Features of blood as living tissue
Blood performs a huge number of functions, including the function of transporting oxygen from the lungs to all tissues of the human body, the function of transporting nutrition, the function of transporting salts to minerals, the function of removing waste products from cells and tissues, the function of thermoregulation, the function of a buffer solution that regulates the acidity of the environment .
In addition, blood carries hormones, enzymes and performs many other functions, for example, protects the body from harmful microorganisms and even takes part in the regulation of respiration (it is carbon dioxide dissolved in the blood that stimulates the respiratory center in the brain).
Therefore, the health of this living tissue and the constancy of its composition is the key to the well-being of that huge and complex system that is the human body, and any disturbances in its work one way or another are reflected in the composition of the blood.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Since a child’s body is more vulnerable to any disease than an adult’s body, a blood test in a child as a method of early diagnosis becomes especially important.
Preparing for the study, how and when to take it correctly
Normal indicators of a general blood test in children may differ and depend on the time of day the test is taken and on how full the child is.
It is recommended to take blood in the morning on an empty stomach from a finger (or from a vein), but failure to comply with this recommendation is not critical.
Another thing is important - if during the period of one illness the baby donates blood more than once, then it is advisable to do it the same way - either hungry every time, or well-fed every time, at the same time.
It’s easier to negotiate with a well-fed child.
Blood is taken from a vein using a syringe, and from a finger - either with a scarifier or a lancet.
A scarifier is a specially shaped needle; it must be individually packaged.
A lancet is more complicated and more expensive; when used, pain is minimized, and the likelihood of bringing the baby to the laboratory the next time without hysterics increases many times over.
No matter how difficult it may be to distract yourself from the child and his worries immediately before this procedure, try to do it.
You must be sure that the laboratory technician who works with him uses rubber gloves, which he disinfects after each patient, or, even better, works in disposable gloves.
Should I give immunostimulants to children? Opinions for and against are presented in our review of popular drugs.
An overview of effective vitamins for improving immunity in children is presented in this article.
And here we’ll talk about what vitamins to give a child for growth.
Decoding the research results
Blood tests should be interpreted by professionals in a laboratory or hospital. In order to understand that something is wrong with a child and make a scientifically based assumption about what kind of disease it may be, a nurse’s qualifications are sufficient, but to make an accurate diagnosis in case of deviation from the norm, the help of more qualified and specialized specialists - hematologists (blood specialists), endocrinologists (specialists in the endocrine glands and the hormones they secrete).
It is extremely undesirable for a non-professional to decipher the analysis, since without special education one can easily make a mistake. Moreover, it is impossible to take measures based on data that was interpreted by a non-specialist without the help of a doctor. This can lead to serious damage to the child's health.
When decoding, the following indicators are usually taken into account:
- Blood color;
- Amount of hemoglobin;
- Red blood cell count;
- Type of red blood cells (when examined under a microscope);
- Number of immature red blood cells;
- Leukocyte count;
- Quantitative relationships between different types of leukocytes;
- Platelet quantity and quality;
- Erythrocyte sedimentation rate;
- Amount of glucose (when donated for sugar);
- Other substances and their ratio.
Blood composition reflected in the analysis
As a rule, a blood test in children consists of not only an infinite number of numbers, but also Latin characters. These are substances that are part of the blood and actively respond to various changes in the body of children. Any disease can change the chemical composition of a child's blood, and this is what the general analysis reflects. The decoding of these symbols can actually be quite clear even to the average person.
- Hemoglobin (a blood test will contain the Latin designation Hb) is a protein that delivers carbon dioxide to the lungs and oxygen to the tissues.
- Color indicator - the ratio of the number of red blood cells and hemoglobin to normal values.
- Red blood cells (RBCs) are one of the most basic cells in the blood and are called the “containers” of hemoglobin.
- Hematocrit (PCV, Hct: stands for Packed Cell Volume) - an indicator of blood thickness.
- Reticulocytes are new red blood cells that are always present in the blood.
- Platelets are cells responsible for blood clotting.
- White blood cells (the test contains the abbreviation WBC) are cells that represent the immune system. One of the most important indicators, which contains a general blood test in children: it is this that allows doctors to accurately determine the cause of the disease. It will be useful for parents to know that the number of leukocytes in a child is much higher than in adults, and this is considered normal.
- Neutrophils are cells that are active against bacteria. The more pronounced the bacterial inflammatory process in children, the higher the number of neutrophils.
- Metamyelocytes, myelocytes, are a type of leukocytes that appear in critical cases, helping the body fight with all its might.
- Eosinophils - these cells react to the “antigen-antibody”.
- Lymphocytes - blood cells involved in immune processes, are responsible for immunity (detect, recognize, destroy antigens). This is also a type of leukocyte. An increase in this indicator in children may be a sign of a viral infection.
- Monocytes are cells that engage in phagocytosis (absorb, digest bacteria, dead cells, etc.).
- Plasma cells - participate in the formation of antibodies. If the analysis detects an increase in this indicator, most likely, viral infections will be detected in children.
Useful: Eye drops for newborns
To make the interpretation of a blood test in children more complete, it will be useful for parents to learn about such an indicator as the erythrocyte sedimentation rate in the blood (abbreviated in the analysis as ESR). This is the length of a column of red blood cells deposited in an hour (measured in mm/h). An increased ESR in children is a direct indication of the presence of an inflammatory process in the body. Knowing the chemical composition of blood, it will be much easier to read what is indicated in the test results.
Red blood cells are one of the most important types of blood cells; they provide oxygen saturation to the body
Norm of indicators in the table
Let's look at the basic blood standards for children in the form of a table:
| Index | Age | Normal value |
| Red blood cells | 0-1 month | 3,6-6,2 |
| 1-6 months | 2,7-4,5 | |
| 6-12 months | 2,7-4,5 | |
| Older | 3,7-5,3 | |
| Hemoglobin | 0-1 month | 180-240 g/l |
| 1-6 months | 105-170 | |
| 6-12 months | 110-140 | |
| Older | 100-140 | |
| Leukocytes | 0-1 month | 6,5-14 |
| 1-6 months | 5,5-12,5 | |
| 6-12 months | 6-12 | |
| Older | 6-17 | |
| Platelets | Everyone has | 160-300*10 in 9/l |
| ESR | 0-1 month | 2-4 mm/h |
| Older | 4-10 |
How to decipher the results
Let's take a closer look at each indicator, its normal value, function in the blood and the reasons for the change.
Important! We are used to the fact that the interpretation of the analysis is a laboratory assistant with test tubes and reagents. However, modern clinics use medical equipment that can perform blood tests based on basic parameters automatically.
Hemoglobin
The hemoglobin level in newborn babies is much higher - up to 240 g/l. By the month of life, the indicator decreases and until adulthood ranges from 110 to 175 g/l, gradually lowering its upper threshold.
An increase in hemoglobin levels occurs when water is removed from the body due to increased sweating, taking diuretics, diarrhea, vomiting, and a small volume of fluid intake.
Video: what is hemoglobin and its norms The following reasons can also be identified:
- congenital defects or insufficiency of internal organs (heart and lungs);
- disease of the blood-forming organs (erythremia);
- kidney diseases.
The condition of the body with low hemoglobin levels is called anemia. Anemia can be determined by external signs:
- headache;
- drowsiness;
- increased heart rate;
- pale skin color.
We recommend reading about what the normal hemoglobin level is for a baby, what to do if your hemoglobin is high, and how to lower your hemoglobin level if it is low.
Often, a decrease in a child’s hemoglobin level occurs due to a lack of vitamins and iron in the body. This is easily corrected at any age. But there are also more serious reasons - blood loss, congenital blood diseases, leukemia.
Red blood cells
Red blood cells carry oxygen in the blood, delivering it to all human tissues and organs. This disk, concave on both sides, contains hemoglobin in almost its entire volume. Therefore, the reasons for a decrease or increase in the level of red blood cells in a child’s blood practically coincide with those that cause fluctuations in the amount of hemoglobin.
After a slight surge in the content of red blood cells in the first days after the birth of a child (4.3-7.6 x 10 to the 12th power of cells per liter of blood), with the subsequent development of the body this figure decreases to the range of 3.5-4.8 until reaching adulthood.
Important! Red blood cells can die from toxic effects, as well as autoimmune lesions.
Color
The color index of a child's blood remains unchanged during his growth - both in a newborn baby and in a 16-year-old teenager, the color norm should be in the range from 0.8 to 1.15% with a slight decrease in the upper threshold.
It is logical that when the blood thickens, its color darkens and becomes more saturated. This can be caused by the same diarrhea, dehydration, insufficient functioning of organs (heart, lungs). The anemia already mentioned above can cause blood thinning and, as a result, a change in its color to a lighter color.
Reticulocytes
In the process of blood formation, reticulocytes degenerate into erythrocytes and become their basis. Their number in a growing child is extremely low (less than 1 percent of the number of red blood cells) and, as a result, they are transformed into red blood cells.
The maximum number of reticulocytes is observed at birth and on the first day of life, when the content of these cells ranges from 30 to 51 ppm. Over the course of a month, the indicator decreases by an order of magnitude, and subsequently, up to adulthood, is at the level of 3-12 ppm.
Leukocytes
White blood cells in the human body work as phagocytes, that is, they counteract infectious agents, dead cells, cell breakdown products, and foreign substances. Leukocytes capture substances harmful and foreign to the blood and digest them.
The maximum concentration of such cells is observed in newborn infants - from 8.5 to 24.5. As the child grows up, the number of leukocytes gradually decreases to a maximum of 9.5 in a unit of measurement of 10 to the 9th power of cells per liter of blood.
The reasons for the increase in the level of leukocytes can be both physiological and the body’s reaction to external damage.
Physiological ones include:
- eating (one of the reasons why you need to donate blood for analysis on an empty stomach);
- graft;
- emotional factors (pain, stress, prolonged screaming).
Video: an increase in the level of leukocytes in the blood of a child External factors for an increase in leukocytes:
- injuries that caused tissue damage (severe bruises, burns);
- inflammatory and purulent processes (from sinusitis to appendicitis);
- postoperative period;
- oncological diseases.
We advise you to read about what an increase in leukocytes in the blood means, what the meaning of a low level of lymphocytes in a child’s blood is, and also what can cause leukocytes in a child’s stool and urine.
Rod
Neutrophil granulocytes are a subtype of leukocytes. Band neutrophils are still immature and have a solid rod-shaped nucleus without division. There are quite a lot of such neutrophils at birth - from 1 to 17%, but during the first month of life, the figure decreases to the normal level for both a child and an adult - 0.5-6%.
It will be useful for you to read about what neutrophils are in a child’s blood, what to do if a child’s neutrophils are low or high.
Segmented
This is the main type of leukocytes, the number of which changes significantly in the first year of life from a surge at birth (up to 80%), to a sharp decrease during the first 12 months to the norm of 15-45%. After which, until adolescence, the content of segmented neutrophils in the blood gradually increases.
Neutrophils, whether segmented or band, are capable of emigrating through the walls of blood vessels of the circulatory system and tend to move to sites of damage or inflammation.
Eosinophils
An eosinophil, like a neutrophil, is a granulocytic leukocyte. The cell received its name because of its ability to be stained only with the dye eosin. Eosinophil, capable of binding histamine, has antiallergic properties.
Find out what elevated eosinophils and red blood cells in a child’s urine mean.
This type of leukocyte does not stay in blood vessels for long, as it prefers to migrate into tissues and remain there. In a child’s body from the first days of life until adulthood, eosinophil is present in almost the same concentration - from 0.5 to 6%.
Basophils
This type of leukocyte differs from eosinophils in the structure of the nucleus, which is not always noticeable during examination. Basophils do not stain when exposed to the acidic dye eosin, and absorb the basic dye with high intensity.
This leukocyte is actively involved in the rapid spread of allergies (anaphylactic shock). The level of basophils in the blood of children remains the same throughout the entire period from birth to adulthood and ranges from 0 to 1%.
Lymphocytes
A type of white blood cell that is the main type of cell of the human immune system, providing cellular immunity. In adolescent children, the level of lymphocytes in the blood is 50% of the total number of leukocytes. Before this age, the number of lymphocytes is slightly higher.
Platelets
These blood elements are necessary to close the damaged area of the vessel. They can promote tissue regeneration by releasing so-called growth factors that help cell renewal and division. The normal platelet count for a child of any age is from 160 to 400 in a unit of measurement of 10 to the 9th power of cells per liter of blood.
An increase in the level of these cells occurs due to anemia, inflammatory processes, and also during the postoperative period. A low platelet count can be directly related to the process of bearing and childbirth - prematurity, genetic blood diseases in children.
Did you know? A blood test is usually taken from the ring finger, since it is least used in everyday life and the wound on it brings less inconvenience.
Red blood cells
Red blood cells are red formed elements that have the shape of “dumplings” (biconcave disks). These elements were once cells, but then lost their nucleus and turned into carriers of hemoglobin, which can equally easily combine with oxygen or carbon dioxide. This allows red blood cells, moving from the lungs to other organs and tissues, to carry oxygen, and moving back to the lungs, to carry carbon dioxide.
There is always a small amount of reticulocytes in the blood - immature red elements that still retain remnants of the nucleus. During bleeding and some diseases, reticulocytes begin to be actively released into the blood without having time to mature in order to replenish the number of red blood cells. Therefore, with a microscopic examination, it is possible to determine whether the child has recently had blood loss or blood diseases leading to the destruction of red cells.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Another important indicator is the amount of hemoglobin , which largely depends on the presence of iron in the body and its normal metabolism. It is hemoglobin that forms the scarlet color of blood.
Finally, the shape of the red blood cells can be seen under a microscope. Deviation from the norm usually indicates severe hereditary diseases of the child.
Deviations from the norm: possible causes
If the analysis shows deviations from the norm in the child’s blood, it is necessary to clarify what they could mean. This often happens in children due to the fact that the analysis is taken on a full stomach, which is strictly recommended. If the problem is still a disease, you will need to consult a doctor and, most likely, treatment.
Hemoglobin
Elevated:
- dehydration;
- congenital lung (heart) defect;
- pulmonary (heart) failure;
- pathologies of the kidneys and hematopoietic organs.
Reduced:
- anemia;
- leukemia;
- lack of iron and vitamins;
- exhaustion;
- great blood loss.
Red blood cells
Increased quantity:
- dehydration;
- diseases of the hematopoietic system;
- respiratory (heart) failure.
Reduced quantity:
- poor nutrition;
- large blood loss;
- leukemia;
- hereditary pathologies;
- hemolysis.
Leukocytes
Increased quantity:
- after eating, active physical activity, vaccinations, operations;
- inflammatory reaction;
- purulent-inflammatory process;
- burns, serious injuries;
- oncology.
Reduced quantity:
- infectious, viral diseases;
- leukemia;
- hypovitaminosis;
- use of certain medications;
- radiation sickness.
Color index
Overpriced:
- erythremia;
- dehydration;
- cardiac (respiratory) failure.
Understated:
- renal failure;
- anemia.
Neutrophils
A lot of:
- infections;
- infectious processes;
- inflammation of internal organs;
- metabolic disease;
- oncology;
- after vaccinations;
- taking immunostimulating drugs.
Few:
- infectious diseases;
- blood diseases;
- heredity;
- after radio- or chemotherapy;
- taking certain medications.
Leukocyte formula
Shift left:
- infectious, inflammatory processes;
- acute blood loss;
- diphtheria;
- pneumonia;
- scarlet fever;
- typhus;
- sepsis;
- intoxication.
Shift right:
- poisoning from radiation waste;
- B12-deficiency anemia;
- lack of folic acid;
- chronic lung diseases;
- obstructive bronchitis.
Helpful: What teas can be given to infants?
Eosinophils
Increased level:
- allergy;
- parasitic diseases;
- infections;
- oncology;
- blood diseases.
Reduced level:
- intoxication;
- sepsis;
- purulent processes;
- the beginning of inflammation.
Monocytes
Promotion:
- infections;
- after acute inflammation;
- tuberculosis;
- brucellosis;
- sarcoidosis;
- diseases of the hematopoietic system;
- phosphorus poisoning.
Demotion:
- anemia;
- leukemia;
- purulent lesions;
- after operation;
- taking steroid drugs.
Basophils
A lot of:
- chicken pox;
- allergy;
- nephrosis;
- anemia;
- taking hormonal drugs.
Lymphocytes
Promotion:
- viral infections;
- ARVI;
- blood diseases;
- lead, arsenic poisoning;
- taking certain medications.
Demotion:
- tuberculosis;
- lupus erythematosus;
- anemia;
- oncology;
- renal failure;
- AIDS;
- radio and chemotherapy.
Platelets
Increased level:
- inflammatory processes;
- anemia;
- after operation;
- oncology;
- physical fatigue.
Reduced level:
- congenital blood diseases;
- lupus erythematosus;
- infections;
- anemia;
- blood transfusion;
- prematurity;
- hemolytic disease in newborns;
- heart failure.
If parents have a blood test for their children, deciphering these indicators will help them calm down or take the necessary measures to maintain the health of their child.
Leukocytes
Leukocytes have the ability to move outside the bloodstream and perform the function of protecting the body from infectious agents (unicellular and precellular life forms) and its own mutated cells (cancerous or benign tumors). They are also able to secrete many chemicals that serve to regulate body functions, “remember” a problem they once encountered, etc.
White blood cells are very diverse, and their functions are divided between different species, just as functions are divided between castes of insects or branches of troops in armies. In various diseases, the number of precisely those leukocytes that are needed to fight a specific disease increases. Therefore, by the ratio of the types of leukocytes to each other, one can judge not only that the body is not healthy, but also what kind of disease has struck it.
For example, an increase in the number of neutrophils indicates inflammation, and eosinophils indicate severe allergies.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Children rarely experience a decrease in the number of leukocytes (usually this situation occurs with bone marrow lesions), but often there is an increased content due to injuries, burns, abrasions and other consequences of childhood pranks. This must be taken into account when interpreting the results of the analysis.
Interpretation of blood tests in children table
A general blood test (CBC) or “clinical” is a popular laboratory diagnostic technique in pediatrics.
It helps the specialist assess the child’s health and identify abnormalities if they are present. Therefore, OAC is prescribed to children for various diseases in order to find the root cause of the problem and select rational treatment. For example, if the disease is caused by a viral infection, then appropriate treatment is required, not antibacterial. This analysis can indicate the nature of the disease.
The results of a general blood test can be affected by a number of factors, which we will discuss below.
First of all, if the child already understands where he is being taken, then you can play doctor. Let the baby take blood from toys himself, and then go see how a specialist does it. A child will not be afraid to go to the clinic if doctors do not frighten him from childhood. It’s better to play doctor more often and visit specialists as planned. Then people in bathrobes will not cause horror in the child.
Mothers and grandmothers often ask me how to properly prepare for the OAC. And this is the right question, because the accuracy of the results depends on it. The child is not yet able to do everything on his own, so responsibility for this lies with the parents.
Rules:
- The most favorable time for taking a general blood test is from 8-11 am.
- Quality and quantity of food. Blood is donated strictly on an empty stomach, 8-12 hours should pass from the last meal. But how can you withstand such a period with a small child? I agree, so for children this time can be reduced to 4-6 hours. By the way, “on an empty stomach” also means refusing to drink: tea, coffee, juices, soda, and also sugar and honey. Some people think that a light snack of cookies and tea won't hurt. But in the end, you can get erroneous blood values, and sometimes this is critical for doctors. You can drink plain water before the test.
- Taking medications also affects the composition of the blood. The day before the blood test, we stop taking medications. If this cannot be done, be sure to inform your doctor about this so that he can make an adjustment when taking into account the results.
- Physical exercise. Of course, nothing will happen from lightly swinging your arms or legs, but it is better to postpone activities in a sports club. Physical activity leads to changes in blood leukemia, hormone levels and glucose.
- Ensure quality sleep and a minimum of emotional stress. In the case of a general blood test, stress leads to an increase in white blood cells. If we are talking about a biochemical blood test, then here, too, experiences can affect the indicators.
- If the child is currently sick, the doctor should also be told about this. Diseases directly affect blood counts.
When the data from a child’s general blood test is in your hands, the question of decoding arises. Of course, this should be done by a specialist, but it is also important for parents to know what is going on with the baby’s health. Instead of the usual words “hemoglobin”, etc., you will find abbreviations in English. Below I give a list of what they mean.
The form also contains notes near the abbreviations:
- (%) - means the relative content of the element,
- (#) is the absolute content of the element.
It is important for parents to know that the child’s blood test standards differ from ours. Their body systems work differently, the immune system only continues to get acquainted with the outside world, and all this affects the blood. Therefore, do not be alarmed if you notice significant deviations when comparing with your parameters. Below you will find a table with blood test standards for children. You may want to save it because your readings change as your baby grows.
The diagnostic features of the medical institution should be taken into account. The laboratory may have its own equipment settings and reagent sensitivity.
Therefore, the indicators may differ slightly, and you need to pay attention to the standards that apply in a given laboratory. Indicators may differ depending on the chosen method of calculating results.
Today this is done by two methods: counting through a microscope by a specialist, or by an automatic analyzer.
Hemoglobin g/l:
- 0 - 7 days: 134-198;
- 7 - 30 days: 107-171;
- 1 month - six months: 103-141;
- six months - 1 year: 113-140;
- 1 year - 6 years: 100-140;
- from 6 years to 18 years: 120-150.
Red blood cells million/µl:
- 0 - 7 days: 4.0-6.6;
- 7 - 30 days: 3.6-6.2;
- 1 month - six months: 2.7-4.5;
- six months - 1 year: 3.7-5.3;
- from 1 year to 2 years: 3.7-5.3;
- 2 years - 6 years: 3.9-5.3;
- from 6 years to 18 years: 4.0-5.2.
Leukocytes thousand/µl:
- 0 - 7 days: 7.2-18.5;
- 7 - 30 days: 6.5-13.8;
- 1 month - six months: 5.5-12.5;
- six months - 1 year: 6.0-12.0;
- from 1 year to 2 years: 6.0-17.0;
- 2 years - 9 years: 4.9-12.3;
- from 9 to 18 years: 4.5-12.0.
Band neutrophils:
- Newborn: 1-17;
- 0 - 30 days: 0.5-4;
- from 1 month to 1 year: 0.5-5;
- 1 year - 18 years: 1-5.
Segmented neutrophils:
- Newborn: 45-80;
- 0 - 7 days: 30-50;
- 7 days – 1 year: 16-45;
- 1 - 2 years: 28-48;
- from 2 to 3 years: 25-35;
- from 4 to 5 years: 45-55;
- from 6 to 9 years: 38-58;
- 9 - 18 years: 43-60.
Eosinophils (%):
- 0 - 7 days: 1-6;
- 7 days - 1 year: 1-5;
- from 1 year to 2 years: 1-7;
- 2 years - 6 years: 1-6;
- from 6 to 18 years: 1-5.
Basophils (%): 0-1
Lymphocytes (%):
- Newborn: 15-35;
- 0-7 days: 22-55;
- 7 days - 12 months: 45-70;
- from 1 year to 2 years: 37-60;
- from 2 to 3 years: 45-67;
- from 4 to 5 years: 45-55;
- 6 - 9 years: 30-45;
- 9 - 15 years: 30-46;
- 15 - 18 years: 20-40.
Platelets thousand/µl: 180-320 (420).
ESR mm/h:
- Newborn: 2-4;
- 0-7 days: 4-8;
- from 7 days to six months: 4-10;
- from six months to 12 years: 4-12;
- from 12 to 18 years: level as in adults.
Take care of your children's health!
The results of a blood test can tell a lot about the child’s health status, his predisposition to certain diseases, and the effectiveness of treatment.
Therefore, a general blood test is taken from children both for preventive purposes and during treatment.
Blood is drawn from a finger, usually in the morning on an empty stomach; the procedure does not take much time and is not overly painful.
A general blood test is a very informative indicator for a doctor. This, at first glance, simple study gives an idea of the number, size and shape of red blood cells, and the hemoglobin content in them.
The analysis also shows the ratio of blood plasma volume and formed elements, allows you to determine the leukocyte formula, platelet count and erythrocyte sedimentation rate. All this speaks very eloquently about the patient’s health status.
Only a doctor can decipher and correctly interpret blood test data. However, you still need to have a general idea of the contents of the results sheet.
- Red blood cells (RBC) are the most numerous formed elements of blood containing hemoglobin.
- Hemoglobin (Hb) is the main component of erythrocytes (red blood cells). This is a complex protein, its main function is to transport oxygen from the lungs to the tissues, as well as to remove carbon dioxide from the body and regulate the acid-base balance.
- Average volume (CV) is one of the erythrocyte indices (along with MCH and MSHC). It is a quantitative assessment of red blood cell volume. The indicator is relative.
- Blood color index (MCI, Mean Corpuscular Hemoglobin) is the hemoglobin content in one red blood cell. Similar to MCHC (Mean Cell Hemoglobin) - the average concentration of hemoglobin in red blood cells.
- Reticulocytes (RTC) are young red blood cells. Their excess quantity indicates an increased need for the formation of new red blood cells caused by blood loss or disease.
- Platelets (PLT) are anucleate, colorless, spherical blood cells. They are responsible for blood clotting and play an important role in the healing processes of damaged tissues.
- Thrombocrit (PCT) is an indicator characterizing the percentage of platelet mass in the blood volume. A very important criterion for assessing the risk of bleeding and thrombosis.
- ESR (ESR) is the erythrocyte sedimentation rate and is an important indicator of the course of the disease.
- White blood cells (WBC) are a group of cells called white blood cells. They are characterized by the presence of a nucleus and lack of color. The role of white blood cells is to protect the body from microbes, bacteria, viruses and foreign cells.
- Leukocyte formula - represents the percentage of different forms of leukocytes in the blood serum. The indicator is determined by counting leukocytes in a stained blood smear under a microscope.
- Segmented neutrophils, or neutrophilic leukocytes, are the most numerous group of leukocytes. Their main task is to destroy pathogenic bacteria. Band neutrophils are also isolated. These are young neutrophils with a rod-shaped solid nucleus. As for neutrophil myelocytes, these are more mature cells that include protoplasm, colored pink. The youngest neutrophils are called metamyelocytes. They appear in the blood in the presence of an inflammatory process.
- Eosinophils (EOS) are cells found in the blood that perform a protective function and are an integral part of the leukocyte formula.
- Basophils (BAS) are the smallest group of leukocytes. An increase in the number of basophils occurs during allergic conditions, infections, diseases of the blood system, and poisoning.
- Lymphocytes LYM are blood cells that are part of the immune system. They circulate in the blood and tissues and provide protection against foreign agents entering the body.
- Monocytes (MON) are large white blood cells responsible for clearing the blood of physical agents and foreign cells. Monocytes can absorb both whole microorganisms and their fragments. If the number of monocytes in the blood is increased, this may indicate the presence of an infection in the body.
We suggest you familiarize yourself with How to cleanse blood with medication.
How to cleanse your blood of toxins yourself It is believed that there are about 1000 people with blue blood living on the planet; they are called kyanetics. The color of blood is due to the fact that it contains copper instead of iron. Children with blue blood are born to ordinary parents.
Such blood is less susceptible to infection and has greater clotting properties; even serious injuries do not cause severe bleeding. Therefore, the ancient knights of “blue blood” aroused fear and reverence among their relatives.
Such blood was considered a sign of chosen persons.
| Index | Age | Reasons for deviation from the norm | ||||
| newborn | 0-7 days | 7-30 days | 1 – 6 months | 6 -12 months | ||
| Hemoglobin | 180-240 | 134 – 198 | 107 – 171 | 103-141 | 113-140 | Above normal |
| Below normal | ||||||
| Red blood cells | 3,9-5,5 | 4,0-6,6 | 3,6-6,2 | 2,7-4,5 | 3,7-5,3 | Above normal |
| Below normal | ||||||
| Color index | 0,85-1,15 | 0,85-1,15 | 0,85-1,15 | 0,85-1,15 | 0,85-1,15 | Above normal |
| Below normal | ||||||
| Reticulocytes | 3-15 | 3-15 | 3-15 | 3-12 | 3-12 | Above normal |
| Below normal | ||||||
| Leukocytes | 8,5-24,5 | 7,2-18,5 | 6,5 -13,8 | 5,5 – 12,5 | 6-12 | Above normal |
| Below normal | ||||||
| Rod | 1-17 | 0,5- 4 | 0,5- 4 | 0,5- 5 | 0,5- 5 | Above normal |
| Below normal | ||||||
| Segmented | 45-80 | 30-50 | 16-45 | 16-45 | 16-45 | Above normal |
| Below normal | ||||||
| Eosinophils | 1 – 6 | 1 – 6 | 1 – 5 | 1 – 5 | 1 – 5 | Above normal |
| Below normal | ||||||
| Basophils | 0 – 1 | 0 – 1 | 0 – 1 | 0 – 1 | 0 – 1 | Above normal |
| Lymphocytes | 15 – 35 | 22 – 55 | 45 – 70 | 45 – 70 | 45 – 70 | Above normal |
| Below normal | ||||||
| Platelets | 180-490 | 180-400 | 180-400 | 180-400 | 160-390 | Above normal |
| Below normal | ||||||
| ESR | 2-4 | 4-8 | 4-10 | 4-10 | 4-12 | Above normal |
| Below normal | ||||||
Automatic (online) interpretation of blood tests for children and adults
| If you want to use the automatic decryption service, follow the link to the Online decryption service, enter your data and view the result. |
Video about clinical blood tests in children
| Index | Age | Reasons for deviation from the norm | ||||
| 1-2 years | 2-3 years | 3-6 years | 6-9 years | 9 -12 years | ||
| Hemoglobin | 100 – 140 | 100 – 140 | 100 – 140 | 120 – 150 | 120 – 150 | Above normal |
| Below normal | ||||||
| Red blood cells | 3,7-5,3 | 3,9-5,3 | 3,9-5,3 | 4,0-5,2 | 4,0-5,2 | Above normal |
| Below normal | ||||||
| Color index | 0,75-0,96 | 0,8-1,0 | 0,8-1,0 | 0,8-1,0 | 0,8-1,0 | Above normal |
| Below normal | ||||||
| Reticulocytes | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 | Above normal |
| Below normal | ||||||
| Leukocytes | 6,0 – 17,0 | 4,9-12,3 | 4,9-12,3 | 4,9-12,2 | 4,5-10 | Above normal |
| Below normal | ||||||
| Rod | 1 – 5 | 1 – 5 | 1 – 5 | 1 – 5 | 1 – 5 | Above normal |
| Below normal | ||||||
| Segmented | 28 – 48 | 32 – 55 | 32 – 55 | 38 – 58 | 43 – 60 | Above normal |
| Below normal | ||||||
| Eosinophils | 1 – 7 | 1 – 6 | 1 – 6 | 1 – 5 | 1 – 5 | Above normal |
| Below normal | ||||||
| Basophils | 0 – 1 | 0 – 1 | 0 – 1 | 0 – 1 | 0 – 1 | Above normal |
| Lymphocytes | 37 – 60 | 33 – 55 | 33 – 55 | 30 – 50 | 30 – 46 | Above normal |
| Below normal | ||||||
| Platelets | 160-390 | 160-390 | 160-390 | 160-390 | 160-390 | Above normal |
| Below normal | ||||||
| ESR | 4-12 | 4-12 | 4-12 | 4-12 | 4-12 | Above normal |
| Below normal | ||||||
Platelets
These are blood platelets - the smallest and most inconspicuous formed elements in human blood. They are responsible for ensuring that when injured, a blood clot forms, which closes the wound opening.
Platelets, like other formed elements, are released in the red bone marrow; their number can increase both with bone marrow lesions and with injuries, when the body responds to the call and increases the number of platelets in case of the next injury.
An increase in platelets may also be a consequence of iron deficiency. In this case, it will be associated with a drop in hemoglobin concentration. To avoid this, you need to give your child foods containing iron: liver, apples, hematogen .
As a side effect, an increase in platelets can be observed in infectious diseases of the gastrointestinal tract, in acute respiratory viral infections, and even in cancer, but in each of these cases it is accompanied by other, more important symptoms by which the cause can be determined.
And of course, stress can increase the level of platelets and leukocytes. Fear, transfer to another school or conflicts with peers have a serious impact on the child’s mental health, which can “spoil” a blood test .
Interpretation of indicator values
Based on the results of the UAC, the specialist checks the state of hemoglobin. It is assessed using three columns - hemoglobin, color index and the average hemoglobin content in one red blood cell.
The accuracy of the diagnosis and the correctness of treatment depend on the accuracy of the blood test results.
The following is also analyzed:
- hematocrit and an increased number of red blood cells (RBC) show whether the child is consuming enough fluid (we recommend reading: the child’s hematocrit is increased: what does this mean?);
- Neutrophils and eosinophils will help assess the baby’s immune reserve;
- the presence of inflammation is indicated by ESR;
- lymphocytes (LYM) and neutrophils indicate a viral or bacterial infection (we recommend reading: what to do if neutrophils in a child’s blood are low?).
Hemoglobin concentration (HGB)
Hemoglobin consists of protein and iron. Its main tasks are the binding of oxygen and its supply to the organs. The transport characteristics of blood, the functioning of the brain, lungs, heart, and the body as a whole directly depend on the saturation of hemoglobin. In the results, its concentration is designated Hb, HGB or hemoglobin.
A large amount of hemoglobin is characteristic of blood diseases, diabetes, various pathologies of the kidneys, heart, and lungs. When the level is low, the cause may be an unbalanced diet, congenital or acquired anemia, or leukemia.
Lymphocytes (LYM)
Lymphocytes belong to the leukocyte lineage and perform a protective function. Lymphocytes are most often designated by the abbreviations LY, LYM or LUM.
Depending on their purpose, they are divided into the following groups:
- B lymphocytes - responsible for immunity after the body collides with a virus or bacteria;
- T-lymphocytes are called killers - they are entrusted with the role of destroying any foreign cells;
- T-lymphocyte assistants are T-killers;
- Suppressor T cells are responsible for ensuring that healthy cells are not harmed;
- atypical ALY lymphocytes appear in children only when exposed to antigens.
LYM is calculated taking into account the total number of leukocytes, but absolute numbers are also found in the analysis results. In the latter case, the norm in children is considered to be 1-4 billion per liter. The absolute number of lymphocytes can be determined independently based on the results of a general blood test, using the formula: LC x LF% = LF, where LC is the number of leukocytes, and LF is lymphocytes as a percentage. If the required number according to the formula corresponds to the norm, there is no need to worry.
The normal level of lymphocytes in children is considered to be 30-70%. Moreover, the main part of them is found in tissues (tonsils, spleen, lymph nodes, bone marrow, appendix), and only 2 percent in the blood. Decoding the CBC includes an assessment of the content of lymphocytes in the body. If the latter are more than expected, the condition is called lymphocytosis. Otherwise – leukopenia.
Red blood cells (RBC)
Red blood cells (RBCs) help oxygenate the organs and tissues of the body, while they transfer the carbon dioxide released back to the lungs. Anisocytosis, or a decrease in red blood cells not due to a pathological condition, can be caused by excessive fluid intake.
An increased amount of rbc is extremely rare and is called erythremia or erythrocytosis. The reasons for such a deviation may be due to:
- presence of blood disease;
- physical activity;
- lung or heart problems;
- accommodation in mountainous areas;
- poisoning;
- dehydration.
White blood cells (WBC)
Leukocytes (WBC) are white blood cells that protect the body's immune forces, creating humoral and cellular immunity. An elevated reading during pregnancy or intense exercise is not considered a deviation. If these factors are excluded, the cause is an allergy, viral or bacterial infection. A low WBC count indicates weak immunity.
The ratio of all types of leukocytes as a percentage is displayed in the leukocyte formula. The MID data indicated in it makes the analysis more informative and allows you to immediately determine which leukocytes are outside the normal range.
Causes of increased wbc: injury, burn, liver disease, anaphylactic shock, malignant neoplasm, internal bleeding or renal colic. The impetus for a decrease in white blood cells is a viral disease, intoxication of the body, or an endocrine disorder.
Platelets (PLT)
Platelets are blood cells responsible for blood clotting. More precisely, they are entrusted with two tasks - creating a platelet aggregate when the walls of vascular beds are damaged and accelerating plasma coagulation.
The growth of platelets is called thrombocytosis - it is characteristic of an inflammatory or infectious process in the body, trauma and significant blood loss, hematological pathologies, leukemia, as well as the use of corticosteroids, sympathomimetics, and antimycotics. Thrombocytopenia, or low platelet levels, may be due to an allergic reaction, hemophilia, a virus, or a malignant tumor.
Erythrocyte sedimentation rate (ESR)
Erythrocyte sedimentation rate is an important non-specific indicator. Essentially, ESR means how quickly red blood cells settle and stick together in a test tube. With its help, the degree of the inflammatory process is determined. An increase in ESR is a slow process, and the same thing happens with a return to normal.
Neutrophils (NEUT)
Cells that resist any foreign formations are called neutrophils. They not only help the body cope with the disease, but also eliminate its own non-living microparticles.
Neutrophilia, when the number of cells is increased, can be of both physiological and pathological nature. In the first case, the trigger is stress or poor nutrition, and in the second, a number of diseases: burns, blood cancer, inflammation, blood loss, insect bites, removal of the spleen.
If the level of neutrophils is low, the condition is called neutropenia. It appears due to one of the reasons:
- flu;
- taking cytostatics and antibiotics;
- radiation;
- HIV;
- lack of vitamins;
- bone marrow depletion;
- toxoplasmosis;
- lupus;
- measles
Eosinophils (EOS)
The subtype of white blood cells responsible for detecting and eliminating foreign protein is called eosinophils. They help cleanse the body of toxins, parasites and actively fight cancer. Using the eosinophil count, the doctor determines whether the patient has an allergy. When the number of cells exceeds the norm, one of the following pathologies may be to blame:
An insufficient number of eosinophils indicates an inflammatory process. In addition, childbirth or infection of the body are provocateurs.
Monocytes (MON)
Monocytes are large immune cells that are another type of white blood cell. They recognize and cleanse tissues of viruses, bacteria, damaged cells, including tumor cells.
Monocytopenia can also occur due to blood cancer. Other reasons for its appearance: postoperative condition, taking hormonal drugs, osteomyelitis, phlegmon and abscess.
Basophils (BAS)
Basophils are a type of leukocyte that is the first to detect anything foreign in the body. They, one might say, “engage in battle” with toxic substances and allergens, resist inflammation and restore blood flow.
If the basophil count has increased, this may be due to a problem with the thyroid gland and lymphatic system, allergies, smallpox, or taking hormonal drugs. The decrease in basophils is affected by stress, pregnancy and increased levels of hormones.
ESR
Red blood cells are heavier than water. Moreover, they are heavier than blood plasma. Therefore, if the blood is left alone and not allowed to clot (this can be achieved simply by adding special anti-clotting reagents), the red blood cells will settle to the bottom, and pure plasma will remain on top.
The rate of this sedimentation is called ESR. The experiment itself can be carried out using different methods , but its essence is the same: a narrow test tube with blood is left vertically for a certain time, and then they look at how many millimeters the red blood cells have settled.
ESR changes with cancer, anemia, bone marrow diseases, damage by various microorganisms, and many other diseases.
Of course, ESR alone is not enough to make an accurate diagnosis , but it can suggest that something is wrong with the child’s body and become a reason for conducting other studies.
Immune cells - granulocytes
Immune cells in the blood are divided into several groups. The largest group of immune cells are neutrophils. Two forms of neutrophils are found in the blood: segmented and band.
An increased number of neutrophils occurs in response to bacterial infections and inflammatory processes.
Neutropenia - a decrease in the number of neutrophils may indicate damage to the bone marrow, exposure to toxic substances, and decreased immunity.
The release of immature forms of neutrophils into the blood indicates a severe inflammatory process.
If the number of immature forms of neutrophils increases, and mature forms cease to form, experts talk about a shift in the neutrophil formula to the left. This pathology can occur with cancer of the bone marrow.
Eosinophils are granulocytes that dissolve foreign proteins that enter the body.
The number of eosinphils increases when pathological agents penetrate the body. An increased number of eosinophils indicates helminthic invasion. The number of cells increases in diseases of the respiratory tract of a bacterial or allergic nature.
The disappearance of eosinophils from the blood is observed at the height of a severe infectious process. The appearance of eosinophils after a long absence indicates an improvement in the condition.
Basophils are the smallest group of granulocytes; they take part in the allergic response and change the permeability of cell membranes.
A high number of basophils is observed during allergic reactions and infections accompanied by the release of bacterial toxins into the blood, for example, chickenpox.
The total number of leukocytes increases with burns, injuries, cancer and purulent inflammatory processes.
A decrease in the total number of granulocytes is caused by vitamin deficiency and poor nutrition. The number of immune cells decreases when treated with corticosteroids.
Changes in red blood cells with a decrease in color index
Blood color index
The color index of blood is the proportional ratio of hemoglobin to red blood cells. Indicates the saturation of red blood cells with hemoglobin.
An increase in the color index is a sign of hypovitaminosis B12, or folic acid deficiency.
A decrease in color index indicates iron deficiency or lead salt poisoning.
A reduced color index may indicate the development of renal failure.
Erythrocyte sedimentation rate
After settling, the plasma is separated from the red blood cell mass
Erythrocyte sedimentation rate is a natural process that occurs if the blood being tested is left in a glass capillary without the ability to clot.
There are two ways to determine the erythrocyte sedimentation rate:
- Westergren method - blood for analysis is taken from a vein and settled in a capillary tube with 200 divisions. The method is highly accurate.
- Panchenkov method - a capillary with 100 divisions is used to determine ESR. Blood for research is taken from a finger; a smaller amount is required.
Blood taken for analysis is diluted with an anticoagulant in a ratio of 1:4 and settled in a graduated capillary. Red blood cells, under the influence of gravity, settle to the bottom, plasma remains at the top. The doctor takes measurements on a capillary scale to determine the ESR.
Under the influence of pathology, red blood cells stick together into complexes, and their sedimentation rate increases.
When ESR increases, it is necessary to look for the source of the inflammatory process.
If the erythrocyte sedimentation rate is reduced, disturbances in water-salt metabolism in the body may occur. The rate also changes under the influence of hormonal changes during puberty.
Reticulocytes
Reticulocytes are immature red blood cells that are formed in the bone marrow and mature in the bloodstream. The intensity of reticulocyte formation allows for differential diagnosis of anemia and identification of the source of pathology.
Reticulocytes increase sharply in the following diseases:
- Hemolytic anemia.
- Acute oxygen starvation.
- Deficiency of B vitamins.
- Presence of cancer metastases in the bone marrow.
When treating anemia, a high percentage of reticulocytes is considered a signal that the patient has begun to recover.
The decrease in quantity occurs under the influence of the following factors:
- Kidney diseases, including bacterial ones.
- Lack of iron in the diet.
- Autoimmune conflict.
- Decreased activity of the thyroid gland.
- Lack of iodine and trace elements.
- Bone cancer.
In combination with other indicators, the number of reticulocytes allows us to draw up a clinical picture of the disease.
In newborns, reticulocytes in the blood are increased, as there is an active process of maturation of the red blood cell mass.
Platelets
The structure of a blood platelet
Platelets are small, flat, colorless cells that contain special proteins. Platelets are responsible for regenerative processes and prevent blood loss as a result of mechanical damage to blood vessels.
Changes in the number of platelets in the blood are associated with changes in blood viscosity.
The platelet count increases with dehydration, physical fatigue, and inflammatory processes. The platelet count increases after surgery.
A reduced cell count may indicate one of the following pathologies:
- Hemophilia is a congenital genetic disease characterized by decreased blood clotting.
- Chronic infections.
- Lupus erythematosus.
- Allergic reactions.
- Viral infections such as rubella or chickenpox.
- Compensated or uncompensated heart failure.
There is a decrease in platelet mass after blood transfusion. If the mother develops an allergy in the period before childbirth, the child's platelet count will be reduced in the first days of life.
Thrombocrit
Thrombocrit is the relative volume of platelet mass in relation to blood plasma. An indicator is determined to determine the risk of developing blood clots or internal bleeding.
The indicator increases slightly with overwork, lack of fluid in the body or after physical stress.
Thrombocrit changes significantly in the following cases:
- Pathologies of the spleen;
- In case of iron metabolism disorders;
- With thyroid dysfunction;
- In case of development of diabetes mellitus;
- In inflammatory reactions provoked by viruses and bacteria.
A decrease in thrombocrit may be a sign of one of the diseases:
- Viral infections;
- Hereditary diseases of the hematopoietic organs;
- Aplastic anemia;
- Liver pathologies;
- Intoxication;
- Exposure to chemicals or ionizing radiation.
In girls, thrombocrit changes during puberty, during ovulation and the menstrual period.
Lymphocytes
Lymphocytes are a group of immune cells without inclusions; cells exist for up to several years. Cells differentiate during maturation, each group performing a specific function.
T-lymocytes, the most numerous group, undergo two stages of formation: in the bone marrow and in the thymus gland. Children have a higher number of T-lymphocytes in their blood compared to adults. There are several subgroups:
- Killer T cells are the main group of T lymphocytes that attack cells damaged by foreign agents.
- T-helpers - perform a coordinating function and regulate the intensity of the immune response.
- T-receptors - recognize foreign proteins and nucleic acids, signaling the onset of infection.
- T-suppressors – suppress the immune response, reduce the intensity of the process.
In addition to T-lymphocytes, the body contains B-lymphocytes. These cells read information about foreign proteins and regulate the production of specific antibodies. B lymphocytes regulate humoral immunity.
NK cells are a type of killer T cells with great potential. They attack the body’s own cells that are susceptible to cancerous degeneration or infected with a virus. They carry a complex of toxins that destroy cell membranes and organelles.
Changes in the number of lymphocyte cells may indicate serious health problems. If the number of lymphocytes decreases, one of the pathologies can be suspected:
- Tuberculosis.
- Lupus erythematosus.
- Acquired immunodeficiency syndrome.
- Long-term use of drugs that suppress the immune system.
- A course of radiation or chemotherapy.
- Development of renal failure.
If there are more lymphocytes in the blood than normal, the study may reveal the following diagnosis:
- Viral infections, including acute respiratory diseases.
- Diseases of the blood and hematopoietic organs.
- Severe poisoning.
- Use of immunostimulating drugs.
In a newborn child, in the first days of life, there is a sharp increase in the number of leukocytes, since after entering the external environment, the body adapts to new conditions and protects itself from viruses that have entered the body.
Monocytes
Monocytes are immature forms of leukocytes, the largest of the white blood cells. They live in the blood for several days, then migrate to tissues, where they transform into macrophages - cells that absorb foreign inclusions and dead particles of the body’s own cells.
The number of monocytes may increase slightly and extremely. A sharp increase in the number of monocytes is called absolute monocytosis.
Monocytosis is observed in the following cases:
- With an intense viral attack, blood damage by fungi and their spores, protozoan parasitic microorganisms.
- When the body is affected by helminths.
- In case of development of an autoimmune conflict.
- If bone marrow diseases are observed: acute leukemia, mononucleosis, lymogranulomatosis.
- When cancer metastases grow into the bone marrow.
- Tuberculosis of the lungs or bone tissue.
- Inflammation of the membranes of the heart.
- Rheumatoid arthritis.
- Poisoning with phosphates or chlorine esters.
- Exacerbation of peptic ulcer of the stomach and duodenum.
A relative increase in monocytes in the analysis occurs during burns, injuries, surgical and dental operations. This condition is not dangerous for the patient and goes away on its own within a few days after the intervention.
The leukocyte formula shows a normal ratio of granulocytes and lymphocytes with a normal general blood test in a child.
Blood for determining the leukocyte formula is taken from a vein. Four hours before the procedure, you should not eat or experience nervous or physical stress.
When calculating the leukocyte formula, not only the number of cells plays a role, but also the degree of their maturation. If young forms of leukocytes predominate, the formula shifts to the left, which indicates serious pathologies.
A shift in the leukocyte formula to the left can be provoked by the following pathologies:
- Necrotic processes.
- Poisoning from food toxins or gaseous toxic compounds.
- Taking hormonal drugs.
- Cancerous degeneration of bone marrow cells.
A shift in the leukocyte formula to the right implies a predominance of mature forms in the absence of young cells. The process may not indicate a lack of vitamin B12. The number of mature forms of immune cells changes with the development of renal or liver failure. The leukocyte formula shifts after blood transfusion and surgery.
Plasma cells
Plasma cells are the precursors of lymphocytes and are not detected in the analysis. When plasma cells appear, the doctor can make one of the following diagnoses:
- Rubella, measles, chicken pox.
- ARVI, influenza of various groups.
- Sepsis.
- Purulent infections caused by streptococci or staphylococci.
- Other types of infections of a bacterial, fungal and viral nature.
- Oncological diseases.
- Radiation sickness.
- Immune disorders.
- Mononucleosis.
Blood sugar test
The blood contains sugar (sucrose), and glucose, a breakdown product of sugar when it enters a medium containing water and a special enzyme - amylase. Glucose easily dissolves in water and is transported in the blood to all cells of the body. Brain and muscle cells need glucose more than others.
The hormones glucagon and insulin are responsible for the amount of glucose With a lack of these hormones, sharp fluctuations in glucose are possible, which pose a danger to the child’s life.
Recently, type I diabetes mellitus is increasingly being discovered in children, which is associated with congenital characteristics that cause the immune system to attack the cells that produce insulin.
When the amount of insulin drops, the concentration of glucose increases sharply, and its excess is no less dangerous than its deficiency.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
A sugar test allows you to identify the first signs of diabetes and start treatment in a timely manner, which can save a child’s life.
At the same time, it is very important to follow all the rules for taking the analysis, because otherwise it will give an incorrect result. These are the rules:
- Do not feed the baby 8-12 hours in advance (otherwise the sugar level will be too high);
- Do not brush your teeth (for the same reason, because toothpastes contain sucrose or glucose);
- You can only drink plain boiled water.
The analysis is done in the morning using a finger prick. Modern glucometers allow you to get results immediately after taking blood, without waiting, as with other tests.
How is blood taken from children for OBC?
Blood for a general blood test is taken from the small external vessels of the fingers. The blood test of a newborn is characterized not only by a different norm, but also by the blood sample itself, which is taken from the heel, or less often, from the baby’s toe. The area is wiped with an alcohol swab, then with a quick movement the laboratory assistant makes an incision and, pressing on the finger, draws blood.
In newborn babies, blood for general analysis is taken from the heel
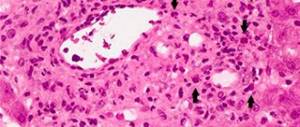
After collection, the laboratory assistant drips the material for research onto the glass and rubs it with another piece of glass. A special dye is added to the smear, after which the number of blood cells is counted under a microscope and other indicators are assessed.
Which children are at risk for diabetes?
There are categories of children who are more vulnerable to diabetes than others. If your child falls into this category, he may need to be tested for sugar more often than others.
Since type I diabetes is inherited , the risk group includes those in whose family there were already patients with this disease. The risk is especially high if your ancestors were sick on both the maternal and paternal lines.
There is also a high risk of getting the disease among residents of islands and remote small settlements due to the fact that inbreeding is more common in a limited population. It is no coincidence that the mountainous countries of Europe (Austria, Switzerland, Sweden or island residents) lead in the number of hereditary diseases.
Obese children are also at risk. Therefore, it is advisable for the child to move more and eat less sweet and fatty foods. And if the child is already overweight, it is better to contact a pediatrician .
Poor diet and lack of physical activity most contribute to the development of both types of diabetes.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
You also need to be careful with cow's milk. Some parents believe that milk is good for all children, but the proteins it contains inhibit the pancreatic cells that produce the hormone insulin.