What is uterine fibroid?
This is a benign tumor consisting of smooth muscle cells that form the wall of the uterus. Tumors of the fibroid type are the most common. They can occur on various organs of the female reproductive system: ovaries, uterus, mammary glands, skin. The tumor grows slowly and asymptomatically. In size it can reach 30-40 cm in diameter. This neoplasm almost never becomes malignant.
How to treat
Based on the results of the examination, the doctor makes a decision on the necessary method of treatment, the appropriateness of which is determined by the type and nature of the tumor, as well as the stage of its development.
The woman’s desire to have a child in the future remains important in this matter, so the choice is always towards organ-preserving manipulations. The treatment process can use a surgical method or use conservative treatment.
Surgery
Surgical operations do not aim to completely remove the uterus; doctors always strive to preserve intact the reproductive organs that are able to function. Most often, myomectomy is used for this, when only one tumor must be removed. However, there remains a risk of relapse, therefore, if otherwise is not possible, partial removal of the uterus along with the tumor can be used. Patients may be offered a new method in the form of arterial embolization, which uses an artificially created obstacle to allow blood to flow into the formed tumor. As a result, the reverse process of its development occurs.
A completely new treatment method is evaporation of the node using FUS ablation, which does not involve incisions and allows you to eliminate it bloodlessly using ultrasound.
Conservative treatment
Conservative therapeutic methods include the use of hormonal medications. The choice of these remedies is entrusted to specialists who take into account the nature of the tumor, the age of the patient, the magnitude of the hormonal imbalance, the presence of chronic diseases and much more.
Often, hormonal drugs in the initial stages of the disease can completely eliminate existing disorders or stop further development of the tumor.
Hormone therapy
Hormonal therapy is usually carried out over a long period of time, at least six months. The purpose of this method is to eliminate the grounds for surgery. Such treatment can use the following groups of drugs:
- progestin agents;
- progestational with the inclusion of estrogens;
- atigonadotropic drugs;
- androgen-containing drugs.
The use of hormonal drugs for the treatment of various types of fibroids makes sense in the initial stages of development of the tumor process, the duration of which is no more than twelve weeks.
Folk remedies
Traditional methods of treatment serve as an effective complement to complex methods of treating fibroids. They are selected taking into account individual indications, use only natural ingredients and have virtually no contraindications. With the help of these means it is possible to restore the internal defenses of the body, with the help of which it is able to eliminate pathological disorders with great success.
It should be borne in mind that the use of folk remedies is more appropriate when the tumor processes are asymptomatic and the size of the fibroids is small.
Causes of occurrence and development of fibroma.
The exact causes of the pathology have not been established for certain. Most often, this disease is inherited, and mainly in women of African descent. The tumor grows and develops when a woman is very sensitive to fluctuations in female sex hormones in her body - estrogens. That is why the disease practically does not occur in girls before puberty and tends to fade after the onset of menopause. But even the presence of these indicators does not always contribute to the development of a tumor.
Uterine fibroids can be triggered by late onset of menarche, frequent abortions, taking estrogen-containing oral contraceptives, the presence of other diseases of the female reproductive system, as well as lack of regular sex life.
If you suffer from excess body weight, diabetes, thyroid disease, or hypertension, this may cause the development of a tumor. In addition, frequent stress is a good background for the development of fibroids.
The existing tumor tends to grow during pregnancy, this is due to the fact that the synthesis of hormones increases. After childbirth, most often, the neoplasm returns to its previous size. As mentioned above, in the post-climactic period, the level of the hormone estrogen in the female body decreases, and at the same time, the size of uterine fibroids decreases, until it completely disappears.
Fibroma during pregnancy
Many young women suffering from uterine tumors are concerned about the question: will they be able to give birth to a healthy baby?
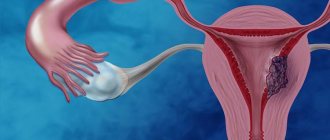
In general, a small fibroid does not prevent either the onset of pregnancy or its successful completion. The exception is large fibromatous nodes and neoplasms located in the area where the fallopian tubes originate, when the entrance to them is closed by a tumor, which interferes with fertilization and the movement of the egg to the endometrium. Large fibroids pose a danger to the normal development of the fetus, as they can disrupt its normal position in the uterus, provoke miscarriages and premature birth. Cervical tumor localization is the most dangerous due to the risk of complicated labor and massive bleeding. All pregnant women diagnosed with fibroma should be under the supervision of specialists, and in case of dangerous forms of the tumor, it is better to get rid of it before pregnancy or childbirth, if possible.
Symptoms of pathology.
In 95% of cases, a fibroid tumor appears and grows asymptomatically. And only the remaining 15% have a clinical picture, accompanied by heavy and prolonged menstruation. The presence or absence of symptoms of the disease depends on where the uterine fibroid is located. If the fibroid nodes occupy an unfortunate location relative to other pelvic organs, then menstruation will take the form of menorrhagia (heavy and prolonged bleeding).
In this case, the woman experiences severe abdominal pain, accompanied by cramps and the release of blood clots. There is also pain in the lower back and perineum, caused by compression of the nerves that go to the lower extremities.
Uterine fibroids put pressure on the bladder and rectum, resulting in a woman suffering from frequent urination and constipation. Sexual life is accompanied by painful sensations.
Treatment
Gonadotropin-containing hormone (GnRH) is used to relieve the symptom of pain.
Myomectomy (to preserve fertility) or hysterectomy for symptomatic fibroid tumors is indicated.
Asymptomatic fibroid tumors do not require treatment. A woman should be examined periodically (every 6–12 months) by a gynecologist.
For symptomatic fibroids, treatment options include ovarian hormone suppression to control bleeding. Opportunities are suboptimal and limited. Physicians should consider medical clinical treatment and discuss other options before performing surgery. Agonists (GnRH) are sometimes given before surgery to shrink fibrous tissue. These drugs often stop menstruation and allow blood counts to increase. In the perimenopausal period, it is permissible to wait, because the mature growth decreases in size after menopause or may disappear.
Drugs for fibrous tumors
A number of drugs are used to relieve symptoms, reduce fibrous growth, or both:
- agonists (GnRH);
- exogenous progestins;
- antiprogestins;
- selective estrogen receptor modulators (SERMs);
- danazol.
Agonists (GnRH) are often the drugs of choice. For large fibroids, they can reduce fibrous size and bleeding.
These drugs can reduce estrogen production. Agonists (GnRH) are most useful if given preoperatively to reduce fibrous and uterine volume, making surgery technically more feasible and reducing blood loss. In general, the drugs mentioned should not be used long term. Increased recovery to pretreatment size within 6 months is common, and bone demineralization is possible. To prevent long-term use of the drugs, doctors must give patients extra estrogen.
Exogenous progestins may partially inhibit estrogen stimulation of uterine fibrous growth. Progestins may reduce uterine bleeding but may not reduce fibroids as well as agonists (GnRH). These medications may be taken every day (continuous therapy). Such therapy often reduces bleeding and provides contraception.
Intrauterine device with hormones
Progestin therapy causes the muscle layer to grow in some women's uteruses. A levonorgestrel-releasing intrauterine device (IUD) may be used to reduce uterine bleeding.
Danazol is an androgen agonist that can suppress fibrotic growth in the early stages, but has a high rate of adverse effects (weight gain, acne, swelling, hair loss, flushing, vaginal dryness), so it is less commonly taken.
Surgery for fibroid tumors
Surgery is usually used for women in the following cases:
- Rapidly growing tumor-like formation of the small pelvis.
- Recurrent uterine bleeding, unresponsive to drug treatment.
- Severe or constant pain or pressure under the skin (requires opioids for control or is intolerable to the patient).
- A large uterus that has a mass effect in the abdominal cavity, causing urinary bowel symptoms or compressing other organs, causing dysfunction (eg, hydronephrosis).
- Infertility (if pregnancy is desired).
- Recurrent spontaneous abortions (if pregnancy is desired).
- Dimensions for mimoma removal surgery.
- Other factors favoring surgery are the completion of the birth of the child and the expressed desire of the patient to choose the exact treatment.
Myomectomy is done laparoscopically or without automated methods.
A hysterectomy can also be done laparoscopically, vaginally, or by laparotomy (an incision in the abdomen).
Most indications for myomectomy and hysterectomy are similar. Patient choice is important, but people should be well informed about the expected difficulties and complications of myomectomy versus hysterectomy.
Scheme of surgery on the uterus
Removal in sections is done during a myomectomy or hysterectomy. Remove in parts, including cutting fibrous tumors or intrauterine tissue into small parts so that they can be removed through a smaller incision (for example, laparoscopically). It is extremely rare for women undergoing surgery for uterine fibroid tumors to have an unsuspected, undiagnosed sarcoma or other uterine cancer. If removal is done piecemeal, malignant cells may be disseminated into the peritoneum. Patients should be advised that if piecemeal removal is used, there is a small risk of dissemination of cancer cells.
If women desire pregnancy or want to keep the uterus, myomectomy is used. In approximately 60% of women with infertility due to fibroid tumors, myomectomy restores fertility and it is possible to become pregnant after approximately 14 months. However, hysterectomy is often necessary or preferred by the patient.
This is a more precise treatment. After a myomectomy, new fibroids sometimes begin to grow again, and approximately 25% of women with myomectomies have a hysterectomy approximately 4-8 years later.
Patients have other pathologies that make surgery more complicated (extensive adhesions, endometriosis).
Hysterectomy reduces the risk of other problems. This includes cervical intraepithelial neoplasia and others.
New procedures may relieve symptoms, but the duration of symptom relief and the effectiveness of the procedures in restoring fertility have not been assessed.
- High intensity focused echography.
- Cryotherapy.
- Radiofrequency amputation.
- Magnetic resonance guided focused ultrasound surgery.
- Detection on x-ray.
- Uterine artery embolization.
Uterine artery embolization tends to cause infarct formation of fibroid tumors throughout the uterus while sparing normal uterine tissue. Women recover more quickly after the procedure than after a hysterectomy or myomectomy, but complication rates and return visits tend to be higher. The treatment failure rate is 20-23%; in such cases, treatment with hysterectomy is required.
Choice of treatment
To treat fibroma, factors are taken into account:
- Asymptomatic fibrous tumors: no treatment required.
- Women after menopause: trial of expectant management, after menopause, fibroids become smaller.
- Symptomatic fibroids provided that pregnancy is desired: uterine artery embolization, another new method (high intensity focused echography) or myomectomy.
- Severe symptoms when other treatment has failed, especially if the pregnancy is unwanted: hysterectomy, possibly preceded by drug treatment (with GnRH agonists).
Treatment of uterine fibroids with folk remedies
Treatment of uterine fibroids with folk remedies is a fairly popular treatment method aimed at eliminating unpleasant symptoms, as well as reducing bleeding.
For treatment, exclusively natural plant components are used, for example, calendula, which is brewed and taken orally.
Other remedies include blue iodine with milk, walnuts, and flaxseeds. But before self-medicating, you need to consult a doctor.
Calendula (2 tablespoons) is poured into an empty bottle, left in the dark for two weeks, shaken daily. Juice gradually appears. After the expiration date, filter the resulting mixture. Drink 1 tbsp. spoon 3 times a day.
Homeopathy helps to get rid of symptoms and tumors so as not to undergo hormonal treatment. This restores balance in the central nervous system. The concentration of estrogen decreases. The preparations are selected by a qualified homeopath. But this does not always achieve a certain effect.
Diagnosis of the disease.
If you have any of the above symptoms, you should consult a doctor immediately. Only an experienced specialist will be able to identify the disease in time and prescribe competent treatment. If during an examination the gynecologist reveals an enlarged uterus with a bumpy and dense surface, this may be a signal of the presence of a fibroid tumor. During the initial examination, it is impossible to make an accurate diagnosis and distinguish fibroma from sarcoma or fibroids, so the doctor must prescribe an additional examination:
- Ultrasound examination of the pelvic organs;
- Carrying out hysterosalpingography and hysteroscopy;
- Computed tomography and magnetic resonance imaging will allow definitive confirmation of the disease;
- In controversial cases, the doctor may additionally prescribe diagnostic laparoscopy;
These procedures are needed to confirm or refute the diagnosis, as well as to exclude other more serious gynecological diseases.
Causes
Most often, cervical fibroids in young women can develop due to excessive production of estrogen by the ovaries. This hormone is produced especially strongly in pregnant women at twenty weeks. Causes also include an increase in estrogen from taking medications during menopause, as well as birth control pills.
Sometimes the development of the disease occurs due to:
- complicated traumatic childbirth;
- caesarean section;
- frequent abortions;
- periodic diagnostic curettage;
- ingrowth of the intrauterine device;
- gynecological diseases of chronic course.
The growth process and the emergence itself are provoked by the following factors:
- Late onset of menstruation in girls.
- Irregular or absent sex life.
- Delayed first birth (after twenty-five years).
- Frequent sex during menstruation.
We recommend reading Purulent atheroma - treatment, causes, removal
The tumor can develop against the background of obesity, diabetes, physical inactivity (muscle weakening due to a sedentary lifestyle), sexually transmitted infections, and constant stress. In almost forty percent of cases, the patient’s relatives had uterine fibroids, so heredity plays an important role here.
Types of benign fibroid tumors.
Uterine fibroid is a nodular formation. Depending on their number, single and multiple fibromas are distinguished. The uterus has a three-layer structure. The outer layer is called perimetrium. The thickest layer is the second layer, called the myometrium (smooth muscle). And finally, the inner layer is the endometrium. It is represented by the mucous membrane. Depending on where the tumor is located, there are:
- Intramural fibroma (formed on the muscle wall);
- Submucosal fibroma (forms under the endometrium and grows inward);
- Subserous fibroma (this type of tumor grows externally on the perimeter);
In addition, there are:
- The stalked form of fibroma (this is a type of tumor in which a stalk appears);
- Interligamentous fibroma (located between the leaves of the broad uterine ligament);
- Parasitic fibroma (extremely rare and caused by appearance on neighboring organs);
Classification
Benign uterine neoplasms are systematized according to the following principle:
- According to the predominance of connective tissue and muscle components of the tumor:
- myoma;
- fibroids.
- According to the severity of proliferation processes:
- simple fibroids/myoma – grows slowly, there are no cell proliferation processes;
- proliferating fibromyoma/myoma – grows quickly, myometrial cell activity is increased, atypical cells are absent;
- presarcoma – characterized by multiple elements with signs of atypia.
- According to the location of tumor nodes:
- interstitial or intramural myoma/fibromyoma - nodes are located in the thickness of the myometrium;
- subserous myoma/fibromyoma – the neoplasm grows under the serous (outer) lining of the uterus, that is, into the pelvic cavity;
- submucosal or submucosal myoma/fibromyoma – the tumor grows under the endometrium, into the uterine cavity, which leads to its deformation;
- intraligamentary or interligamentous myoma/fibromyoma - the neoplasm is located in the leaves of the broad ligament of the uterus and grows in the parametrium.
- By growth pattern:
- diffuse growth - uniform germination of the muscular layer of the uterus;
- nodular growth - individual nodes form in the thickness of the myometrium.
Prognosis and prevention of the disease.
First of all, it is necessary to exclude provoking factors. Avoiding excess weight after 18 years of age, quitting smoking and a healthy lifestyle are components that will help avoid pathology. Regularly visiting a gynecologist and undergoing an ultrasound examination is an effective way to prevent uterine fibroids.
If you are faced with this pathology, do not despair! Regular observation by a gynecologist will help maintain the disease at a stage that does not interfere with the normal functioning of the reproductive system.
Myoma and fibromyoma
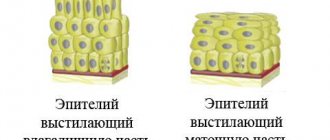
Since the uterus contains not only smooth muscles, but also connective tissue, it is customary to distinguish fibroids from myomas. However, in reality, many specialists, to understand patients, combine the concepts of fibroma, myoma and fibromyoma into a single whole. In the tissue layers of the uterus, if stromal cells predominate in the tumor process, and smooth muscle fibers are in the minority, they speak of fibromyoma of the uterine body. If the predominance of myometrial cells is pronounced, and there is very little connective tissue, the doctor has the right to diagnose myofibroma. When only connective tissue structures are found in a tumor, it is called fibroma.
What is common in the characteristics of these neoplasms is that any benign process in the uterus involves a large number of blood vessels, proliferating tissues and maintains characteristic symptoms. A thorough cytological examination revealed that there are still more of them in fibroids. A tumor consisting exclusively of smooth muscle cells is softer to the touch.