Thalassemia is a disease that causes disruption of hemoglobin synthesis. The name of the pathology literally means “anemia of the sea coast.” The disease is inherited in a recessive manner and manifests itself as a result of genetic mutations. Knowledge of what kind of disease thalassemia is will be useful in family planning.
Classification
For some time, scientists were unable to figure out what thalassemia is. Only with the discovery of DNA and the properties of polypeptide chains was it possible to determine the following classification of pathology:
- Alpha thalassemia. At the same time, the synthesis of α-chains of hemoglobin A is suppressed in the body. The disease develops as a result of heterozygous carriage of the manifest, or “silent” thalassemia gene or homozygous hydrops of the embryo. Sometimes hemoglobinopathy N develops.
- Beta thalassemia. In the body, the mechanism of formation of the β-chains of hemoglobin A is suppressed. Includes Cooley's anemia, homo- and heterozygous δβ-thalassemia.
- Gamma thalassemia. The γ-chains of hemoglobin are suppressed.
- Delta thalassemia. The δ-chains of hemoglobin are inhibited.
- Thalassemia, due to which the structure of the blood protein responsible for the transfer of oxygen is disrupted.
- Lepore hemoglobinopathy.
- Constant Spring hemoglobinopathy (GS).
The most common is beta thalassemia. It can be small, large and in between. The minor form of the disease is characterized by mild symptoms. According to the severity of the course, the pathology is divided:
- mild (patients can survive until puberty);
- to moderate (life expectancy of patients does not exceed 10 years);
- to severe (death occurs in the first years of life).
Gamma and delta variants of the disease are extremely rare.
Specifics of diagnosing the disease
There are a lot of diagnostic methods that can be used to identify hematological diversification in the blood of a patient with thalassemia, which consists of biochemical microanalysis of blood and auxiliary ultrasound studies, supplemented by the patient’s medical history.
The initial diagnosis of thalassemia consists of examining the patient’s blood, which makes it possible to identify the presence of the disease in the early stages, as well as to detect which of the chains of red blood cell formation contains pathology. With thalassemia, a blood test will indicate low hemoglobin parameters, which rarely exceed fifty units. A low color coefficient, elevated reticulocyte count, and high serum iron criteria also indicate the presence of thalassemia. Laboratory blood tests will show distorted, hypochromic, target-shaped or flattened red blood cells.
Visual indicators of the presence of thalassemia may include a change in the patient’s skin color to a jaundiced tint, as well as facial features characteristic of Mongoloid races. When collecting a patient’s life history, it is advisable to pay attention to the patient’s ethnicity, since Latin Americans, Africans and Caucasians are more prone to the disease.
If thalassemia is suspected, the patient is referred for consultation to a hematologist and geneticist to confirm or refute the tentative diagnosis. To verify the diagnosis, the patient may be prescribed an additional ultrasound examination.
Thalassemia in children mainly manifests itself in a very bright form, which allows it to be identified in the early stages and treatment therapy to be started immediately. Modern medicine makes it possible to identify the presence of a disease in the fetus even during its gestation period using a special analysis called screening. In severe forms of the disease in the fetus, thalassemia can be a direct indicator for artificial termination of pregnancy. For people who have a family history of thalassemia patients, or who themselves are carriers of the mutation gene, it is important to visit a geneticist before planning a pregnancy in order to reduce the likelihood of having a child with the pathology.
Causes
Thalassemia is a genetically determined pathology that is inherited in an autosomal recessive manner. The immediate causes of the development of the disease are mutations in the gene that encodes the synthesis of a particular hemoglobin chain. The mutation occurs as a result of the synthesis of abnormal RNA, ineffective gene transcription. Due to mutations, the synthesis of polypeptide chains of the hemoglobin protein is disrupted, causing it to lose its functions.
An excess or deficiency of certain polypeptide chains of hemoglobin leads to disruption of the formation of red blood cells and to their gradual destruction. In beta thalassemia, “fetal” hemoglobin accumulates in red blood cells. It cannot transport oxygen to tissues and cells, causing them to experience oxygen starvation.
Important information: How is hemolytic anemia treated and its symptoms
Due to the proliferation of bone marrow, the skeletal structure is disrupted. As a result of oxygen starvation, anemia and ineffective formation of red blood cells, the normal development of the child is delayed.
The homozygous form of thalassemia has 2 pathological genes that are inherited from two parents. In heterozygous thalassemia, a person has only 1 gene, inherited from one parent.
Types of disease in violation of beta chains
The genes that control the production of beta chains can be in different states:
- Normal healthy gene. In healthy people, it is normal, which ensures the production of correct hemoglobin chains.
- Gene with partial deviations. This pathology allows the body to produce normal hemoglobin, however, it is produced in insufficient quantities.
- The gene is distorted so much that it completely prevents the formation of beta chains.
Structure of beta chains
Depending on the extent of the disease, the following types of beta thalassemia are distinguished:
- Minor thalassemia. In this type of disease, only one gene is damaged. There are practically no symptoms. Slight anemia may occur. Apart from anemia, a person does not complain about his health.
- With a more serious pathology of the gene responsible for the synthesis of beta chains, thalassemia intermedia is observed. As a result of disruption of the hemoglobin production process, red blood cells are formed either underdeveloped or small in size. Blood transfusions are not necessary, however, the subsequent condition of the body directly depends on its ability to live with low hemoglobin levels.
- Beta thalassemia type "major" is characterized by a violation of all genes responsible for the synthesis of beta chains. Patients with this type of disease require regular blood transfusions. This procedure allows the patient to live.
Symptoms
If a child is born with thalassemia, symptoms appear from the first weeks and months of life. The general clinical picture of the disease includes the following signs:
- change in the shape of the skull (it has an almost square shape);
- saddle-shaped nose bridge;
- the presence of a Mongoloid eye shape (i.e. the child’s palpebral fissure narrows);
- enlargement of the upper jaw;
- enlargement of the liver, spleen (these processes develop from the first days of the patient’s life);
- hemosiderosis (accumulation in tissues of the pigment hemosiderin, formed as a result of the breakdown of hemoglobin);
- pallor and yellowness of the skin and mucous membranes;
- deposition of bilirubin stones in the bile ducts;
- hydrops fetalis (this symptom is incompatible with life because the disease irreversibly affects the brain);
- delay in sexual and physical development;
- malocclusion;
- weakness;
- fatigue;
- decreased immune defense.
Due to progressive damage to bone tissue, patients suffer from pathological fractures. Hemosiderosis gradually leads to cirrhosis of the liver. Fibrous lesions (replacement of glandular tissue with connective tissue) leads to the development of insulin-dependent diabetes mellitus. The accumulation of hemoglobin breakdown products in tissues and anemia lead to heart failure.
Beta thalassemia minor is asymptomatic or with minimal clinical manifestations. In patients, the spleen is slightly enlarged and anemia is diagnosed. Constant fatigue is noticeable.
When a person develops heterozygous alpha thalassemia, hemoglobin alpha chains are not formed. Fetal hemoglobin is also not synthesized. This type of disease is incompatible with life. The disease leads to intrauterine death of the fetus due to dropsy or spontaneous termination of gestation.
With hemoglobinopathy H, anemia with phenomena of hemoglobin decomposition, splenomegaly (enlarged spleen), and severe disorders of the structure of bone tissue develop.
With beta thalassemia major, the following phenomena develop:
- skin lesions in the form of trophic ulcers (occur in response to disturbances in circulatory processes);
- cirrhosis of the liver, in which there is a progressive replacement of the glandular tissue of the liver (connective);
- damage to the pancreas with the development of symptoms of diabetes;
- severe delay in sexual development;
- frequent pneumonia;
- sepsis, i.e. blood poisoning.
Important information: How to treat chronic anemia
In the intermediate form of thalassemia, its first signs appear at a later age. Children do not lag behind in physical development, their appearance does not change. The main complication of the pathology is an enlarged spleen and damage to bone tissue.
Silvestroni-Bianco syndrome (beta thalassemia minimal) is asymptomatic and is diagnosed incidentally.
Frequency of occurrence
Thalassemia is inherited in an autosomal recessive manner. This means that it affects both boys and girls equally. The recessive nature suggests that children with thalassemia appear in those families where mom and dad are both carriers of mutations. Although they may not even realize that they are carriers, since the symptoms are sometimes invisible.
The average incidence is 1 in 100,000 people and may vary by region. Beta thalassemia is more common than alpha thalassemia.
How is the disease diagnosed?
Less than 5% of the world's population have hidden genes for thalassemia, which means it can appear in children whose parents had ancestors suffering from this disease. Complex diagnostics can reveal pathology. To do this:
- general examination of a sick child;
- blood test (shows a significant decrease in hemoglobin - even up to 30 g/l, a drop in the color index of the blood to 0.5);
- blood smears (diagnosed as faintly colored red blood cells);
- biochemical blood examination (an increase in the amount of bilirubin is diagnosed, a decrease in the ability of blood serum to bind iron);
- decomposition of hemoglobin on cellulose acetate film;
- studying the processes of hemoglobin biosynthesis in vitro;
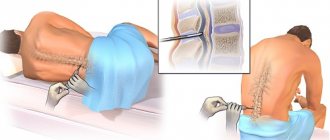
- bone marrow puncture;
- radiography of bones (areas of osteoporosis and striations of bone tissue are detected);
- polymerase chain reaction (it detects hemoglobin mutations).
Thalassemia diagnosis
There is a whole range of diagnostic measures aimed at identifying thalassemia. The main principle of diagnosing thalassemia: determination of characteristic hematological changes, disruption of the normal structure of the erythrocyte and identification of the hereditary nature of the disease.
The possible hereditary nature of the development of the disease is usually determined by collecting an anamnesis of the life and illness of a patient with suspected thalassemia. Another important diagnostic criterion for thalassemia will be the ethnicity of the patient - belonging to the peoples of the Mediterranean region, the peoples of Africa, Latin America, the Caucasus (thalassemia is most common to these peoples, as mentioned above).
The following characteristic changes will occur in the blood with thalassemia: a decrease in color index and hemoglobin level. In addition, with thalassemia, it is possible to determine the extremely characteristic shape of the red blood cells themselves: due to the disturbed structure of hemoglobin, it will be “target-shaped”, flattened (instead of the normal biconcave shape). Also, since due to the constant breakdown of red blood cells, the percentage of their relative content in the blood sharply decreases, the body automatically starts the formation of new ones, and therefore a certain number of future precursors of red reticulocyte cells can be found in the blood. For absolutely the same reasons, the red hematopoietic lineage in the bone marrow with a high number of normoblasts and erythroblasts (all these are cells of the erythrocyte series) will be enlarged (hyperplastic).
Also, for thalassemia, signs of extensive hemolytic damage will be characteristic: an increase in the indirect part of bilirubin, an extremely high level of iron in the blood serum (formed due to the breakdown and release of the erythrocyte pigment hemosiderin into the blood) and a visual indicator: hemolytic jaundice. It should be noted that only carrying out all the above diagnostic methods in one complex will allow us to suspect the probable presence of thalassemia in a patient.
Treatment
If a patient develops thalassemia, its treatment depends on the severity and form of the pathology:
- In severe cases of the disease, transfusion of whole blood or red blood cells has a short-term effect. These procedures are associated with the risk of developing hemosiderosis.
- Side effects develop much less frequently if a person is transfused with thawed or washed red blood cells. In parallel, iron chelates are used.
- Iron chelate is administered continuously and under the skin. For this, special pumps are used. All patients with severe thalassemia receive this drug using pumps 5 times a week throughout their lives. Moreover, the injection sites of the drug are constantly changed so that areas of local tissue damage do not appear. This treatment for thalassemia provides optimal results.
- During hemolytic crises, small doses of glucocorticosteroid drugs are administered.
- If the spleen is enlarged, it is removed. The operation is not prescribed for children under 5 years of age. It is best if such an operation is performed at 8-10 years of age.
- The most preferred measure is a bone marrow transplant. This is the only radical method of therapy. Finding the right bone marrow donor can be extremely difficult.
Important information: How hypochromic iron deficiency anemia is treated in adults, its symptoms and proper dietary nutrition for IDA
Patients need to follow a diet with a high content of foods rich in tannin: tea, cocoa, nuts, soy. These products significantly slow down the absorption of iron.
Symptomatic therapy is used:
- prescribing hepatoprotective drugs to support liver function;
- the use of ascorbic acid (vitamin C) to activate the excretion of iron.
Possible complications and prognosis
In severe forms of the pathology, hemosiderin accumulates in the tissues. Patients develop cirrhosis of the liver and diabetes. Myocardial hemosiderosis leads to the death of the patient.
In case of hemoglobinosis H, the spleen is removed. Due to the fact that patients are prone to developing infectious complications, they need to be vaccinated against pneumococcal infections.
The prognosis of most types of homozygous thalassemia is unfavorable. Patients die in infancy or young age. In severe forms of the pathology, the patient's life expectancy depends on timely treatment and prevention of hemosiderosis.
With the heterozygous form of thalassemia, the quality of life of patients does not suffer. Bone marrow transplantation improves prognosis.
Prevention
Since the disease thalassemia is genetically determined, primary prevention includes prenatal diagnosis. If both parents have thalassemia, the fetus should be tested. Sometimes the doctor recommends termination of pregnancy.
When examining pregnant women, fetoscopy and amniocentesis (under ultrasound control) are used. Subsequently, a genetic examination of the fetus is carried out.
Parents who have relatives suffering from thalassemia should consult a geneticist before planning a pregnancy. If necessary, genetic testing is prescribed.