Mycoplasma is the smallest organism that can cause the infectious disease “mycoplasmosis,” which is characterized by an acute form and is fraught with serious complications.
The smallest organism mycoplasma is capable of causing the infectious disease "mycoplasmosis"
How dangerous is mycoplasma in a woman, how to identify the infection and protect yourself from infection?
Methods of infection
Mycoplasma infection is characterized by a rather slow increase in symptoms; they can appear even several months after infection. Therefore, many infected people, being carriers of the infection, do not even suspect that they are “spreading” mycoplasmosis.
- The most common way of spreading this infection is sexually. Moreover, any type of sexual contact (genital, oral, anal) can result in infection. In this case, only a barrier method of protection will reduce the likelihood of transmitting the disease.
- The vertical route of transmission of infection occurs when the fetus passes through the birth canal during natural childbirth. This is facilitated by a high concentration of infectious agents that are found in the cells of mucous tissues.
Causes of the disease
Mycoplasmas of a genital nature are transmitted from a carrier to a healthy woman through sexual contact during unprotected sexual intercourse (oral and genital).
Mycoplasmas are transmitted sexually through unprotected sex
A small percentage of mycoplasma infection can occur through household means (through household items). Most rarely, infection occurs due to the use of unsterile medical equipment.
Note! If a pregnant woman becomes infected while pregnant, then in 60% of cases the infection will be transmitted to the child through amniotic fluid or the birth canal.
With strong immunity, mycoplasma will not cause inflammation in the body, and the person will simply remain a carrier of the infection. In order for mycoplasmosis to develop, favorable conditions are necessary for the proliferation of microorganisms. Provoking factors for the occurrence of mycoplasmosis are:
- Sexually transmitted infections associated with infection (chlamydia, gonorrhea, trichomoniasis);
- Changes in hormonal levels during pregnancy;
- Hypothermia of the body, sudden climate change;
- Severe stress, emotional stress;
- Pathologies of the endocrine system;
- Lack of proper genital hygiene;
- Ovarian diseases;
- Decreased immunity due to illness or poor lifestyle;
- Long-term use of hormonal drugs, antibiotics;
- Promiscuous sex life (constant change of partners, frequent abortions, early onset of sexual activity).
Mycoplasma infection is very difficult to determine, because... the incubation period lasts 3-5 weeks (in some cases up to two months). Therefore, mycoplasma is very difficult to diagnose in the early stages, especially considering that the disease usually does not have a clear clinical picture.
Symptoms
The presence of mycoplasmas in the body is indicated by the erased low-symptomatic signs characteristic of this disease. Approximately 10-20% of infected people do not feel obvious symptoms of the disease until a stressful situation, for example, severe hypothermia or abortion, activates the infection.
Often, the acute form of the pathology is preceded by a long incubation period, and only a week after infection the first symptoms of the disease may appear:
- When the external genitalia are affected, bacteria accumulate on the mucous membrane of the urethra and vagina. As a rule, in such a situation, patients do not complain.
- In rare cases, colorless discharge from the genitals and itching of the external genitalia may occur.
- When an infection penetrates into a woman’s internal genital organs, unpleasant symptoms occur: burning during urination, pain in the lower abdomen, and rarely, thick purulent discharge.
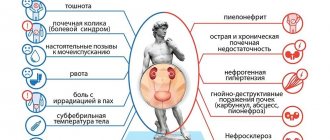
Urogenital mycoplasmosis in women can manifest itself as:
- inflammation of the ovaries, uterus and fallopian tubes;
- mycoplasma urethritis;
- pyelonephritis;
- bacterial vaginosis (gardnerellosis);
- Mycoplasmosis is often combined with ureaplasmosis and chlamydia.
Features of the disease
Treatment of mycoplasmas in women should begin as early as possible. More than 40 species of various mycoplasmas are known to modern science. Only a few pose a real danger to humans. These are Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum and Mycoplasma pneumoniae.
The listed infections can lead to various problems, so at the first symptoms of this disease you should immediately consult a doctor.
This disease is detected in more than half of patients suffering from chronic diseases of the genitourinary system. Moreover, it is also observed in 5-15% of healthy women, which indicates that the infection in some cases is completely asymptomatic.
If you do not treat mycoplasmas in women, this is fraught with the occurrence of various inflammatory diseases, changes in the structure of sperm, which lead to male infertility, pathologies during pregnancy, and female infertility. Pathologies during pregnancy in women who more often suffer from this disease can manifest themselves in a variety of ways. This could be a miscarriage, non-developing pregnancy, premature birth, fever, premature rupture of amniotic fluid. As a result, the child may be infected at birth; among other consequences of this infection, it is worth noting the likelihood of pneumonia and eye damage in the baby. In newborn girls with mycoplasmas, the organs of the genitourinary system may be affected.
Complications
The cause of the consequences in the presence of this pathology is bacteria of the type Mycoplasmosis hominis, less often - Mycoplasmosis genitalium.
Possible complications:
- Urethritis is an inflammatory process in the urethra (urethra). Characteristic symptoms: itching, burning and pain in the urethra. As the bladder is emptied, the pain increases.
- Endometritis is a disease of inflammatory etiology, in which mycoplasmosis develops on the cervix and on the mucous membrane of the uterus. Clinical picture: the appearance of pain in the lower abdomen, discomfort, discharge with blood before and during ovulation. Often women suffering from this disease cannot become pregnant. If this happens, there is a high risk of spontaneous abortion in the first trimester.
- Cystitis is an inflammation of the bladder, pyelonephritis is an infectious disease of the kidneys.
- Vaginitis is a disease of the genital organs (particularly the vagina), in which a bacterial process causes damage to a specific area. In the area of destruction of the epithelium by mycoplasmas, burning and itching occurs. These symptoms are accompanied by copious discharge mixed with mucus and pus, which has an unpleasant odor. During sexual intercourse, a woman experiences increasing pain.
- Gardnerellosis (vaginal dysbiosis). Occurs when infected with mycoplasma species hominis.
- Salpingoophoritis is an inflammatory process that develops in the fallopian tubes, uterine appendages, and ovaries. Due to damage to the uterine mucosa by pathogenic bacteria, swelling occurs, which often causes obstruction of the fallopian tubes and, as a result, infertility.
- Pathological processes during pregnancy. Miscarriages and early births are often caused by damage to the endometrium of the uterus, which is unable to ensure a full pregnancy and vital activity of the fetus.
- Infertility. Due to the appearance of salpingoophoritis and endometritis, the entire genital area becomes infected with mycoplasmas, and the woman is unable to become pregnant. In such a situation, the endometrium of the uterus is damaged, and the fertilized egg is rejected by the affected tissue. The inflammatory process contributes to swelling of the walls of the fallopian tubes, which leads to blocking the path for sperm. As a result, the likelihood of conception is minimized.
- Autoimmune diseases are a malfunction of the immune system, which is forced to resist infectious and inflammatory processes for a long time.
Folk recipes
In some cases, traditional medicine recipes are effective for these diseases. But it should be noted that they can only help in the early stages of the disease. In addition, you should definitely first consult with your gynecologist, who will tell you whether home treatment for mycoplasma hominis in women or other similar infections will be effective.
Anti-inflammatory preparations are most often used. You need to take two tablespoons of St. John's wort leaves and four tablespoons of sweet grass flowers. Then you should mix these ingredients together, and after four tablespoons of raw material, pour 800 ml of water. The healing decoction is boiled for 10 minutes, then allowed to brew for a couple of hours and filtered. It should be taken one glass three times a day before meals.
Another method of treating mycoplasma hominis at home in women involves douching with medicinal herbs. In this case, boron uterus and oak bark are used. Two tablespoons of bark are mixed with one tablespoon of boron uterus, and then poured with boiling water (one and a half glasses is enough). The healing agent must be infused for half an hour. The finished infusion should be filtered and then used for vaginal douching twice a day. Let us note that this method causes numerous controversies; some doubt its safety, but healers actively use it.
Mycoplasmosis during pregnancy
During pregnancy, any existing infections in a woman’s body worsen, which contributes to the development of complications, in particular: polyhydramnios, miscarriages, rupture of membranes caused by inflammation of the vaginal walls and, as a result, premature birth.
Most often, during delivery (when the fetus passes through infected tracts), the fetus (usually female) becomes infected. Against the background of this pathology, after artificial termination of pregnancy or childbirth, there is a high probability of developing endometritis.
Mycoplasmosis in pregnant women is a fairly serious disease that cannot be ignored. If mycoplasmosis is diagnosed during this period, a woman must undergo a course of treatment. It is recommended to do this in the first trimester of pregnancy, since in the future taking medications can negatively affect the development and health of the fetus. This pathology can provoke the development of various abnormalities in the first weeks of pregnancy: spontaneous miscarriage, placental abruption, etc.
In addition, this infection often causes ectopic pregnancy, which makes conception difficult. This disease in chronic form often contributes to the development of secondary infertility.
Effective drugs in the fight against mycoplasmosis
The main medications used in the treatment of mycoplasma are antibiotics that can affect the reproduction of microorganisms or slow down their growth. Often the doctor prescribes the following antibiotics to the patient:
- tetracycline;
- sumamed;
- amoxiclav;
- doxycycline;
- azithromycin;
- Solutab.
Medicines are prescribed to the patient in the form of dosed tablets or injections, depending on the course of the disease. The period of treatment is determined by a qualified doctor. An individual approach is applied to pregnant women. And children are prescribed medications with the least side effects on the body. For people treated for mycoplasma and uriaplasma using antibiotics, this helps get rid of the disease in 95% of cases. If the pathogen does not die during the first attempt, repeated treatment and other antibacterial drugs are prescribed. In addition, additional treatment is possible using the following methods:
- suppositories for topical use;
- douching;
- immunomodulators (multivitamins, aloe or echinacea tinctures);
- physiotherapy;
- proper nutrition.
It is important to understand that mycoplasmosis cannot be treated with traditional methods, so you should not waste precious time and money. The choice of the correct treatment depends on the pathology of the disease, its duration and the characteristics of the patient’s body.
Prevention is reliable armor against disease
To protect yourself from unexpected “guests” - mycoplasma or uriaplasma, it is important not to forget about prevention. Following simple rules will help you avoid the disease:
- use a condom during sexual intercourse;
- carry out treatment on time;
- do not change sexual partners, have one proven partner;
- regular visits to a gynecologist, at least once every six months;
- support immunity all year round.
As mentioned above, the mycoplasma pathogen can infect the respiratory tract. As a result of this, the disease takes on different forms. For example, acute respiratory infections, bronchitis and tracheitis, as well as mycoplasma pneumonia. Infection mainly occurs through airborne droplets when a patient coughs. Therefore, preventive measures will certainly become real armor in the fight against the disease.
Diagnostics
There are no characteristic clinical symptoms indicating the presence of mycoplasmosis. As a rule, they are manifested by an inflammatory reaction of the genital or urinary tract, so the main criterion for a patient’s infection is the results of a laboratory examination.
Despite the variety and perfection of laboratory research methods, a gynecological examination is also recommended. This is due to the fact that this pathology can be combined with other infections that arise due to disturbances in the vaginal microflora or are sexually transmitted. To prescribe a treatment regimen, it is necessary to diagnose the full range of possible lesions of the genital area.
Diagnosis of mycaplasma infection includes:
- A conversation with a doctor. During a consultation with a specialist, an anamnesis of the disease is compiled. The doctor is interested in chronic gynecological diseases, the health status of the sexual partner, as well as the presence of sexually transmitted diseases in the past.
- Gynecological examination. This is a mandatory procedure if symptoms of inflammation of the urogenital system occur. It includes examination of the cervix, vaginal mucosa and external cervical os. Most often, this examination reveals inflammation of the vaginal mucosa and copious mucopurulent discharge.
Laboratory examinations
During the diagnostic examination, the doctor takes biomaterial (from the mucous membranes), which allows you to most accurately identify the presence of mycoplasma infection. Also an effective diagnostic method is PCR testing and bacteriological examination (allowing to identify concomitant sexually transmitted infections).
Specifics of laboratory diagnostic methods:
- Serological examinations (PIF, ELISA) - prescribed to identify certain antibodies to the pathogen. However, this method does not indicate the dynamics of the process and the development of the infection, and also does not allow determining the effectiveness of the prescribed treatment.
- PCR diagnostics. This method accurately detects even a small population of microbes. Thanks to this diagnostic method, it is possible to reproduce the genetic material of the infectious agent, as well as its identification. This examination is the main one in diagnosing this pathology.
- Microscopic and bacteriological examination of a smear. This method allows you to identify concomitant diseases (fungal or bacterial vaginosis, trichomoniasis, gonorrhea). With its help, it is possible to promptly identify all existing infectious diseases, including chronic ones.
As a result of a full comprehensive examination, a gynecologist has the opportunity to establish a diagnosis and prescribe adequate treatment.
How does it affect pregnancy?
Mycoplasmosis is dangerous for the health of a pregnant woman, as it causes rejection of the fertilized egg and leads to the development of a miscarriage. Also, the causative agent of an infectious disease can be transmitted to a child in utero. In this case, the perinatal form of the pathology in question develops. Since a sexually transmitted infection cannot be eliminated without the use of antibiotics, pregnant women should receive treatment only after childbirth. The reason is the high probability of penetration of antibacterial drugs through the placental barrier, causing harm to the fetus. Even the use of the antibiotic Josamycin can lead to the development of anatomical defects in a child. The risk to the fetus from administering this drug is greater than the benefit to the mother.
Treatment
If test results show the presence of Mycoplasma hominis or genitalium species in the body, this is not a reason to prescribe treatment. How to treat mycoplasmosis in women is determined by the doctor according to the presence of concomitant ailments, the development of which can be caused by Mycoplasmi (inflammation of the bladder, uterus and appendages, urethra, kidneys, gardnerellosis). Only a doctor can prescribe treatment and prescribe medications, since self-medication can lead to serious complications and chronicity of the process.
In case of infection with a bacterium of the Mycoplasma hominis species, therapy is prescribed similar to that prescribed for gardnerellosis (bacterial vaginosis). If the mucous membrane has become a breeding ground for bacteria of the species Mycoplasma genitalium, this pathology is treated according to a scheme identical to the treatment of ureaplasmosis.
If mycoplasmosis is accompanied by various complications, treatment with antibacterial drugs is carried out, which involves the simultaneous use of several types of antibiotics. In addition, other effective methods are used - drip administration of medicinal solutions into the urethra, immunotherapy and physiotherapy.
It is advisable for both partners to undergo treatment, otherwise if one recovers, there is a high risk of re-infection.
Drugs
After conducting a sensitivity test for the treatment of mycoplasmosis, the doctor will prescribe one of the antibiotics:
- Clarithromycin - one tablet contains 250 mg of the active substance, drink twice a day. The course of treatment depending on the stage of the disease is 1-2 weeks;
- Doxycycline - recommended at a dosage of 100 mg, taken twice a day. Duration of treatment – 10-14 days;
- Levofloxacin – contains 250 mg of the active substance, it is recommended to take one tablet for three days;
- Josamycin (Vilprafen solutab, Vilprafen) – dosage 500 mg, drink three times a day. The course of treatment is 10 days;
- Ofloxacin - permissible dosage is 200-400 mg. Take once;
- Clindamycin - recommended dosage of 200-400 mg. Take the drug every 6 hours. Duration of treatment is one week.
- Azithromycin . There are two regimens for taking this medicine: 1 g once (2 tablets of 0.5 g each) or 0.25-0.5 g once a day for 2-5 days. Azithromycin is recommended to be taken one hour before meals or two hours after.
Chronic form
In the treatment of this pathology in a chronic form, great importance is given to local therapy and treatment of the immune system. The goal of such therapy is to correct and strengthen the immunodeficiency state, which has become one of the causes of the chronic course of the disease and has significantly intensified against its background. Treatment is prescribed taking into account the results of the immunogram.
Local therapy is prescribed simultaneously with systemic antibiotic therapy. In most cases, such treatment lasts no more than one week. In this case, anti-inflammatory, ethmotropic drugs and enzymes (chymotrypsin, trypsin, etc.) are prescribed in the form of installations or using cotton-gauze swabs to treat the vagina.
After its completion, patients are recommended to undergo a course of treatment with drugs to restore microflora (probiotics).
Requirements
During treatment of mycoplasmosis, you should adhere to some rules:
- during therapy, stop intimate relationships;
- follow the doctor’s instructions until complete recovery;
- when taking medications, strictly follow the instructions of the gynecologist;
- do not stop the treatment regimen until control tests are carried out;
- Be sure to follow a diet: exclude fatty, fried, spicy, salty foods, as well as smoked and fast food.
How to treat mycoplasmosis
Treatment of mycoplasmosis is carried out only when an accurate diagnosis is established after certain laboratory tests.
Mycoplasmosis can only be diagnosed after laboratory tests.
Due to the too small size of mycoplasma, it is impossible to determine the infection during a routine gynecological examination or by taking a smear of the vaginal microflora. Usually, if there is no suspicion of mycoplasmosis, tests to detect it are prescribed last.
Tests for mycoplasma in women:
- The bacteriological method (growing microflora in biomaterial taken from the patient) takes from 4 to 7 days and is the most accurate diagnostic method.
- PCR method - detects the presence of mycoplasma DNA in a smear, the fastest method (result in 30 minutes), but also the most expensive;
- The immunofluorescent method is a special dye that detects fragments of mycoplasma.
For a final diagnosis, one of the listed diagnostic methods is sufficient. But after 2-3 weeks, the study should be repeated to exclude false results.
The treatment regimen is prescribed taking into account the individual characteristics of the patient: age, presence of symptoms, severity, degree of prevalence, etc.
Important! Treatment should be carried out simultaneously in both sexual partners. Otherwise, therapy does not make sense due to the risk of re-infection.
Treatment of mycoplasma in women is a very complex process, because... the infection is resistant to some antibiotics. But you can’t do without antibacterial therapy - the latest generation drugs are prescribed (cephalosporins and penicillins are useless for mycoplasma): Erythromycin, Sumamed, Azithromycin, Doxycycline.
The course duration and dosage are determined individually. In most cases, antibacterial therapy helps cure mycoplasmosis, but there may be cases where the disease cannot be defeated the first time. Then a repeat course of therapy is prescribed, replacing the antibiotic.
In addition to taking antibiotics, the following treatment regimen is prescribed:
- Local treatment: antipruritic and anti-inflammatory ointments and suppositories, as well as antibacterial suppositories containing clindamycin and metronidazole, douching with antiseptic agents.
- Physiotherapy (ozone therapy, magnetic laser therapy);
- Taking immunomodulatory drugs: Likopid, Cycloferon;
- Probiotics (to eliminate the harmful effects of antibiotics on the intestinal microflora).
- Vitamin therapy.
During treatment, it is advisable to avoid sexual intercourse and follow a certain diet, which the doctor will recommend. Two weeks after the end of the course of therapy, you need to re-test for mycoplasma.
Note! During treatment for mycoplasmosis, it is recommended to drink plenty of fluids to help the body remove toxins produced by the destruction of mycoplasma.
Traditional methods are powerless in the fight against mycoplasmosis - traditional recipes can only help strengthen the immune system and prevent re-infection.
Prevention
The main methods of preventing this pathology include:
- use of barrier methods of contraception;
- visit a gynecologist every six months for examination;
- enter into intimate relationships with one partner;
- support immunity;
- timely detection and treatment of other sexually transmitted infectious diseases.
Important! When planning a pregnancy, it is necessary to undergo a comprehensive examination of the body to avoid possible sexually transmitted infections.
Mycoplasmosis in women is an insidious disease that can lead to serious complications even in the absence of minor symptoms. At the first manifestations of this pathology, it is recommended to visit a specialist. If treatment of the disease is started in a timely manner, the patient with mycoplasmosis has a favorable prognosis. In this case, a complete recovery without any complications is possible.
What is mycoplasma
In terms of development, mycoplasma is between viruses and bacteria. But scientists still have not decided which classification to classify these tiny microorganisms into. Therefore, mycoplasmas are considered opportunistic pathogens.
A unique feature of mycoplasmas is the absence of a cell wall.
This means that they are capable, like viruses, of remaining in the body for a long time without causing any harmful effects, but under the influence of certain factors they can be activated and cause disease.
Note! Normally, mycoplasmas can be present in small quantities in the genitourinary system of men and women. Moreover, their carriers can be absolutely healthy people.
Mycoplasmas have a unique feature - they do not have a cell wall. This allows microorganisms to live outside the cell, settling on the epithelium of the respiratory organs or genitourinary system, and gradually penetrating into their thickness. This same feature makes it possible for mycoplasmas not to accept antibiotics, because The action of these drugs is aimed at destroying cells.
There are many types and subspecies of mycoplasmas, but only three of them can cause inflammatory diseases in women:
- Mycoplasma hominis causes various vaginoses in women;
- Mycoplasma genetalium - provokes exacerbation of pathologies of the genitourinary system;
- Ureaplasma Urealictum - causes urogenital inflammation.
In terms of the frequency of cases among sexually transmitted infections, ureaplasma and mycoplasma are ahead of even classic gonorrhea and syphilis. This prevalence of the disease poses a real threat to women’s health, especially reproductive function.