What is vulvodynia?
Vulvar pain (or vulvodynia ) is a clinical condition characterized by the presence of chronic pain (lasting at least 3 months) located in the vulva (female external genitalia), without any apparent cause.
Vulvodynia is a clinical condition (symptom) of great importance for various reasons:
- This is a problem that affects many women, although many tend not to talk about this condition with their doctor;
- in addition to pain, patients also experience other symptoms (itching, burning, swelling, vulvar discomfort), which can be particularly unpleasant and interfere with the normal course of daily activities;
- although this is not a dangerous condition, it can be associated with complications, especially psychological, which can disrupt daily life, but above all relationships between couples and intimacy with the partner;
- Although vulvodynia is widespread, it is a disease that is largely underdiagnosed and is often traced solely to stress or psychological conditions (anxiety, depression);
- There are many medications available to treat vulvodynia that are not universally effective (some women benefit from medications that are not effective for other women), so treatment must be individualized and often very lengthy; note, however, that many women can successfully overcome this problem;
- The success of treatment is based primarily on dialogue: overcoming embarrassment to talk to a doctor or gynecologist is the first therapeutic step.
It is very difficult to estimate the number of women actually affected by vulvodynia, as many tend not to bring symptoms to the attention of their doctor; The prevalence in Russia can be approximately estimated at 200,000/6,000,000 people of any age (from adolescence to postmenopausal period).
Prevention measures
To prevent vulvodynia, it is recommended:
- wear underwear with hygroscopic properties;
- stop wearing tight underwear;
- wash your genitals twice a day;
- use special gel or soap intended for intimate hygiene;
- undergo regular gynecological examinations (at least twice a year);
- promptly treat gynecological and systemic diseases;
- avoid casual sex.
Measures to prevent this form of genital diseases are:
- selective approach to choosing sexual partners;
- using a condom during casual sex;
- prevention of injuries to the external genitalia;
- compliance with the rules of intimate hygiene;
- maintaining normal hormonal levels and blood sugar levels;
- increasing immunity;
- refusal to use scented pads, synthetic underwear and tampons;
- use of hypoallergenic intimate hygiene products;
- avoiding stressful situations and hypothermia;
- timely treatment of acute and chronic inflammatory diseases;
- regular examination by a gynecologist (at least 2 times a year);
- limiting the consumption of foods rich in oxalates;
- prevention of viral diseases (HPV infection and herpes).
In order to prevent complications with vulvodynia, you must consult a doctor and strictly follow the treatment regimen. There is no specific prevention.
Today, the problem of treating diseases of the vulva is topical, since it presents great difficulties in achieving a therapeutic effect and is chronic in nature. Translated, “Vulvodynia” means “painful vulva.” Vulvodynia is a condition of discomfort experienced by women in the groin area.
To avoid the development of such a disease, representatives of the weaker half of humanity should follow several simple preventive recommendations.
These include:
- engaging in protected sex;
- refusal of promiscuous sex life;
- wearing underwear only made from natural fabrics;
- compliance with personal hygiene rules;
- avoiding the use of intimate products that cause allergic reactions;
- timely and complete treatment of any somatic diseases in their acute or chronic course;
- avoiding hypothermia;
- minimizing stressful situations;
- regular visits to the gynecologist.
READ MORE: How to treat oliguria with folk remedies
Vulvodynia has a favorable prognosis, but significantly reduces a woman’s quality of life, and is quite difficult to treat. Depending on how long the patient lives with this pathology, the risks of complications of the underlying disease increase.
If you think that you have Vulvodynia and the symptoms characteristic of this disease, then a gynecologist can help you.
Classification
The vulva is the external part of the female genital organs, which includes:
- labia majora;
- labia minora,
- vestibule of the vagina;
- clitoris.
Based on the location of vulvodynia, you can determine:
- generalized : pain is felt indiscriminately in any area of the vulva, affecting several areas at the same time, or it can migrate, occur spontaneously and be aggravated by pressure in one of the painful areas;
- localized : only part of the vulva is affected, and pain is most often caused by pressure on the affected areas.
Symptoms
The main symptom of this pathology is discomfort or discomfort. The pain has the following characteristics:
Pain in the area of the vaginal opening and labia has been bothering me for six months or more.
Additional symptoms are:
- pain on palpation of the vulvar ring (there is a lot of glandular tissue in this area);
- burning;
- paresthesia (tingling or crawling sensation);
- redness of the skin and mucous membranes;
- feeling of heat;
- vaginal dryness.
Causes of vulvodynia
To be considered vulvodynia, the pain must be chronic (lasting more than 3 months) and idiopathic in nature (without a specific cause).
When one or more causes can be recognized, it is better to talk about secondary pain in the vulva , which is easily recognized by the presence of the vulva and treatable damage when the cause that provoked it is eliminated.
Reasons considered include:
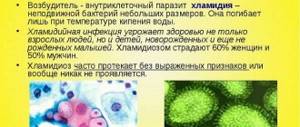
- genital infections (herpes in the intimate area, bacterial vaginosis, candidal infections, Trichomonas vaginalis...),
- neoplasms of the vulva;
- lichen sclerosus;
- furuncle;
- Bartholin gland abscess;
- vulvar warts;
- atrophic vaginitis;
- local injuries in the vaginal area;
- exposure to harmful agents or chemicals.
Primary vulvodynia is free from visible damage, but there may be functional or anatomical microscopic changes at its basis. In fact, there is a chronic inflammatory process at the level of the vulva, characterized by a predominance of mast cells, which release factors that can enlarge nerve endings and increase sensitivity to stimuli (hyperesthesia) or abnormal perception: in simple terms, normally painless stimuli are perceived by the woman as painful (a process called allodynia).
Causes of pathology
There are quite a lot of factors that provoke the formation of pathology. For convenience, they are divided into several groups:
- spasms of the muscles of the vagina and vulva;
- damage to vulvar nerve endings;
- imbalance of hormones (estrogens) during the menopausal period;
- pathologies of the vulva, which are accompanied by degenerative changes in tissue (dermatoses);
- the woman is allergic to synthetic underwear and hygiene products;
- somatic illnesses with a chronic course (diabetes, kidney diseases, and so on);
- a history of inflammatory and infectious pathologies affecting the external genital organs (vaginosis, vulvitis, vulvovaginitis).
READ MORE: How to treat old bumps from injections
Signs and symptoms of vulvodynia
The main symptom of vulvodynia is pain , usually of sudden onset, lasting for months or years, and can come in various forms:
| Nature of pain | Acute (like a sharp burning sensation), piercing, pulsating. |
| Localization | Localized (in the vaginal area) or generalized (throughout the body). |
| Duration | Continuous or paroxysmal pain. |
| The beginning of the pain | Spontaneous, caused by pressure stimulation, physical activity (walking, cycling), sexual intercourse or even rest. |
| Associated signs/symptoms | Itching of the vulva and/or vaginal dryness. |
| Appearance of external genitalia | Normal or scratches (with itching). |
Symptoms can be so severe that they can make it difficult to carry out daily tasks, work activities, and sometimes even trivial activities.
Definition and classification of the disease
Modern medicine has combined vestibulitis in women and vulvodynia, previously considered different pathological forms, into one nosological unit called “vulvodynia.”
Based on the above etiological factors, vulvodynia is divided into:
- allergic;
- psychogenic;
- infectious – this also includes the herpetic form;
- caused by somatic ailments;
- atrophic;
- dystrophic.
Depending on the clinical course, the following forms of pathology are distinguished:
- Provoked - pain occurs only at the moment of irritation of the vulva. This may be caused by sexual contact, intense sports, or the insertion of a sanitary tampon.
- Unprovoked – pain appears spontaneously, often in moments of physical calm, in particular during night rest.
It is also worth noting that vulvodynia is a concept that combines several diseases and pathological conditions, namely:
- cyclic;
- vulvar vestibulitis;
- dysesthetic form of the disease.
Complications of vulvodynia
Although not a dangerous clinical condition, vulvodynia can have dangerous psychological consequences if left untreated, leading to severely impaired quality of life if left untreated.
Problems with your partner
- Dyspareunia (pain during sexual intercourse),
- decreased libido (decreased sex drive),
- Difficulty in finding pleasure during a relationship.
These are problems that can make a woman feel inadequate, unable to satisfy her partner, and prevent her from living a peaceful and fulfilling relationship.
These factors can ruin a couple's relationship, especially when there is no good, sincere dialogue about the problem with the partner, which can provoke the woman's psychological closeness, aggravating the situation, so that a vicious circle is formed.
Psychological disorders
- Anxiety,
- depression,
- difficulties in communicating with people,
- difficulties in solving everyday problems of various nature.
These are the consequences of discomfort caused by vulvodynia, which can prevent you from leading a full life.
Sleep disorders
Often a woman who suffers from this chronic condition also develops insomnia: pain and reduced sleep hours may be the basis:
- irritability,
- difficulty concentrating,
- poor performance at work or school.
Changing the way you perceive your own body
This disorder in extreme cases can lead to more serious problems, especially in adolescents, such as anorexia and bulimia.
Accompanying illnesses
Vulvodynia is often associated with other pathologies associated with hypertension of the pelvic muscles:
- vaginismus (involuntary contraction of the pelvic muscles, which makes sexual intercourse painful or impossible);
- constipation (dysfunction of defecation or anismus) due to impaired relaxation of the pelvic muscles necessary for defecation;
Treatment of vulvodynia
Treatment for vulvodynia should only begin after a thorough examination. There is no single method of treating such a disease; it is individual for each patient and its effectiveness depends on the immediate cause that caused it. Before prescribing treatment, the doctor must exclude possible causes of pain, for example, the presence of bacterial or fungal infections, diabetes mellitus, and various skin lesions. After a thorough analysis of the symptoms, the doctor will prescribe treatment and recommend ways to reduce pain. I will say right away that the effect of the prescribed treatment may not appear immediately; months may pass when the symptoms of the disease decrease.
Treatment of infectious processes is carried out by prescribing antibiotics, antiviral, antifungal and other agents. Corticosteroids are usually used to treat dystrophic diseases of the vulva. In the treatment of vulvodynia caused by mental disorders, a specialized approach is required, as in the treatment of somatic diseases. To treat atrophic vulvovaginitis, systemic and local hormone replacement therapy (estrogen creams to reduce pain, vaginal estrogen tablets to eliminate dryness or atrophy, etc.) are used.
To reduce chronic pain, tricyclic antidepressants (amitriptyline, desipramine (Petylil) and nortriptyline (Aventil, Allegron), anticonvulsants carbamazepine (Finlepsin) and gabapentin (Gabagamma), as well as antihistamines to reduce itching (hydroxyzone) can be prescribed. For pain relief, lidocaine ointment is prescribed, which temporarily relieves pain symptoms.
Autogenic training (achieving a relaxed state) is also a good way to reduce pain. It is expressed in self-control of the reactions of the pelvic muscles, which can spasm in anticipation of pain, thereby causing chronic pain.
Physiotherapeutic procedures can be used to treat vulvodynia, such as: massage, stimulation of nerve endings, exercises to strengthen the pelvic muscles, therapeutic ultrasound, as well as exposure to trigger points with steroid hormones in combination with an anesthetic, which helps relieve painful tension in the muscles.
Diagnostics
Often, just a glance at the symptoms and signs by a doctor or gynecologist is enough to make a diagnosis, however, additional tests are needed to rule out the presence of other diseases responsible for secondary vulvodynia.
- Medical history : It is very important to collect data on symptoms and identify causative factors (history of recurrent infections, predisposing psychological conditions, if any, history of sexual abuse).
- Objective examination : it is necessary to examine the vulva area to exclude the presence of concomitant diseases (infections, neoplasms, lichen).
- Q-tip test : The doctor uses a Q-tip to stimulate different areas to detect painful areas.
Reasons for the development of the disease
Vulvodynia is not an independent disease. The reasons may be:
- Pudendal nerve neuropathy. The cause is compression of the nerve fibers. Risk factors include difficult childbirth, trauma and malignant tumors.
- Herpetic infection. The causative agent of the disease is tropic to nervous tissue and, under favorable factors (decreased immunity), can cause neuropathy.
- Vestibulitis. This condition is characterized by damage to small glands in the vestibule of the vagina.
- Operations on the pelvic organs.
- Sharp fluctuations in blood glucose levels.
- Vulvovaginal candidiasis (a fungal disease from the STI group).
- Infection with human papillomavirus.
- Rape.
- Uncontrolled use of oral contraceptives.
- Changes in hormonal levels.
- Increased nerve fiber density.
- Kidney failure.
- Lichen sclerosis.
- Dermatoses.
- Increased muscle tone.
- Mental disorders.
- Inflammatory diseases of the external female genital organs.
- Exposure to chemicals.
Vulvodynia may be caused by the use of scented pads and intimate hygiene products . Irritation of the vulva is possible from contact with washing powder or underwear. Pain syndrome can also occur in a child (girl), but this is rare.
Care and protection
Although the underlying pathology is often psychological, there are numerous treatments for vulvodynia that can be combined with targeted psychological support.
Vulvodynia is a treatable condition in most cases, although treatment often takes a long time (months, sometimes even years).
The biggest difficulty is that there is no universal treatment that is certainly effective, but it is likely that a patient must try a large number of drugs before finding one that works for her, since drugs that work for one patient may not work for someone else.
Lifestyle changes and what NOT to do
- Avoid harsh detergents or those that are not suitable for intimate cleaning.
- Avoid perfumed products, creams and ointments.
- Avoid tampons.
- Avoid using spermicidal creams as birth control.
- Avoid synthetic underwear.
- Avoid too tight trousers, tights, leggings, bodysuits.
- Avoid foods that can irritate the bladder (beans, chocolate, chili peppers, dried fruits).
- Avoid sitting for long hours.
- Avoid excessive physical activity.
- Avoid sports such as cycling to avoid putting pressure on the vulva area.
- Avoid spending many hours in the pool.
Lifestyle changes you NEED
- Good intimate hygiene, washing the external genitalia after urination with warm water.
- It is preferable to use high-quality intimate products with a neutral pH.
- External absorbents must be used.
- Use soft toilet paper.
- Use cotton underwear.
- Wear comfortable, loose clothing.
- Change wet clothes (for example, after training).
- Dry your intimate area thoroughly after showering.
- Use soft cushions for chairs, sit on soft ones.
Treatment
Treatment tactics for vulvodynia are selected depending on the cause of the disease:
- if the pathology was provoked by infectious processes, the patient is prescribed antibacterial, antiviral or antifungal drugs;
- for mild symptoms, local medications are used: vaginal suppositories or tablets “Nystatin”, “Neomycin”;
- Acyclovir and interferon inducers help well with herpes infection;
- if the disease is of a dystrophic nature, vaginal suppositories and ointments are used that can activate the natural regeneration processes of the epithelium;
- in severe forms of the disease, medications are administered intramuscularly or intravenously;
- vulvodynia during menopause is treated with hormonal drugs;
- with allergic etiology, pain is accompanied by itching, so in this case, tests to identify the allergen and subsequent treatment with antihistamines are indicated.
The chances of positive dynamics and full recovery can be increased if:
- maintain sexual rest, avoid situations that may lead to the formation of microcracks and vaginal injuries (use of tampons, sports);
- limit consumption of foods high in calcium oxalate (chocolate, asparagus, parsley);
- perform physical therapy – it will help strengthen the pelvic floor muscles, eliminate aching pain and relieve muscle spasms;
- carry out physiotherapy, paraffin treatment, take mud and soothing sitz baths.
Treatment of vulvar pain
In order of invasiveness, to relieve pain, the gynecologist may advise:
- Bath with warm water.
- Apply a heat source to the affected area (a cloth heated with an iron, a hot water bottle, special products that can generate heat...), while other women benefit from applying ice (not in direct contact with the mucous membrane, but wrapped in a cloth) ).
- Preparations:
- Oral antihistamines, to treat itching.
- Lidocaine (local anesthetic), for intermittent pain, or before sexual intercourse.
- Cortisone-based ointments.
- Estrogen-based ointments.
- Antidepressants (tricyclics, SSRIs) orally.
- Opioids (painkillers).
- Anticonvulsants for the treatment of neuropathic pain (Carbamazepine).
Treatment of vulvodynia
A variety of measures are used to treat vulvodynia, but none of them are optimal in terms of effectiveness and long-term prognosis. It is believed that this is due to the lack of a CNS component in treatment, an incomplete understanding of the pathogenesis of this condition, and a failure to take into account the psychosocial aspect. It is probably best to consider chronic vulvar pain as one of the systemic pain syndromes.
Treatment algorithm for vulvodynia
- Nonspecific but necessary measures: patient education on vulvodynia;
- consulting;
- avoiding the use of irritating substances and unnecessary topical medications;
- lidocaine (2% gel or 5% ointment);
Diet issues for vulvodynia
Some studies indicate that vulvodynia is somehow related to calcium oxalate in the urine. Calcium oxalate is believed to be a strong irritant to the genital skin. Not all researchers have confirmed these data. But whether the genital irritation is caused by calcium oxalate in the urine or simply increased sensitivity to it, the fact is that many women benefit from a low-oxalate diet and daily intake of calcium citrate. Dr. Herzl Melmed, a gynecologist specializing in this area, reports that 70% of his patients experienced significant improvement with such measures. A low oxalate diet should be followed for approximately six months. Rhubarb, celery, chocolate, strawberries and spinach contain a lot of oxalates.
Calcium citrate also reduces oxalate levels. Look for foods without vitamin D on the label; you don't want excess amounts of this substance. The drug Citracal contains 200 mg of calcium and 750 mg of citrate in one tablet. You can take another drug with approximately the same dose, two tablets before meals three times a day. Sometimes this is enough for a Woman to get rid of pain in the genital area and return to normal life.
It is recommended that women suffering from vulvodynia change their diet and start taking a good vitamin and mineral complex in doses recommended by their doctor. Add proanthocyanadins (antioxidant substances found in grape seeds and grape skin, these can be purchased at health food stores) initially at a dose of 2 mg per 1 kg of body weight, this dose should be divided into two to four doses and taken daily for two weeks. Then reduce the dose to maintenance, 20-60 mg per day. Taking vitamins, minerals, and antioxidants improves the functioning of the immune system and helps repair and regenerate cells throughout the body. This is probably why this regimen helps cure vulvodynia.
Psychological aspects of vulvodynia
Like all diseases, vulvodynia has physical, emotional and rational aspects. All of them must be dealt with at the same time, otherwise we will achieve only temporary improvement, and our inner voice will look for an opportunity to convey information and attract attention. Studies of the emotional aspects of Bartholin's gland inflammation, in which these patients were compared with a control group of women with other vulvar diseases, found that women with vulvodynia were more psychologically depressed, had a greater tendency towards sexual dysfunction, and were more preoccupied with their body's reactions, which were generally completely normal. But instead of realizing that these tests are normal, they believe that they have symptoms of serious illnesses. For example, they feel bloated after eating and fear that this is a sign of a serious illness. Small pink spots and other normal changes on the skin lead them to believe it is cancer, or they think their heart is beating in their ears at night, which is a sign of a brain tumor.
As already mentioned, patients with inflammation of the Bartholin gland are more likely to have a history of sexual or physical abuse than women with other vulvar problems. It is a well-documented fact that women who have suffered sexual or physical abuse often have difficulty subsequently establishing normal sexual relationships, so it is not surprising that trouble occurs in the genital area, to which the woman's inner voice wants to draw attention in order to heal it. One way to change the nervous system signal in this area is to activate a biological feedback mechanism. Vaginal biofeedback involves knowing how to relax and re-tighten your pelvic floor muscles, and the exercise has been shown to relieve pain in 83% of women who did it for 16 weeks. Most of these women were able to have sexual intercourse after treatment. Kegel exercises work according to the same mechanism; women can perform them at home. Many therapists are trained and skilled in pelvic floor injury rehabilitation. Those dealing with stress incontinence can also help with this.
Other treatments
Treatment of depression
. Tricyclic antidepressants, such as amitriptyline or desipramine, help some women because of their ability to block the reuptake of the neurotransmitters serotonin and norepinephrine, which can affect the function of the Bartholin glands themselves. Some doctors consider it correct to use antidepressants “to give the nerves a rest.” Newer antidepressants, such as Prozac, have not yet been studied in these conditions.
Treatment was started with the lowest dose, which was increased if necessary and if there were no side effects. Amitriptyline was started at 10 mg every evening for a week, then the dose was increased to 20 mg every evening for another week, then 30 mg for the third week. You will need to work with your doctor to find a dose, but women most often achieve benefits with doses ranging from 30 to 75 mg per day.
Allergy therapy using the Nambudripad (TLAN) method
. Despite the fact that there is still no data on the connection between vulvulitis and allergies, it is known for sure that it is associated with impaired immune response. It may be treatable using the TLAN method described earlier.
Interferon
. Interferon is an antiviral agent that stimulates cells - natural killer cells of the immune system. It may help treat many cases of vulvodynia, although we do not yet understand what mechanism is at work. It is clear that in women with vulvodynia, something is abnormal in the mucosal immune response. Therefore, it is logical to assume that a substance that affects the immunity of the mucous membrane will help treatment. Some researchers believe that interferon only works in women with herpes virus infection. Others believe that He works in all cases.
Interferon is given as an injection into the Bartholin glands three times a week for four to six weeks. Improvements are reported in 40-80% of cases, depending on the selection of patient groups. Although the herpes virus is not known to be the cause of vulvar pain, the success of this treatment is an interesting paradox that has not yet been explained. Interferon has no effect in women who are not infected with the herpes virus.
Surgical methods of treatment
. Surgical excision of the Bartholin glands is successful in some women, but not in all.
After reviewing all the scientific evidence and clinical observations, it is clear that the best treatment for vulvodynia must combine physical, emotional and psychological aspects. The symptom of constant and chronic genital pain requires a lot of faith in your inner wisdom, a lot of empathy and patience.
Signs
The main symptom of vulvodynia is long-lasting pain in the external genitalia. It can be both acute and aching in nature. The pain is localized in the area of the vaginal opening, clitoris, labia minora and/or labia majora. Pain near the anus or perineum is much less common. In some patients, the pain is combined with dryness, itching, a feeling of heat and redness of the vaginal mucosa.
Vulvodynia is characterized by the occurrence or intensification of pain at the moment of even light touching the tissues of the vulvar ring.
Without treatment, vulvodynia becomes chronic and can last over six months.
Common female diseases and their symptoms
6 myths about urinary incontinence in women
Hormonal imbalance in a woman: 7 signs
How is vulvodynia treated?
Treatment for vulvodynia depends on the causes of its development. Some types of genital pain are greatly relieved by the use of yeast infection creams or tablets. Sometimes the pain can be overcome by using creams with estrogen or cortisone, but the latter is contraindicated for use over a long period of time. A number of antidepressants can relieve nerve pain and irritation. Other treatment options include interferon injections, laser therapy, and surgery.
Muscle spasms in the pelvic area can also aggravate genital pain, in which case physical therapy to strengthen and relax the pelvic muscles and clinical monitoring may help. If you decide to try this type of treatment, contact a women's health specialist. Over time, you will learn to relax your pelvic muscles at home with the help of special exercises.
How else can I relieve my symptoms?
The following recommendations will help reduce symptoms. If at least one of them gives results, continue to stick to it. If all attempts are unsuccessful, ask your doctor about alternative treatments.
- Try to avoid soaping the genital area. Limit rinsing with water. Do not use creams, petroleum jelly, foam or bath oil, or intimate deodorants.
- Wash your genitals regularly with clean water to clear any vaginal discharge that could cause irritation. After each urination, use a spray bottle to cleanse.
- Wear only cotton underwear and loose clothing. Avoid tights and other tight-fitting synthetic items.
- Use only unbleached white toilet paper and 100% cotton hygiene products (tampons and cotton pads).
- Report any discharge or irritation to your doctor immediately so fungal and bacterial infections can be quickly diagnosed and treated.
- Avoid using mechanical contraceptives and creams that can irritate the genital area. Talk to your doctor about other methods of contraception.
- Be sure to wash new underwear before wearing it and always rinse thoroughly after each wash to remove any detergent residue.
- Do not stay in a wet swimsuit for a long time, as this will create favorable conditions for the growth of bacteria and fungi in the genital area.