Pancreas:
- Takes part in the production of enzymes that are components of digestive juice.
- Participates in metabolism.
During various diseases of the gland, there is a failure in the digestion of food, the breakdown and absorption of elements necessary for the body. Based on the claims, the specialist diagnoses disorders of this organ, but to clarify the diagnosis it is necessary to be examined.
Can your pancreas hurt?
Inflammatory processes of the pancreas in women and men manifest themselves with differences, but insignificant. At first, the disease makes itself felt to the same extent.
The difficulty is that women attribute the signs of the disease to gynecology . Start taking pills to cure diseases of the genitourinary system. When pancreatitis provokes nervous disorders, the heart and central nervous system are treated, believing that these are diseases of the cardiovascular system.
The pain is localized depending on the location of the inflammatory processes of the gland:
- It may also appear on the right side of the abdomen;
- There is pain in the right shoulder, chest and kidney areas.
- Inflammation is often confused with heart disease.
Therefore, when sudden pain occurs, you need to consult a specialist for an accurate diagnosis and prescribe therapy.
Pain may be accompanied by:
- Nausea;
- Vomit;
- Diarrhea;
- Constipation;
- Bloating.
After vomiting, the patient does not feel better:
- Tachycardia increases;
- Blood pressure decreases.
- In some situations, the attack is accompanied by yellowing of the skin and the appearance of dark spots near the lower back and navel.
- Patients complain of poor health, weakness, and lethargy.
- They are tormented by severe sweating, high fever, and their skin turns pale.
What to do if you suspect pancreatitis
Any regular abdominal pain, especially if it is accompanied by other symptoms (nausea, indigestion) is a reason to go to a therapist or gastroenterologist. This is important for a number of reasons.
Firstly, it may not be pancreatitis at all. Only a specialist will find out what exactly hurts in the stomach after an examination. And the options are multifaceted - from dyspepsia, irritable bowel syndrome or gastritis to developing cancer.
Secondly, if we are talking about pancreatitis, under no circumstances should it be neglected. Even if the abdominal pain appears only occasionally and seems minor. Without treatment, pancreatitis may develop. Symptoms and Causes provoke other conditions, sometimes very serious and even deadly.
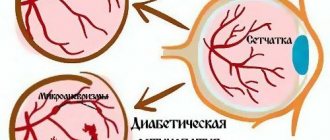
- Diabetes. In a pancreas damaged by inflammation, insulin production is disrupted, which becomes a trigger for the development of diabetes.
- Pseudocysts. Due to acute pancreatitis, fluid may accumulate in one or more alveoli of the pancreas (in this case, they speak of the formation of a cyst-like “pocket”). Rupture of a large pseudocyst can lead to internal bleeding and cause peritonitis.
- Kidney failure. Acute pancreatitis can lead to inflammation and severe kidney damage.
- Breathing problems. Due to the fact that the pancreas is also responsible for the production of certain hormones, damage to it can cause changes in the body that will affect the functioning of the lungs.
- Pancreas cancer.
Symptoms of a diseased pancreas: how to understand what exactly hurts?
We wrote about the symptoms of pancreatic disease here.
The main symptoms indicating the disease:
- Pain.
- Dyspepsia (disruption of normal stomach activity, difficult and painful digestion).
To eliminate pain, it is necessary to identify where the pancreas hurts:
- Unpleasant sensations are concentrated in the epigastric region, they tend to move to the left hypochondrium, left shoulder blade, and lower back.
- They arise or intensify after overeating, excessive consumption of fatty, spicy or fried foods, and alcoholic beverages.
- Local cold makes it possible to relieve pain; it happens that the patient, in order to reduce the pain, takes a forced position (lying on his side with his knees pressed to his stomach or sitting, bending forward).
Causes of inflammation
Various factors lead to the appearance of acute pancreatitis.
The reasons that provoke the appearance of inflammatory processes include:
- Disruptions in the digestive processes. In such situations, pancreatic disease occurs due to increased concentration of fat in the blood. Such deviations lead to the fact that the gland produces more enzymes that break down fats than necessary. After such functioning in the gland, there is a high probability of acute pancreatitis, which is accompanied by acute pain.
- Bad habits. Smoking and alcoholism stimulate the gland to produce pancreatic juice and destroy tissue. In addition to the above, they provoke disruptions in the blood supply to tissues, which leads to a lack of oxygen and catalyze the development of inflammation.
- Diseases of the liver and gall bladder. With various ailments of such organs, the digestive processes go wrong. Bile penetrates the ducts of the gland and its enzymes begin to function close to the tissues, provoking inflammatory processes.
- Medications. Some medications cause the production of digestive enzymes, increasing the risk of diseases of this organ.
- Malfunctions in the immune system. Inflammation, which is caused by weakened immunity, when healthy cells are attacked, the cells of the pancreas are affected.
- Changes with age.
How to prevent pancreatitis
This is what doctors recommend Treatment for Pancreatitis to prevent pancreatic diseases.
- Limit your alcohol intake.
- Try to quit smoking.
- Maintain a healthy weight.
- Eat a balanced diet: less sugar (including sugary drinks), more high-fiber foods. This diet will reduce the risk of developing gallstones, which are one of the main causes of acute pancreatitis.
What happens in the pancreas during an attack of pain?
The pancreas produces inactive enzyme precursors, which turn into an active form, and this process takes place inside the duodenum, where they pass through the glandular duct and the common bile duct.
Various factors influence it, thereby increasing the pressure inside the gland, disrupting the outflow of its secretions, and early activation of enzymes begins to occur. As a result, instead of digesting food, they digest the organ itself. Acute inflammatory processes develop.
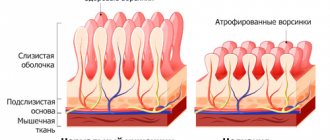
In the process of chronic pancreatitis, normal gland tissue is eventually replaced by scar tissue, and insufficiency of the exocrine and endocrine functions of the organ appears.
Responsibilities of the pancreas
Many people wonder what functions the pancreas gland performs in the body and its role in the human body. We will try to answer this question briefly and clearly.
The role of the pancreas in the human body is very serious and significant. By eating food, our body receives useful and necessary minerals and vitamins.
However, when eating food, beneficial substances are in a complex compound form, to obtain which they need to be completely broken down into the necessary microelements.
For these purposes, the pancreas produces digestive juice, which is delivered through a channel in the organ to the duodenum.
In this intestine, products are broken down into a simple state, which facilitates rapid absorption.
In the scientific community, this condition is called exocrine function. There is also another function - endocrine, in which the synthesis of two hormones insulin and glucagon occurs.
Insulin is responsible for the amount of glucose in the bloodstream. By directing glucose to tissues and organs, the human body ensures good functioning of muscle and fat tissue.
At this moment, insulin turns on and stops the strong increase in glucose in the human life-support organs.
Glucagon also works in tandem with insulin, but is its opposite. It is created to increase glucose in the body and blood plasma, and forms reserves in the human liver organ.
In addition, these two hormones also maintain the amount of potassium and sodium in the blood. This is the role the pancreas plays in digestion.
The role of the pancreas in the human body is simply colossal. In addition to hormones, it produces enzymes, which facilitates the processing of food.
The main enzymes produced by the gland are:
- Amylase. This enzyme reduces the chain of carbohydrates, which, after processing, must break down into sugar molecules. After all, this is the only way they will be absorbed in the intestines of the human body.
- Lipase. This enzyme breaks down fats into glycerol and fatty acids. Only in this state are they able to be absorbed into the human body and complete the process of food digestion correctly. Lipase helps the body absorb vitamins A, D, E, K, which are a type of fat solvent.
- Nuclease. This enzyme releases nucleic acid and uses it at the genetic level to develop its own structures.
- Trypsinogen. This enzyme is not directly involved in the digestive chain, but serves to generate another enzyme needed by the body, which creates the dissolution of protein into molecules.
- Prophospholipase. This enzyme acts on the constituents of complex fats, like phospholipids.
Therefore, answering the question what function does the pancreas perform, we can safely say that it is the most important one in the human digestive system.
It is worth understanding that the importance of the pancreas for the body is indisputable, but there are certain moments in which pathological changes in the functioning of this organ create failures and problems, causing serious diseases throughout the body.
How does pain manifest itself?
To answer the question of how the pancreas hurts, we need to talk about the pathology:
- The main symptom of acute pancreatitis is severe pain in the upper abdomen. They cannot be removed with antispasmodics and analgesics. There is often vomiting, abnormal bowel movements, and lethargy. The main signs of pancreatitis on ultrasound of the pancreas are a change in shape and irregular contours, the appearance of a cyst.
- The disease develops in a complex manner. There is a high probability of death.
- Pain is the most worrying sign of chronic pancreatitis. The pain is localized in the epigastric region, moving to the hypochondrium and hitting the back. It can be shingles, it can get worse if you lie on your back, and become weaker when the patient sits down and bends over a little. They may appear or intensify 50-60 minutes after eating.
- Another unpleasant sign of the disease is diarrhea . The stool will become loose and may contain particles of undigested food. The amount of feces will increase significantly. Belching, nausea, gag reflex, and flatulence appear. There is a loss of appetite and rapid weight loss.
Read more about how to check your pancreas here.
Where does the pancreas hurt in a person? Symptoms:
- With this disease, the gland becomes inflamed, nausea occurs, and often vomiting. Vomiting does not bring relief or relieve symptoms.
- But the most unpleasant thing is pain in the abdomen (upper part) with a transition to the back area. It lasts for several days – it’s painful. Back pain intensifies.
- The pain is severe and debilitating.
- Gradually, the sick person tries to eat less, fearing pain. Losing weight.
- Weight loss also consists of the inability of a diseased pancreas to digest food. The production of enzymes is disrupted.
- Gives diarrhea.
- The heart beats quickly (tachycardia). The psychological state of the patient, loss of fluid during vomiting, and symptoms of intoxication, if this is after a “binge,” are also important.
- You develop a fever, shakes, and chills (infections are possible).
- The stomach seems to be swollen.
- The person is irritated, weak, and has difficulty concentrating on the problem.
- Headache.
- A sudden drop in pressure can cause shock.
Complications of pancreatitis
- Often pancreatitis is followed by cholecystitis, and, conversely, the latter provokes pancreatitis.
- It happens that during acute pancreatitis a virus gets attached. Cellulitis or abscess of the pancreas occurs. In certain situations, intra-abdominal bleeding begins.
- The second serious complication is the destruction of this organ and the appearance of peritonitis.
- In the future, the disease may become chronic. The process of exacerbation of pancreatitis is caused by irritating foods and alcoholic drinks. It may also be a consequence of diabetes mellitus.
Types of pancreatitis:
- Acute pancreatitis.
- Chronic pancreatitis.
The functions of the pancreas are fully restored during the acute form of the disease. The chronic form will eventually destroy the cells of the organ and lead to the appearance of other diseases.
If inflammatory processes affect the tissue whose cells produce insulin, patients who suffer from this disease develop second-degree diabetes.
Treatment of pancreatitis
Most acute cases of pancreatitis are treated in the hospital. The goal of treatment is to relieve symptoms and support pancreatic function so that it can recover from inflammation.
If the inflammation is caused by an infection, antibiotics . They help prevent or treat infection in the pancreas and surrounding tissues.
Treatment for chronic pancreatitis involves painkillers and diet changes . Some patients may require oral pancreatic enzymes in pill form to help digest food, while others may require insulin.
If you think you have acute pancreatitis, do not eat or drink anything until you see your doctor. Eating and drinking cause the release of enzymes from the pancreas. This will make the pain even worse.
The doctor will not allow you to eat or drink until you begin to feel better. Without forced fasting, in most cases nothing can be done to speed up healing. If the attack lasts for several days or a week, nutrition is administered to the patient intravenously.
If you have an attack of pancreatitis caused by gallstones , you may need an endoscopic examination. During this procedure, your doctor may make a tiny incision in the opening of the bile duct to treat a current or future blockage. Most likely, you will be advised to remove your gallbladder. This is usually done a few days or weeks after the attack of pancreatitis has passed.
Immediate surgery is technically more difficult and may worsen pancreatitis.
In rare cases, surgery may be required to drain a pseudocyst, debride an abscess, or stop bleeding.
Treatment for chronic pancreatitis aims to help control the condition and reduce any symptoms.
Changes in diet are necessary because chronic pancreatitis reduces the gland's ability to digest certain foods.
You will have to change your diet. A low-calorie, high-protein diet with fat-soluble vitamins and supplements is usually recommended. But don't make changes to your diet without consulting your doctor.
Pain management is an important part of the treatment of chronic pancreatitis. Painkillers are prescribed by the doctor depending on the intensity of the pain and the results of the examination.
If your pain is severe, you may be referred to a specialist such as a gastroenterologist or surgeon for further evaluation.
Symptoms of pancreatic dysfunction: pain in acute pancreatitis
The causes, manifestations, diagnosis and treatment of acute and chronic pancreatitis vary significantly.
During the acute form:
- Inside the gland, inflammation occurs rapidly. The enzymes contained in the juice are released into the blood and involve nearby tissues and distant organs.
- The main symptom of acute pancreatitis is considered to be severe girdling pain, which is concentrated in the epigastric region and, sometimes, in the hypochondrium.
- During the rapid development of inflammation, there is a risk of painful shock.
In addition, during an attack, the following are characteristic:
- Intoxication, which is expressed in the appearance of fever, tachycardia, a strong decrease in blood pressure and lethargy;
- Digestive problems, during which bloating, diarrhea or constipation, gag reflex, belching and dryness occur;
- The appearance of dark spots near the abdomen, coating on the tongue, etc.
The symptoms of acute pancreatitis develop rapidly according to the degree of death of gland cells that are affected by their own enzymes.
Read about how to treat diffuse changes in the pancreas here.
The nature of pain in pancreatitis
Inflammatory processes in the organ can be acute or chronic, which affects the severity of the main symptoms. Acute pancreatitis causes sudden, stabbing and piercing pain. As a rule, it is quite long and intensifies with sudden movements, coughing, sneezing and palpating the abdomen. In attempts to find a comfortable position to reduce the intensity of the pain syndrome, in a horizontal position on the back or on the side, the patient only gets worse. The only position in which the general condition can really improve slightly is sitting with a slight bend forward. The entire pancreas can become inflamed, or maybe only a separate part of it, so the pain is localized in different parts of the body:
- when the body or tail is inflamed, pain occurs in the left hypochondrium or in the center of the upper abdomen, in rare cases it radiates to the back;
- in the event of a pathological process in the head, pain is noted in the right hypochondrium or in the upper abdomen, in the center area;
- if the entire organ is inflamed, the pain is girdling in nature.
In fairly rare cases, pain due to pancreatitis may occur in the left side of the chest with a pronounced impact on the left shoulder blade, arm or lower jaw. In this case, it is important to correctly differentiate the diseases and exclude myocardial infarction. Other symptoms of acute pancreatitis include: fever, tachycardia, shortness of breath, cold sweat, yellowing of the sclera, yellow coating on the tongue, nausea and subsequent vomiting, constipation, diarrhea, the appearance of a blue-green color around the navel, lumbar region and groin. If such signs are detected, you should immediately seek emergency medical help. After all, the patient will get worse every minute.
The chronic form of pancreatitis is characterized by periodic exacerbations and remissions. With the next relapse, the patient experiences paroxysmal, cutting pain. Just as in the case of the acute form, an exacerbation leads to the patient being unable to carry out everyday activities. The situation gets worse when standing or lying down. Only sitting with a slight bend forward can you feel a little relief. A distinctive feature of chronic pancreatitis is that pain can occur not only in the upper abdomen and hypochondrium, but also deviate to the side:
- middle part of the abdomen;
- lower chest;
- the entire back area;
- small of the back.
As a rule, attacks of pain occur as a result of a diet disorder, after severe stress or alcohol intake. In this case, the patient suffers from intestinal upset, bloating, and possible weight loss. Depending on the degree of organ damage, the main symptoms can appear frequently and pronounced, or rarely and without much intensity. Untreated chronic pancreatitis leads to necrosis of pancreatic tissue and subsequently to diabetes mellitus.
Symptoms of chronic pancreatitis
The chronic form of pancreatitis is considered an inflammatory disease that lasts for years. Remissions are replaced by exacerbations, which are caused by various factors. During remission, symptoms do not appear.
When an exacerbation begins, the following occurs:
- Cutting or dull pain in the upper abdomen, which appears mainly after eating;
- Nausea and gag reflex followed by the inclusion of bile, broken stools, dryness that occurs after spicy and fatty foods;
- Feelings of heaviness and bloating when eating;
- The patient has yellowness of the skin and sclera. With chronic pancreatitis, symptoms become more and more pronounced.
Pancreas: pain from poor nutrition
What to do if your pancreas hurts as a result of poor nutrition?
Causes:
- Frequent consumption of fatty, spicy, fried foods.
In this regard, both a single attack of pain and acute pancreatitis are likely. Fatty foods are difficult to digest and can cause a disruption in the outflow of pancreatic juice and changes in its composition. This provokes pain and nausea.
To avoid problems with the pancreas:
- You need to regulate your diet
- Eliminate bad habits.
Read about what you can eat if you have pancreatitis.
What happens when the functions of the pancreas are impaired?
Pancreatic dysfunction is manifested by various symptoms of digestive disorders if its exocrine part is affected. If the endocrine part suffers, then symptoms of hyperglycemia develop, associated with excess sugar in the blood.
Article on the topic: Irrigography - why is it so important
Diseases resulting in enzyme deficiency
When consuming very fatty foods, alcohol abuse, overeating, concomitant gallstone disease or parasitic infestation, pancreatitis, that is, inflammation of the pancreas, can develop. Symptoms of this condition are pain in the upper abdomen or left hypochondrium, nausea, and vomiting. The stool changes its color and consistency, it takes on a “greasy” appearance. Appetite and physical activity decrease.
As a result of inflammation of the gland, the production of enzymes decreases, food is poorly digested, and the body lacks nutrients. In addition, the accumulation of salts in the body progresses, osteochondrosis, osteoarthritis, and vascular atherosclerosis appear.
Diseases associated with the destruction of islet cells
Against the background of chronic pathology of the pancreas, not only the production of enzymes may decrease, the islets of Langerhans are often affected, and the amount of insulin decreases. This condition is classified as type 2 diabetes mellitus. Treatment of this pathology includes treatment of chronic pancreatitis and taking glucose-lowering drugs in tablet form.
Another case is when, as a result of unspecified reasons, possibly a viral infection, there is a total defeat of the beta cells of the islets. In this case, we speak of type 1 diabetes mellitus, which requires lifelong administration of insulin in the form of a drug.
Symptoms of diabetes are itching, thirst, excessive urine production, weight loss, and dry mouth.
Advice There is a hereditary predisposition in the development of type 2 diabetes mellitus. If your blood relatives have or had diabetes, take care of your pancreas, limit your sugar intake and watch your body weight.
Pancreas and pregnancy
Pain in the pancreas during pregnancy is a dangerous and alarming symptom that should be paid attention to and investigated. As soon as alarming pain sensations begin during or after eating, you need to immediately contact a specialist.
Most often, the pancreas hurts:
- After overeating;
- Failure to comply with the prescribed diet.
In such a situation, to eliminate pain, the doctor recommends antispasmodics and other medications that relieve the pregnant woman from pain. Antibiotics cannot be prescribed as therapy for the pancreas during pregnancy, as they are dangerous for the mother’s body and the child.
The best choice for pain is the use of enzyme agents that reduce the load and relieve the pain itself.
Where does the pancreas hurt in a person, where is it located:
- You should know that the pancreas is located at the back of the stomach. It’s not for nothing that it’s called the “pancreas.”
- Located horizontally along the abdominal cavity (level of the first and second vertebra of the lumbar spine).
- She has a head, tail, body, and neck. It is shaped like a fish.
Head: located on the right side of the abdomen, in the area of the duodenum.
Tail: Located on the left side of the abdomen, close to the spleen.
Body: this is the name given to the middle region of the gland.
Neck: The thin area between the head and body.
It has many lobes in its structure. They constantly produce gastric juice. Size up to 25 centimeters long, weighing up to 80 grams.
Now you know where your pancreas is. Many people ask, where does it hurt on the right or left?
She can get sick:
- In the head area (right).
- Bodies (epigastric region).
- In the area of the tail there will be pain under the ribs on the left.
- But the pain is mostly very strong, “girdling”. It hurts in the stomach area and spreads to the back and sides.
- This condition will come over you immediately after eating a large, fatty or fried meal.
Seeking help from a doctor is strictly necessary! If treatment is delayed, the disease will develop into a protracted, chronic form with the following complications.
Consists of two types of glands:
95% exocrine: produces enzymes.
Endocrine 5%: The islets of Langerhans release hormones to control blood sugar.
Participates in the digestion of food by producing enzymes. They help process food in the intestines.
There are three types of such enzymes produced.
Symptoms of pancreatic pain: how to get rid of them?
- When symptoms appear in the form of severe pain in the upper abdomen, you should immediately contact a specialist. You should not eat anything until the ambulance arrives.
- If you are thirsty, then only non-carbonated mineral water is acceptable. Other drinks are not recommended.
- Taking medications before specialists arrive and make a diagnosis is dangerous . Elimination of pain may not be possible, but further diagnosis may become more complicated.
- Self-medication during pain is prohibited. If symptoms persist for more than 2 hours, the patient needs medical attention.
- When an inflamed state begins, you need to follow 3 rules: rest, hunger and cold . These requirements must be met until the ambulance arrives.
- When pain in the pancreas is severe, the patient should lie down and not eat. It is optimal to place a heating pad with ice on your stomach.
Characteristics of pain in pancreatic necrosis and cystic fibrosis
Pancreatic necrosis is a disease that destroys the pancreas. It is preceded by pancreatitis. Characterized by girdling pain that radiates to the left shoulder, persistent vomiting, stool instability, and rapid heartbeat.
The gland loses its ability to protect itself from the action of enzymes, intraductal pressure increases, the parenchyma becomes edematous and tissue necrosis progresses. Simply put, the organ destroys itself. Vomiting dehydrates the body, gas formation in the intestines is increased, and peristalsis is weak.
The abdomen is swollen, the pancreas is enlarged, and an inflammatory infiltrate may form, which is visible through the skin after a few days. These pathological changes cause shock, peritonitis, abscess, fibrosis and other complications. The main reason is alcoholism. The success of treatment lies in early diagnosis of destruction and adequate therapy.
Cystic fibrosis is a genetic disease characterized by cystic formations in the pancreas, intestines, and respiratory tract. The exocrine function of the gland is impaired, it is compacted. Pathological changes in the gland are observed already at 1 year of life and are steadily progressing. The infant cannot report his condition.
Warning signs that should prompt you to see a doctor:
- Retarded physical development, poor weight gain;
- Dry cough with shortness of breath, wheezing;
- Frequent, foul-smelling stools that are difficult to wash out of diapers and the potty;
- Swelling, too salty child's sweat, large loss of salts.
Sometimes the symptoms of cystic fibrosis are a little later - in preschool, less often in primary school age. Children who are able to describe their condition complain of intestinal colic, tension in the right side, suffer from vomiting, and stool instability.
The role of diet in the treatment of pancreas
We wrote about nutrition for pancreatic pancreatitis here.
Diet for pain in the pancreas plays a major role. Experts advise following attacks for 2 days on a fasting diet. This will help this body recover from shocks. It must be remembered that constant fasting contributes to the appearance of chronic pancreatitis.
There is a list of foods that should be removed from the diet for this disease. These include broths made from meat, fish, mushrooms and vegetables. Margarine, sour and spicy foods, and legumes are prohibited. Some vegetables are prohibited: radish, sorrel, onion and garlic. Coffee, strong tea and alcohol are prohibited.
The diet for pancreatitis includes boiled meat or steamed fish. The best vegetables to consume are zucchini, cauliflower and beets. Meals should be frequent (5-6 times a day). It is not advisable to allow a situation where you are constantly tormented by a feeling of hunger.
Read about the manifestations of pancreatic cancer in the early stages here.
Secretion
The pancreatic gland functions continuously. Even with an empty stomach, it produces a little juice, and when food enters the duodenum, the pancreas begins to actively produce pancreatic secretion.
According to experts, about a liter of pancreatic juice is produced per day. Externally, the pancreatic secretion has a neutral tint and a slightly alkaline reaction.
The juice contains enzymatic substances, the action of which is aimed at breaking down fats, carbohydrates, proteins, and nucleic acids.
- Chymotrypsin and trypsin, which are present in the juice, are necessary for the digestion of protein components, but they are synthesized in an inactive form, and are activated under the influence of intestinal secretions.
- Lipase digests foods high in fat, breaking down lipids into glycerol and fatty acid components.
- Lactase, amylase and malpase are needed by the digestive system for the active breakdown of carbohydrate foods. First, amylase breaks down starches into a disaccharide state, and then malpase and lactase convert disaccharide forms into monosaccharides.
The secretion of pancreatic juice begins within minutes of food entering the digestive system. Then this process continues for another 6-12 hours.
Moreover, the composition and duration of pancreatic secretion production depends on the specific food consumed by a person. For example, to digest bread, the pancreas functions at maximum speed, but to break down milk, it shows minimal activity.
The activity of the pancreas is regulated by nervous system structures. When the vagus nerve is irritated, the abundant secretion of pancreatic secretion is activated, and when the sympathetic nerves are irritated, the production of pancreatic juice slows down.
Secretion production is inhibited by various pain sensations, physical activity, sleep or too intense mental activity. But thoughts about food, delicious smells or the sight of food only increase the production of pancreatic secretions.
Phases
Secretion increases after food and persists for quite a long time (from 6 to 14 hours). The composition and amount of secretion produced is determined by the type of food and its volume. In general, secretion occurs in several stages.
- First comes the cerebral phase, during which, under the influence of stimuli, pancreatic secretion increases.
- Then comes the gastric phase, characterized by the active production of pancreatic juice and its vagovaganal reflex and gastrin maintenance.
- The final stage of pancreatic secretion is the intestinal phase, which begins after the gastric contents move into the cavity of the duodenum. The mucous membranes of the intestine are exposed to acidic contents, which provokes the release of secretin and the vagovaganal reflex - all of which support the stimulation of pancreatic secretion.
During the intestinal phase, self-regulation of pancreatic secretion, which depends on the contents of the duodenum, is very important. For example, if bicarbonates actively enter the intestine, they help reduce secretion.
Regulation
The processes of regulation of pancreatic secretion are controlled by nervous and humoral mechanisms. An increase in secretory activity occurs when eating food. At this time, the tone in the nervous system parasympathetic structures increases, which leads to increased production of pancreatic juice.
If the tone increases in the sympathetic nervous system fibers, then the production of secretions is inhibited, but at the same time acinar fermentation increases.
- A powerful stimulator of pancreatic secretion is secretin, produced by the duodenum.
- Cholecystokinin also has an enhancing effect on pancreatic secretion.
- The synthesis of pancreatic secretions is enhanced by substances such as insulin and bombesin, gastrin and hydrolysis products, serotonin and acetylcholine.
- The secretory activity of the pancreas also increases under the influence of bile salts, secretin, vasointestinal peptide or cholecystokinin, as well as hydrochloric acid secretion.
The production of pancreatic juice decreases under the influence of vasopressin and somatostatin, norepinephrine or glucagon, pancreatic peptide or calcitonin, etc.
Juice formation
Juice in the pancreas begins to form during the absorption of some food, which is notified to the pancreas by neurohumoral regulation.
On the mucous membranes of the oral cavity, gastric or duodenal walls there are cellular structures that react to food as an irritant. They transmit the impulse through the vagus nerve to the base of the medulla oblongata, to the digestive cerebral center.
After receiving such a signal, digestive processes are immediately activated. First, the signal enters the duodenum, to which the organ responds with the synthesis of secretin, and then to the stomach, which activates the production of gastrin. After gastrin and secretin enter the pancreas, the processes of producing pancreatic secretions begin.
The signal from neurohumoral structures activates pancreatic cells, which begin to produce secretions.
Pancreatic juice accumulates in lobules, each of which has its own duct, which subsequently flows into the common pancreatic ductal canal. With its help, secretions are transported to the duodenum.
Composition and properties
The secretion of the pancreas is a transparent liquid substance containing 987 g of water per liter of juice. In fact, pancreatic juice is 2% enzymes and 98% water. In this case, about a liter of such liquid is produced in 24 hours.
This is an alkaline liquid that has an alkalizing effect and neutralizes the acidic environment of gastric contents when they enter the duodenum. The pancreatic secretion contains a lot of components.
- Bicarbonates give the liquid an alkaline reaction.
- Sodium and potassium chlorides and proteins are also present in the secretion and are intended for the digestion of all types of food components.
- But the main composition is still represented by enzymatic components - amylase, protease and lipase.
Each enzyme is designed to break down specific food components.
Secretion products
For the health of intestinal tissues, it is extremely important that pancreatic juice is an alkaline liquid, because the walls of the duodenum cannot tolerate increased acidity, reacting to it with the formation of erosive and ulcerative lesions, sometimes bleeding and causing various complications.
A properly functioning pancreas provides protection to the mucous membranes of the duodenum by neutralizing hydrochloric acid gastric juice.
In general, the secretion may contain up to 15 different enzyme substances, although not all are fundamentally important for the digestive process.
The pancreas determines the nature of the food consumed and produces in the pancreatic secretion those components that are necessary in each specific case. In other words, the composition of pancreatic juice is determined by the B/F/U ratio in the contents of the stomach, and then the intestines.