhosis, it is necessary to eliminate the drug that has become poisonous to the liver and detoxify.
If autoimmune processes are the key cause of the pathology, the administration of immunosuppressants is indicated.
Liver restoration
Liver function can be restored with the help of certain drugs - hepatoprotectors. These drugs are based on herbal ingredients and do not harm liver cells. By prescribing hepatoprotectors, it is possible to restore those liver cells that have not died. It is worth saying that hepatoprotectors may not be effective in all cases, since in severe stages of the disease, treatment of cirrhosis with hepatoprotectors alone will not give results.
Drug treatment
If cirrhosis of the liver is diagnosed, treatment with medications is most effective in the first two stages of the disease. Medicines for cirrhosis are prescribed depending on the cause and complications of the disease. For viral hepatitis, the disease is treated with antiviral drugs and vitamins and microelements are prescribed. For ascites that has developed against the background of cirrhosis, diuretics are recommended. Karsil, Anaprilin, Sibektan, Creon, Silymarin, Ursosan, Nitrosorbitol will have a certain effect.
How to cure late-stage liver cirrhosis is a complex question; in most cases, doctors can only offer a transplant, and other methods are ineffective.
Folk remedies
Is it possible to cure liver cirrhosis with folk remedies? This question is asked by patients when faced with a disease, but the answer is clear - no. If signs of the disease occur, it is important not to go to the pharmacy for herbs, but to consult a doctor who will prescribe drugs with proven effectiveness. Only when the disease is managed by the attending physician can one hope for a positive outcome. However, this does not mean that folk remedies cannot be taken. The doctor may prescribe diuretics, cleansing herbs, and choleretic herbs. Dandelion, milk thistle, rose hips, corn silk, and beet juice are useful.
Diet
There is no special diet for liver cirrhosis. Doctors recommend adhering to table No. 5 - a general diet for diseases of the liver and biliary tract. The diet is designed to facilitate the functioning of the organ; all its components are balanced. It is recommended to give up alcohol, fatty and fried foods, smoked meats, offal, canned food; fast foods and other unhealthy foods are strictly prohibited. Diet: small portions five times a day. Drinking regimen – 1.5-2 liters per day as recommended by a doctor.
Forecast
Treatment of liver cirrhosis in men and women in the first two stages of the disease gives a positive prognosis, provided that all doctor’s recommendations are followed. The third and fourth stages are complicated not so much by cirrhosis as by other pathologies, so in this case doctors do not give encouraging prognoses. Even with an organ transplant, the new liver may fail if physical health is compromised.
In the fourth degree of the disease, patients die from hepatic coma, internal bleeding, infected ascites, or metastases of hepatocarcinoma.
Who to contact?
Liver cirrhosis in women and men can be treated by a general practitioner, but in most cases the doctor gives a referral to a gastroenterologist or infectious disease specialist. It is best if the medical institution has a hepatologist - a specialist who has sufficient experience in treating cirrhosis and will tell you what to do in case of liver cirrhosis. If surgical intervention is necessary, patients diagnosed with cirrhosis are treated by abdominal surgeons and transplantologists.
Know that if a person has symptoms of a developed pathology, under no circumstances should you hesitate. With timely diagnosis of the symptoms of liver cirrhosis and treatment of the disease, it can be transferred to the compensated stage.