You should know that herpetic encephalitis is one of the most dangerous diseases caused by the activity of the herpes virus in the human body. We have already discussed in previous articles the causes and symptoms of herpesvirus infection. Let us remember that this virus lives in the body of every person, entering it in childhood through the mucous membranes by airborne droplets. But it manifests itself only against the background of reduced immunity. Fortunately, many of us develop antibodies to the virus, so severe complications are rare.
Herpetic encephalitis is a pathology of herpesvirus infection, which affects the cerebral cortex. After a rash on the mucous membrane of the nose and mouth, the virus travels through the nerve canals to the brain. Most often, this disease manifests itself when immunity decreases due to prolonged stress, colds and respiratory infections, brain injuries, stroke, and cancer.
Children are most susceptible to this disease, since even a primary herpesvirus infection can progress to the encephalitic stage. In this case, the virus, passing through the neurons of the olfactory system, is transferred to the central nervous system. In adults, encephalitis occurs due to another strain of the virus entering the body and secondary infection, in which the herpes virus infection enters the central nervous system. Moreover, the virus can rest in it for many years, and under certain conditions become active again.
Description of the disease
Herpetic encephalitis is an acute infectious disease of the brain. The causative agent of the disease in 95% of cases is herpes simplex virus type 1, in other cases – type 2. Many experts consider the pathology as a complication of herpesvirus infection, which leads to damage to the frontal and temporal parts of the brain.
The disease develops more often in children and elderly patients, and the incidence rate increases in the spring. Doctors identify 2 peaks of incidence: 5-25 years and age over 50 years.
Important! The proportion of encephalitis, which is caused by herpes virus infection, does not exceed 11.5% of all cases of brain inflammation.
The disease may be primary if it develops immediately after infection. This option occurs mainly in childhood. In adults, herpetic encephalitis is secondary - it develops during an exacerbation of an infection present in the body.
Diagnostic methods
It is impossible to diagnose herpetic encephalitis based only on complaints and clinical picture. A thorough examination is required, the purpose of which is to differentiate the causative agent of the disease. Most often, to diagnose herpetic meningoencephalitis, a lumbar puncture is used, followed by a study of the cerebrospinal fluid using the PCR method. When analyzing the cerebrospinal fluid, an increased number of leukocytes is determined. Instead of clear, the liquor becomes xanthochrome - a special shade of yellow. It increases the content of protein and glucose.
A portion of the cerebrospinal fluid is sent for PCR diagnostics. The purpose of the study is to detect DNA of herpes types 1 and 2.
In the first 72 hours after the onset of clinical symptoms, PCR may give a false negative result. If there are characteristic signs of brain damage by herpes and MRI data, a repeat puncture is prescribed on the 4th day of the disease.
Neuroimaging of the brain is mandatory. The most specific method is MRI. During the first 24 hours, CT scan has a sensitivity of less than 50%, so it is not advisable to use it.
If MRI and CT cannot be performed, an EEG is performed. This method has higher sensitivity than computed tomography, but is not specific enough. The encephalitic recording corresponds to high-amplitude sharp waves and slow wave complexes, which are observed in the temporal leads. If a normal EEG is recorded from the first days of illness, this is a favorable prognostic sign.
Virological testing is not performed. This is a very long and expensive method, which is based on growing the virus in special nutrient media. Serological diagnosis is not used due to low objectivity and accuracy.
General blood tests are carried out, in which signs of inflammation are observed - an increase in the number of leukocytes, acceleration of ESR.
Causes and mechanism of occurrence
Infection with the herpes virus occurs mainly through airborne droplets, less often through household contact. Viral particles enter the human body through the oral mucosa, then enter nerve cells through the axons of olfactory neurons. After this process, replication and death of brain cells do not occur; on the contrary, the pathogen goes into a latent state. However, against the background of decreased immunity, herpes is reactivated and becomes manifest.
The risk of developing herpetic encephalitis increases significantly during a decrease in immunity against the background of such provoking factors:
- prolonged stressful situation;
- respiratory infections;
- immunodeficiency states;
- stroke;
- various oncopathologies;
- brain injuries.
In most cases, herpetic encephalitis is a complication of herpes, the rashes of which are localized in the oral and nasal mucosa. Less commonly, the disease develops against the background of a genital herpes virus infection. Doctors were unable to fully study the pathogenesis of the disease. At the moment there are 2 theories:
- Reactivation of viral particles in the nerve ganglia leads to the spread of herpes along the nerves that innervate the middle cranial fossa;
- The infection remains latent in nerve cells for a long period, where it is subsequently reactivated.
Complications and rehabilitation
Brain herpes can have extremely adverse consequences. In this pathological condition, neurological disorders may remain after the completion of the acute course of the disease. Complications that often occur with this disease include:
- migraine;
- meningitis;
- decreased mental activity;
- muscle weakness;
- partial memory loss;
- visual, speech and hearing impairments;
- attacks of dizziness;
- epilepsy;
- various mental disorders.
If rehabilitation is not carried out properly, these complications may persist for the rest of your life. If, after eliminating acute symptoms, a person is forced to work and is mentally overtired, takes alcohol or is exposed to other unfavorable factors, the consequences of the viral damage to brain tissue may become more pronounced.
Herpetic encephalitis
– extremely dangerous damage to brain tissue by the herpes virus. In the absence of targeted treatment, death occurs in approximately 80% of cases. Timely seeking medical help prevents the development of severe complications that will persist for a long time. To reduce the risk of encephalitis caused by herpes, it is necessary to maintain a high level of immunity: eat right, exercise regularly, and give up all bad habits.
Herpetic encephalitis ranks first in prevalence among infectious brain lesions. In half of the cases it affects children and young people under 20 years of age, as well as the older age group after 50 years of age. Before the use of Acyclovir, mortality reached 70%; today this figure is 28%. The disease has a severe course and is often accompanied by neurological complications.
Clinical picture of the disease
Herpetic encephalitis leads to the development of the following symptoms:
- damage to the ectoderm - rashes appear on the skin, in the area of the nasal mucosa and oral cavity;
- headache;
- increased body temperature, which is difficult to decrease after using antipyretic drugs;
- the development of seizures throughout the body, which are difficult to stop with medications;
- disturbance of thought processes, behavioral reactions;
- neurological disorders;
- the sense of reality is disrupted, which can lead to hearing loss or a coma.
Important! Viral particles mainly affect the gray matter of the brain, located in the temporal and frontal lobes.
Some symptoms are individual:
- visual impairment: sideways glance, double vision;
- speech distortion;
- movement disorder;
- memory losses;
- unilateral limb paralysis;
- the appearance of hallucinations;
- increased sweating;
- nervous excitement;
- increased blood pressure, tachycardia.
Sluggish herpetic encephalitis is also distinguished. Chronic inflammation of the central nervous system leads to periodic increases in temperature and the development of asthenic syndrome. This condition, after 6 months, provokes encephalitis, which is characterized by focal brain damage. Patients note the development of the following symptoms:
- reflex asymmetry;
- short-term convulsions;
- muscular dystonia;
- unilateral paralysis
This form of the disease often leads to the death of the patient due to resistance of viral particles to Acyclovir or late diagnosis.
Symptoms and treatment of herpetic encephalitis in children and adults
Herpetic encephalitis is caused by the herpes virus types 1 and 2; in neurology, the disease is characterized as severe. To get rid of its acute manifestations, prevent the development of severe complications and reduce the risk of death, doctors carry out mandatory hospitalization of the patient.
The disease is characterized by an acute febrile onset with vivid symptoms. Its development may be preceded by an acute respiratory infection, which occurs at lightning speed.
Herpetic encephalitis is caused by herpes virus types 1 and 2.
What's happened
Herpes brain is a disease of viral etiology. The lesions are localized in the frontal and temporal lobes.
Herpetic pathology occurs with equal frequency in people of both sexes. The following groups of people are most susceptible to developing the disease:
- From 2 to 30 years.
- After 50 years.
Damage to the brain by herpetic infection is accompanied by inflammation (more details here).
The lesions are localized in the frontal and temporal lobes.
Acute stage
The onset of the acute stage of the disease is characterized by rapid brain swelling. In parallel, necrotic processes develop in the tissues of the lower region of the frontal lobes and the medial part of the temporal lobes.
The disease begins abruptly (with headaches) and progresses quickly. In the absence of medical care, the following are observed for several days:
- Deterioration of the patient's condition.
- A more severe course of the disease, manifested by increased symptoms.
- Stupor (depression of consciousness, ability to function exclusively at the level of reflexes, numbness).
- Coma.
In the absence of medical care, coma occurs for several days.
Without medical intervention, brain swelling increases. In more than 50% of cases, deep coma develops and breathing stops (on days 1-3).
Sluggish course of the disease
Some patients experience indolent herpes of the brain. Its development occurs due to chronic inflammation of the central nervous system, characterized by:
- asthenic syndrome;
- periodic increase in temperature.
External manifestations of encephalitis are observed only after six months.
The percentage of deaths resulting from the indolent form of the disease is higher than mortality due to the acute form. This is due to late diagnosis of the pathology and resistance of the virus to acyclovir.
The sluggish course of the disease is characterized by periodic increases in temperature.
Symptoms
There is a triad of first signs of the disease that are characteristic only of encephalitis caused by herpetic infection. They are observed in all patients without exception.
What else to read: What to do if the lymph nodes are inflamed due to herpes
Classic symptoms include:
- Rapid increase in body temperature to 39°C.
- The appearance of convulsions, disturbance of movements (can be observed both in the whole body and in its individual parts).
- Disturbance of consciousness (ranges from confusion and oblivion to coma).
The classic symptom is the appearance of seizures.
The general clinical picture of herpetic brain disease in its acute form is similar to other types of encephalitis. Observed:
- disturbances in the functioning of the organs of vision, accompanied by double vision, strabismus;
- the occurrence of stiff neck muscles, drowsiness, vomiting and headaches;
- behavior changes;
- the appearance of hallucinations (olfactory and gustatory);
- increased sensitivity to light;
- memory and speech disorder;
- paralysis;
- instability while walking;
- increased sweating.
With herpetic brain disease, drowsiness is observed.
The appearance and severity of symptoms depend on the location of the herpetic lesion, its area, as well as the degree of tissue changes.
The sluggish form of the disease is characterized by:
- short-term convulsions;
- muscle dystonia;
- reflex asymmetry;
- one-sided paralysis.
Symptoms of low-grade encephalitis caused by herpes infection may be vague. This makes diagnosis difficult, increases the risk of complications, and increases the likelihood of death.
Symptoms of sluggish encephalitis may be vague - this increases the likelihood of death.
Causes
The pathogenic microorganism that causes inflammation enters the brain from the nasal cavity (transmitted along the branches of the nerves).
Encephalitis caused by the herpes simplex virus may not manifest itself for some time and remain dormant.
With a decrease in immunity, the herpetic virus concentrated in the nervous tissues is activated, and the development of the pathological process begins.
The risk group includes people who take drugs and abuse alcohol.
The risk group includes people who take drugs.
Treatment of herpetic encephalitis
If the development of encephalitis caused by a herpetic infection is confirmed, the person is hospitalized in the intensive care unit. Therapy is not carried out at home. This is due to the high likelihood of developing respiratory problems. Many patients require emergency ventilation.
The only treatment for the disease is drug therapy. To select the right drugs, the herpetic type of inflammation of the brain is differentiated from other diseases that have a similar clinical picture, and the degree of tissue damage is established.
Therapy is not carried out at home. This is due to the high likelihood of developing respiratory problems.
Diagnostics
Several examination methods help to recognize pathology and determine its severity. These include:
- Magnetic resonance imaging. It is a key method for identifying affected areas of the brain, assessing the localization of herpetic lesions and monitoring the dynamics of the development of pathology. Allows differential diagnosis with other types of encephalitis, as well as ganglioglioma (neoplasm), sclerosis, hypoxic disorders, and epilepsy.
- Electroencephalography. Helps to record the presence of characteristic periodic or semi-rhythmic bioelectrical activity in the brain. The presence of discharges indicates the development of encephalitis, which is of a herpetic nature.
- Cerebrospinal fluid examination. Makes it possible to detect the DNA of the herpes virus and the presence of antibodies (10-12 days after the onset of the disease). The study is used to confirm the appropriateness of the prescribed treatment.
- Biopsy of brain tissue. The analysis is performed if there is no result from treatment or it is impossible to make a diagnosis in another way.
What else to read What is postherpetic neuralgia and how to treat it?
Drugs
When treating herpetic brain lesions, medications are used. They are divided into 3 groups:
- Etiotropic (help eliminate the cause of the pathology). Acyclovir (Virolex, Zovirax) is used. It is administered intravenously. Immunostimulants are auxiliary medications. They enhance the immune response of cells, helping the body cope with herpes infection.
- Pathogenetic (affects affected brain tissue). To relieve inflammation, glucocorticoids (Cortisone, Dexamethasone) are used. Decongestants (Glycerol, Mannitol) help reduce swelling. To improve blood microcirculation, angioprotectors and metabolic medications (Cavinton, Piracetam) are used.
- Symptomatic (help eliminate external manifestations of pathology). Medicines used: antiparkinsonian (Parcopan), antipyretic (Paracetamol), anticonvulsant (Sibazon), improving the transmission of nerve impulses (Proserin).
Prevention
To prevent relapses, rehabilitation therapy is carried out. It helps restore normal brain function. To do this, the doctor prescribes:
- physiotherapeutic procedures;
- taking vitamins;
- massage;
- physical therapy.
To prevent relapses, rehabilitation therapy is carried out, one of them is physical therapy.
For prevention and quick recovery, experts recommend including in the diet a sufficient amount of macro- and microelements for the body.
Complications and consequences
The most severe consequence of herpetic brain disease is death. If you do not consult a doctor in a timely manner or the course of the disease is unfavorable, the patient may experience complications. These include:
- Herpetic meningoencephalitis. It develops when the cerebral membranes are involved in the inflammatory process. Causes memory loss.
- Partial or complete paralysis. Occurs when brain tissue becomes necrotic.
- Jacksonian type seizures. Most cases occur on one side of the body. They start with the finger of the hand. They spread to the entire upper limb, leg, face. Accompanied by impaired consciousness. Repetition of attacks is observed at different intervals.
- Epileptic seizures. They arise due to damage to the temporal lobe of the brain.
- Loss of coordination.
- The occurrence of auditory, visual, olfactory hallucinations.
If you do not consult a doctor in a timely manner or the course of the disease is unfavorable, the patient may experience visual hallucinations.
Many patients experience severe disorders of the nervous system (mental disorders, mental retardation, partial amnesia).
What else to read Features and treatment of recurrent herpes
Forecast
Herpes encephalitis is difficult to treat; in most cases, the course of the disease has an unfavorable prognosis. The mortality rate is:
- 20-25% of patients undergoing therapy;
- 70-75% of patients who did not treat the pathology.
Most survivors experience residual effects in the form of seizures or mental impairment.
Herpetic encephalitis in children
Herpes encephalitis can occur before birth. In this case, the infection penetrates the brain during pregnancy. In addition, in newborns the disease appears due to contact with carriers of the virus. The causative agent is the Epstein-Barr virus.
Signs of the presence of the disease are dysfunction of the brain. Convulsions, headaches, dysfunction of the digestive system, and coma occur. Often, before symptoms are detected in an infant, manifestations are diagnosed in carriers of the virus who have been in contact with the infant, infected adults.
If the disease is the result of a previous inflammatory process, the symptoms may resemble ARVI.
Treatment of herpetic encephalitis should begin immediately.
If this is not done, the consequences can be severe: damage to other organs is possible, in some cases the disease ends in death. Therapy is carried out with antiviral drugs. In addition, medications that strengthen the immune system are used.
In some cases, it is necessary to connect the child to a ventilator.
Source: https://gerpes.expert/oslozhneniya-i-posledstviya/gerpeticheskij-encefalit
Diagnostic measures
Differential diagnosis involves computer and magnetic resonance imaging of the brain, electroencephalography. The type of pathogen can be accurately determined by examining blood and cerebrospinal fluid using polymerase chain reaction (PCR). However, an increase in the level of antibodies in the patient’s biological fluids is typical only 10 days after the onset of infection. Therefore, the method allows only retrospective confirmation of herpetic encephalitis and the appropriateness of the prescribed therapy.
Important! In some cases, a biopsy of necrotic areas of the brain is indicated to determine the DNA of the virus. This method rarely leads to complications.
Diagnostics
Diagnostic measures for herpetic encephalitis should include:
- General clinical and laboratory tests aimed at assessing the general condition of the patient. Patients are shown a general and biochemical blood test, as well as a urine test. These tests make it possible to assess the negative impact on the body as a whole.
- Cerebrospinal fluid analysis. The material obtained during puncture of the spinal canal is subject to PCR analysis, during which DNA sections of the pathogen are identified. This study is very important for differentiating the virus from other pathogens.
- Instrumental diagnostics aimed at assessing the degree of damage to brain tissue, allowing to determine the foci of the pathological process. For this purpose, various types of tomography and Doppler scanning of cerebral vessels are used. The assessment criterion is the size of the ventricles of the brain, which makes it possible to assess the degree of hydrocephalus.
To diagnose herpetic encephalitis, a cerebrospinal fluid analysis is performed.
Properly constructed diagnostic measures help to select the most effective treatment regimen.
Treatment of the disease
A patient with herpetic encephalitis is isolated in an intensive care or resuscitation room, which is associated with the risk of developing respiratory disorders and dysgraphia. Acyclovir (Virolex, Zovirax) is widely prescribed to treat infection. Depending on the patient’s condition, the drug is prescribed orally or by injection. In the first 2 days, the antiviral agent is prescribed in large dosages (10-15 mg/kg three times a day). This tactic helps reduce patient mortality and prevents the development of severe complications. The course of therapy is usually 1-2 weeks.
Important! In a hospital setting, the body is detoxified and the water-salt balance is restored.
At the same time, many specialists prescribe interferons (Viferon, Cycloferon), but studies conducted by European scientists have not confirmed the effectiveness of such therapy. In case of severe cerebral edema, corticosteroids are indicated; the duration of treatment should not exceed 7 days. If the patient is in a coma, then tracheal intubation and ventilation are performed.
Treatment
Herpetic encephalitis is primarily controlled by antiviral therapy in the form of acyclovir. Therapy with acyclovir should be started immediately at the first signs of herpetic encephalitis, pending confirmation of the diagnosis. Because acyclovir is relatively non-toxic.
Medication
Include the following:
- Antiviral drugs (eg, acyclovir, famciclovir): will shorten the clinical course, prevent complications, prevent the development of latency and subsequent relapses, reduce transmission.
- Anticonvulsants (eg, carbamazepine, phenytoin): will stop clinical and electrical seizure activity as quickly as possible and prevent recurrence of seizures
- Diuretics (eg, furosemide, mannitol): normalize increased intracranial pressure during complications resulting from herpes infection
Complications of herpetic encephalitis
Herpesvirus damage to the brain can lead to the development of the following neurological and mental consequences:
- increased fatigue, apathy;
- paralysis;
- decreased memory and attention;
- headaches and dizziness;
- impaired coordination of movements;
- dementia, which leads to impaired cognitive function;
- decreased hearing, vision and speech;
- drowsiness;
- aggressiveness and irritability;
- urinary incontinence.
However, in rare cases (mild infection, adequate therapy, patient age, immune status), people can return to a full life, because the negative consequences of herpetic encephalitis are either absent or mild.
Complications
Herpetic encephalitis causes life-threatening conditions:
- swelling or compression of the brain;
- decortication (destruction of the brain cortex);
- acute attacks of respiratory and heart failure.
The long-term condition after suffering herpes encephalitis is characterized by the manifestation of mental disorders, hearing impairment, insufficiency of neurological reflexes and epileptic seizures.
After brain herpes, complications that are irreversible are highly likely to develop. Children, after suffering from inflammation, suffer from epilepsy, various paralysis, and hydrocephalus develops at an early age.
In adults, complications of herpetic infection are:
- Jacksonian type cramps - they can affect only certain muscle groups or all;
- multiple sclerosis – there is a constant progression of the disorder, which ultimately leads to complete disability;
- Alzheimer's disease;
- dementia – weak-mindedness, which is often observed in old age;
- acquired schizophrenia;
- Parkinson's disease.
How dangerous is herpetic encephalitis in an infant? Firstly, the disease belongs to the list of those characterized by high mortality. Secondly, even if the baby survives, there may be irreversible pathological changes that will lead to the child’s incapacity in the future.
In severe cases of herpetic meningoencephalitis, disturbances of consciousness lead to coma, which in 90% of cases ends in death.
The consequences of focal necrotic changes are manifested by the persistence of symptoms of brain tissue destruction after the acute period of the disease. Can be stored for life:
- epilepsy;
- impairment of cognitive abilities (memory, speech, attention);
- loss of self-care skills;
- behavior change.
The disease can become chronic with periodic phases of exacerbation. In children, encephalitis leads to intracranial hypertension syndrome, which is caused by impaired circulation of cerebrospinal fluid. Convulsive seizures and delayed psychomotor development may also persist.
Prevention of herpetic encephalitis
Infection with herpes virus infection occurs through airborne droplets, therefore, to prevent infection, it is recommended to carry out a set of measures as for a cold: increase immunity, avoid close contact with sick people and carriers, take multivitamin complexes.
To prevent infection with genital herpes, it is recommended to use condoms while taking antiviral drugs. Particular attention should be paid to the prevention of herpesvirus infection in newborns.
Herpetic encephalitis is a dangerous viral infection that requires immediate and effective treatment. Otherwise, the disease leads to irreversible changes in the brain and death of the patient. Doctors are developing a vaccine drug that will reduce the frequency of relapses of the infection. However, the effectiveness of vaccination has not been proven.
Similar articles:
- Herpes type 4
- Symptoms and treatments for herpes zoster (shingles)
- Herpes type 3
- Causes of herpes
Great article 0
Therapy methods
Treatment of herpesvirus is carried out in the intensive care unit in the intensive care unit. The main therapeutic drug is Acyclovir. Other antiviral agents (Famciclovir) are also used. Medicines in large doses are administered intravenously.
Combating complications includes prescribing broad-spectrum antibiotics to prevent the development of a bacterial infection in a bedridden patient. The rest of the therapy is symptomatic. Drip administration of water-salt solutions and glucose is prescribed to maintain brain function, correct the basic balance and detoxify. Cardiac activity and respiratory function are constantly monitored, and measures are taken to prevent cerebral edema. If necessary, perform artificial ventilation.
For convulsive syndrome, anticonvulsants are used to combat feverish conditions
. During the recovery period, neuroprotectors, nootropics and vitamins are needed. Depending on the degree of dysfunction of the brain, classes with a speech therapist or rehabilitation doctor may be required. In 1-2% of patients, the disease passes without consequences. In other cases, there are persistent residual effects.
Herpes brain (herpetic encephalitis) is a serious and dangerous disease that manifests itself in the form of inflammation with a rapid course, which leads to changes in the brain. Certain strains of herpes simplex, namely HSV-1 and HSV-2, can cause this disease.
The herpes virus contains DNA chains, has a size of 150 nanometers and a covering shell consisting of lipids. When the human body is infected, it penetrates inside the cells, where it divides, but does not cause any harm - the latent stage (inactive). As soon as the body succumbs to the influence of certain factors, the pathogen enters the reactivity stage. In most cases, the pathology occurs in people 5-30 years old; after 50, it most often acts as a complication.
The herpetic type is the most common form among all known encephalitis. In many patients who carry the herpes virus pathogen in their body, this infection has settled in the brain and is activated in the event of any injury to the organ. This can happen while taking certain medications or prolonged exposure to low or high temperatures. For the rest, infection occurs from exogenous causes. Studies have found that the peak increase in infection cases occurs in the spring.
Causes
The main reason for the development of herpes encephalitis in brain tissue is infection with a viral agent. Scientists have not yet reached a consensus on the conditions for the initiation of the disease. It is unclear whether the pathology occurs due to primary infection or reactivation of the viral agent.
Typical clinical cases (about 25%) are initiated by reinfection, when the patient simultaneously had several strains of HSV found in the studied material from different parts of the head (nasopharynx, brain).
It is assumed that the virus penetrates the tissues of the central nervous system through the trigeminal nerve ganglia or olfactory bulbs, which determines the localization of the pathological focus - the anterior parts of the brain. The spread of the infectious agent through the nerve structures is carried out through the fibers that innervate the vessels located in the meninges.
Basic treatment methods
Treatment of herpetic encephalitis must be started immediately, because in its absence, 80% of patients quickly fall into a coma and die, therefore, timely identified symptoms of infection give a person a chance to live. Sometimes the disease develops at lightning speed and is accompanied by rapid swelling of the brain and subsequent cessation of breathing, and if the person still survives, the symptoms develop in the opposite direction, but persistent residual effects remain. In rare cases (1–2% of all patients), a person recovers without consequences.
Treatment of herpetic brain damage takes place in a hospital setting, because the risk of sudden respiratory arrest is very high, and doctors begin drug therapy even without confirming the diagnosis with laboratory tests. The patient is prescribed Acyclovir (in high doses and intravenously) as the main drug, and additional therapy includes the use of antibiotics that can penetrate the blood-brain barrier, immunomodulatory agents (Interferon), and drugs for symptomatic treatment (antipyretics, anticonvulsants, neuroprotectors).
Herpetic encephalitis is a dangerous disease, the lack of treatment of which can lead to irreversible consequences, therefore, at the first symptoms of its development, you must consult a doctor. Today, scientists are working on creating a universal antiherpetic vaccine, but its effectiveness has not yet been sufficiently studied. The only available method of preventing the development of encephalitis is the regular use of medications that improve the functioning of the immune system.
Herpes viruses are common infectious agents that cause characteristic rashes in the skin, eyes (HSV type 1) and external genitalia (HSV type 2). An infectious agent can cause various diseases of the central nervous system. Herpetic encephalitis, which occurs against the background of a viral infection, is especially severe. The share of the disease in the general structure of encephalitis of viral etiology is 20%. Prevalence – 2-3 cases per 1 million population annually.
Symptoms
The onset of the disease is characterized by an acute course. The elevated body temperature lasts for 3-4 days. Then the clinical picture is complemented by neurological symptoms. Typical of the pathology is depression of consciousness, often to the point of coma, which develops against the background of rapidly progressing swelling of the brain tissue. Symptoms of herpes encephalitis include:
- Temperature rises to 38-40°C.
- Pain in the head area.
- Attacks of nausea and vomiting.
- Stiffness of muscle tissue in the neck area.
- Convulsive syndrome.
- Epileptic seizures of generalized (distributed throughout the body) and focal type.
- General weakness, malaise.
Signs of damage to the cranial nerves and respiratory manifestations (cough, runny nose, hyperemia of the mucous membrane of the pharynx) often appear. Symptoms of herpetic encephalitis are supplemented by focal manifestations characteristic of damage to the temporal (in 90% of cases) and frontal lobes:
- Anosmia (loss of smell), taste, olfactory hallucinations.
- Epileptic seizures of partial (partial, local) type.
- Hemiparesis is paresis in one half of the body.
- Psycho-emotional disorder, behavioral disorders.
- Aphasia is the loss of formed speech.
- Hemianopsia (bilateral blindness affecting half of the visual field).
- Deterioration of cognitive abilities - mental activity, memory.
The disease progresses rapidly. Within a few days, stupor (profound depression of consciousness) and coma may develop. The lack of correct therapy leads to the death of the patient. The progression of the disease is usually accompanied by increasing cerebral edema, which initiates transtentorial herniation syndrome - the middle part of the temporal lobe is wedged through the area of the cerebellar tentorium.
As a result of this effect, deep coma and death due to respiratory arrest occur rapidly (24-72 hours). On average, the duration of the infectious period is about 5 days, the febrile period is about 12 days. An increase in neurological deficit occurs against the background of high temperature and increased intoxication. A comatose state often develops after 6-12 days.
Herpes encephalitis in children is manifested by pain in the head, nausea, vomiting, and psychomotor agitation. In 75% of cases, pediatric patients develop symptoms: apraxia, aphasia, agnosia (impaired auditory, visual, tactile perception). Often the clinical picture is supplemented by tremors of the limbs, increased muscle tone, and symptoms of damage to the pyramidal tracts (motor disorders).
Symptoms
Encephalitic herpes likes to affect the temporal and frontal lobes of the brain, where necrotization and hemorrhagic lesions most often occur.
The main symptoms may manifest themselves in different ways, depending on the severity and location of the affected area of the brain. Experts have identified a specific triad of symptoms that are characteristic specifically of herpetic inflammation:
- Acute fever – sudden hyperthermia of the body (up to 39 degrees). It is difficult to bring down such a temperature, even by taking antipyretic drugs.
- Jacksonian type seizures - they can affect the entire body or certain areas of it.
- Disorder of consciousness - ranging from short-term oblivion to deep coma (this disorder is almost always disappointing, since in 90% of cases, people immersed in a coma do not survive).
These signs will certainly manifest themselves in all infected people, but there are also some among them that are purely individual for each specific case. These include:
- Dysfunction of the oculomotor nerve - patients may experience strabismus and a feeling of double vision.
- Rapid hallucinations (a common phenomenon that accompanies other central nervous system pathologies and requires immediate treatment).
- Increased sweating.
- Short-term memory loss.
- Unsteadiness when walking.
- Monoparesis or a disorder of motor functionality on one side of the body (the result of damage to the temporal lobe of the brain).
- Excited state.
- Speech disorder.
In addition, damage to the brain of a herpetic nature can be assumed by such signs as an increase in protein content in the cerebrospinal fluid, a high level of ESR and lymphopenia. Infants may develop decortication or hydrocephalus.
Characteristics of the disease
According to statistics, the herpes virus is detected in 90% of the population. In approximately 20% of cases, a viral infection causes serious disruptions in the body's functioning. Once entering the body (hematogenous, neuronal route), HSV (herpes simplex viruses) remain in it forever. An infectious agent can be in different states, which determines the degree of its impact on health. The following forms of pathology are distinguished:
- Latent (hidden).
- Persistent (chronic).
- Progressive (with increasing symptoms).
- Recurrent (with alternating periods of progression and remission).
Under favorable conditions, reactivation of a latent infection occurs. The acute form of the pathology can lead to loss of ability to work, disability, and death. HSV is characterized by pantropism - the ability to infect different organs and systems. Infectious agents cause pathological autoimmune reactions, induce the formation and growth of malignant neoplasms, and cause perinatal pathologies.
Penetrating into the central nervous system, viruses provoke the development of temporal lobe epilepsy of the median type. Encephalitis caused by viral agents is a common (about 76% of cases) forms of encephalopathies of various (bacterial, fungal, anaplasmic) etiologies. Herpetic encephalitis in children usually occurs acutely and provokes the appearance of persistent neurological deficits, often of a focal type. The disease often causes retardation in the mental and physical development of the child.
Herpetic encephalitis in adults is more often detected in patients of two age groups: under 30 years of age and over 50 years of age. In most cases (about 95% of cases), the infectious agent is type 1 HSV, which affects the mucous membrane and skin of the face in the mouth area. HSV type 2 affects the mucous membrane of the genital organs. It is more often detected in newborns, who are transmitted from an infected mother during fetal development.
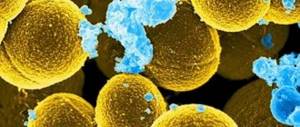
In the body of 70-90% of infected people, antibodies to the viral agent are detected, which in normal conditions helps to suppress the activity of HSV by one’s own immune system. From the point of view of pathomorphology, the disease is an acute necrotizing process, which is characterized by the appearance of multiple foci of hemorrhage, lymphocytic and plasmacytic infiltration in the brain tissue.
In the acute stage of the disease, eosinophilic elements (granulocyte leukocytes) are found in the nuclei of nerve cells (neurons, neuroglia). Typical localization of the pathological focus is the medial (middle) part of the temporal lobes and the orbital (lower) part of the frontal lobes. In the residual (after the acute stage) stage of the course, cystic-glial tissue is formed at the site of foci of necrosis.