The "IBS" request is redirected here; for the river, see Ibs (river).
| Cardiac ischemia | |
| ICD-10 | 20.-25. |
| ICD-9 | 410410-414414 |
| DiseasesDB | 8695 |
| eMedicine | med/1568 |
| MeSH | D017202 |
Cardiac ischemia
(IHD; lat. morbus ischaemicus cordis, from Greek ἰσχαιμία[1] -
ischaimia
- “ischemia”, from ἴσχω[2][3] -
iskho
- “detain, stop” and αἷμα[4] -
ayma
- “blood” ) is a pathological condition characterized by an absolute or relative disruption of the blood supply to the myocardium due to damage to the coronary arteries[5].
Coronary heart disease is myocardial damage caused by a disorder of the coronary circulation, resulting from an imbalance between coronary blood flow and the metabolic needs of the heart muscle. In other words, the myocardium needs more oxygen than is supplied by the blood. IHD can occur acutely (in the form of myocardial infarction), as well as chronically (recurrent attacks of angina).
Features of the disease
All kinds of fatty and calcium deposits lead to atherosclerosis, thereby preventing oxygen from reaching the heart muscle. People over 45 are most susceptible to the disease. That is why it is important to take vitamins, avoid stress, and eat rationally. Also, many doctors previously believed that this was a more “male” disease, but now they have come to the conclusion that it simply appears later in women than in men.
The danger of the disease is that the patient develops “angina pectoris” (angina pectoris), the likelihood of myocardial infarction increases, and the risk of sudden coronary death is too high.
Read below about the classification of coronary heart diseases of blood vessels (arteries).
The following video will tell you more about coronary heart disease:
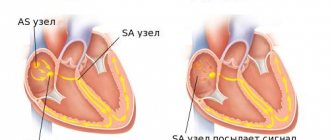
Pathogenesis
Ultrasound diagnostics revealed narrowing of the coronary artery.
The plaque area is marked in green. According to modern concepts [17], coronary heart disease is a pathology based on myocardial damage caused by insufficient blood supply (coronary insufficiency). An imbalance between the actual blood supply to the myocardium and its blood supply needs can occur due to the following circumstances:
- Causes inside the vessel:
- Atherosclerotic narrowing of the lumen of the coronary arteries
- Thrombosis and thromboembolism of the coronary arteries
- Spasm of the coronary arteries
- Causes outside the vessel:
- Tachycardia
- Myocardial hypertrophy
- Arterial hypertension
The concept of IHD is a group one [17]. It unites both acute and chronic conditions, including those considered as independent nosological forms, which are based on ischemia and the changes in the myocardium caused by it (necrosis, dystrophy, sclerosis); but only in cases where ischemia is caused by a narrowing of the lumen of the coronary arteries associated with atherosclerosis, or the reason for the discrepancy between coronary blood flow and the metabolic needs of the myocardium is unknown.
The formation of an atherosclerotic plaque occurs in several stages. At first, the lumen of the vessel does not change significantly. As lipids accumulate in the plaque, ruptures in its fibrous cover occur, which is accompanied by the deposition of platelet aggregates that promote local fibrin deposition. The area where the parietal thrombus is located is covered with newly formed endothelium and protrudes into the lumen of the vessel, narrowing it. Along with lipid fibrous plaques, almost exclusively fibrous stenotic plaques are formed that undergo calcification[17].
As each plaque develops and enlarges, and the number of plaques increases, the degree of stenosis of the lumen of the coronary arteries also increases, which largely (although not necessarily) determines the severity of clinical manifestations and the course of IHD. Narrowing of the artery lumen by up to 50% is often asymptomatic. Typically, clear clinical manifestations of the disease occur when the lumen narrows to 70% or more. The more proximal the stenosis is located, the greater the myocardial mass is exposed to ischemia in accordance with the area of the blood supply. The most severe manifestations of myocardial ischemia are observed with stenosis of the main trunk or mouth of the left coronary artery.
A sharp increase in myocardial oxygen demand, coronary vasospasm or thrombosis can often play a role in the origin of myocardial ischemia. Prerequisites for thrombosis due to damage to the vascular endothelium can arise already in the early stages of the development of an atherosclerotic plaque, especially since in the pathogenesis of IHD, and especially its exacerbation, processes of hemostasis disturbance, primarily platelet activation, the causes of which are not fully established, play a significant role. Platelet microthrombosis and microembolism can aggravate blood flow disturbances in a stenotic vessel.
Significant atherosclerotic damage to the arteries does not always prevent their spasm. A study of serial cross-sections of affected coronary arteries showed that only in 20% of cases an atherosclerotic plaque causes a concentric narrowing of the artery, which prevents functional changes in its lumen. In 80% of cases, an eccentric location of the plaque is detected, in which the vessel’s ability to both expand and spasm is preserved.
Classification
It is generally accepted that coronary heart disease includes:
- Myocardial infarction;
- Pathological heart rhythms;
- Sudden coronary death;
- Angina pectoris;
- Heart failure.
Purpose and measures of secondary prevention of cardiac pathologies
This direction involves reducing cardiac risks in patients with an existing diagnosis. Secondary prevention of CVD is based on taking into account the risk of recurrent cardiovascular events over the next 10 years. Measures applied:
- non-drug correction (nutrition, physical education);
- maintenance drug therapy;
- timely treatment of existing cardiovascular diseases.
Secondary prevention measures are selected by the doctor taking into account current chronic and acute pathologies.
When selecting a drug program, the effect of medications on the patient’s quality and life expectancy is taken into account. Medicines to prevent heart disease:
- statins – Simvastatin, Mertenil, Atomax, Liptonorm;
- fibrates – Bezamidin, Miscleron, Gevilon, Atromidine;
- antithrombic agents/anticoagulants – Heparin, Aspirin, Fragmin, Klivarin;
- beta blockers - Tenzol, Anaprilin, Pindolol, Coronal, Acekor;
- ACE inhibitors – Enalapril, Lisinopril, Captopril, Ramipril;
- potassium and magnesium preparations - Panangin, Asparkam, Doppelhertz Active.
Causes
The formation of plaques is promoted by a lot of reasons, but not all of them will necessarily result in CHD. However, as soon as several of these causes are combined, the risk of the disease increases. Most often, its factors include:
- Increased blood pressure;
- Diabetes;
- Increased cholesterol levels;
- Adverse habits, especially smoking;
- Obesity of varying degrees;
- Frequent stress;
- Sedentary lifestyle.
In addition to this, there are also “human factors”:
- Age (over 45 years old);
- Heredity;
- Gender (controversial factor).
Causes and localization of coronary atherosclerosis
Atherosclerosis of the coronary vessels affects the large trunks of the arteries that carry blood to the myocardium; cholesterol deposits are often located near the mouths. They are often found in the LAD, a little less often - in the circumflex branch. Plaques in the right coronary artery are uncommon. Signs of sclerosis are found in the extramural (superficial) parts of the vessels, while in the intramural parts they remain unaffected. The process is characterized by diffuse damage with varying degrees of narrowing.
The reasons for the development of pathology are increased cholesterol levels and metabolic disorders due to obesity, poor nutrition, and low physical activity. People with a hereditary predisposition and addiction to smoking are at risk. This deviation is often observed in men over 45 and women over 55 years of age.
Atherosclerosis does not develop as a local pathology; usually all vessels are affected. Lack of treatment results in heart attack, stroke, development of heart and brain failure, disability and death of the patient.
Symptoms of coronary heart disease
If we are talking about a latent form of the disease, when there are no symptoms of the problem, then such a condition can last for several years, or even decades. The development of CHD begins even in adolescence under a combination of circumstances and the presence of risk factors.
The main symptom of CGD can be considered pain, a feeling of tightness in the chest during tension, as well as chronic pain in the “engine”, which manifests itself even with mild physical activity. For example, when a person bends down to zip up a shoe, or slowly climbs the stairs, he may feel pain radiating to his left arm and jaw, and it becomes difficult for him to breathe.
The disease may also be accompanied by the following symptoms:
- dyspnea;
- sweating;
- increased heart rate;
- nausea;
- fear and panic.
Anterior interventricular branch
The anterior interventricular branch is located in the anterior interventricular groove and goes to the apex, giving off the anterior ventricular branches (diagonal artery, D) and anterior septal branches along the way. In 90% of cases, one to three diagonal branches are determined. The septal branches depart from the anterior interventricular artery at an angle of approximately 90 degrees and pierce the interventricular septum, feeding it. The anterior interventricular branch sometimes enters the thickness of the myocardium and again lies in the groove and along it often reaches the apex of the heart, where in approximately 78% of people it turns posteriorly onto the diaphragmatic surface of the heart and at a short distance (10-15 mm) rises upward along the posterior interventricular groove. In such cases, it forms the posterior ascending branch. Here it often anastomoses with the terminal branches of the posterior interventricular artery, a branch of the right coronary artery.
Treatment
There is no cure for CHD, but its control is quite possible if you lead a healthy lifestyle and take certain medications.
Therapeutic method
- First of all, the doctor will instruct the patient to forget about bad habits, because smoking plays a major role in the development of the disease.
- Patients with excess body weight are advised to use special diets and a balanced diet - everything must be done to ensure that the weight returns to normal.
- The doctor will also recommend methods for correcting high levels of cholesterol, blood pressure and blood sugar.
Thus, therapeutic treatment is reduced to eliminating the negative influence of risk factors.
Medication method
Having understood the risk factors, it is worth starting to fight the symptoms of CAD and aim at improving blood flow. Therefore, the patient may be prescribed:
- Acetylsalicylic acid to reduce agglutination of blood cells;
- Calcium antagonists to activate bioenergetic processes, enhance cellular metabolic processes, reduce blood pressure;
- Nitroglycerin and similar drugs necessary to expand the lumens in blood vessels;
- Lovastatin, provastatin and the like to lower blood cholesterol levels;
- Beta-adrenergic receptor blockers, which will help reduce the blood's need for oxygen.
Surgery and other therapies
- If the first two treatment methods are ineffective, the doctor may refer the patient for coronary artery bypass surgery. The essence of such an intervention is that a different path is created for blood flow to the place of lack of oxygen in the heart (not through the area of narrowing of the artery). To pave this path, special shunts are used, created from fragments of other human arteries and veins. The mechanism is as follows: such an artery from another place joins one end to the aorta, and the other to the coronary artery. Most often, the internal mammary artery is used for such manipulations.
- Transluminal percutaneous coronary (“balloon”) angioplasty is also used as an alternative to such surgical intervention. The following mechanism operates here: a deflated air balloon is placed into the coronary artery in the area of the affected area, after which it is inflated, thereby destroying the plaque. As a result, proper blood flow is restored.
Diagnostics
To prevent acute conditions in the later stages of the disease, you must immediately consult a doctor and diagnose atherosclerosis. Its purpose is:
- confirmation or refutation of damage to the vascular wall;
- clarification of the localization and extent of the process;
- assessment of the functional state of ischemic tissues.
Laboratory methods
Using laboratory tests you can:
- determine the progression of pathology;
- evaluate the effectiveness of treatment.
This is done by measuring the levels of cholesterol, lipids and triglycerides in the blood. The complete and detailed picture that can be obtained regarding the content of these substances in plasma is called a lipid profile. Particular attention should be paid to low-density cholesterol (LDL). It is its concentration that is considered atherogenic. Increased triglycerides are also a health threat. Elevated levels of high-density lipoprotein (HDL) indicate a low risk of plaque formation in the vascular intima.
For the diagnosis of atherosclerosis, the determination of the atherogenicity coefficient is of great importance. It is calculated simply. The resulting number of HDL is subtracted from the total amount of cholesterol and divided by LDL. The normal value ranges from 3 to 5, and exceeding the value indicates the risk of developing atherosclerosis.
Instrumental
The gold standard for diagnosing myocardial ischemia is angiography. This far from new method still allows me and my colleagues to clearly determine the cause of pain in the heart during an attack or rhythm disturbance. The introduction of a contrast agent and observation of its distribution in the coronary vessels makes it possible to accurately identify the location of occlusion. This type of research helps to establish an accurate diagnosis and determine the method of treatment. Its disadvantage is its high invasiveness and the need for careful preparation.
Computed tomography using a contrast agent allows you to obtain a three-dimensional image of the affected vessel and assess the condition of the part of the heart that is undergoing changes. MRI makes it possible to examine the pathology in volumetric form and in high quality, without requiring the use of additional drug administration. But this study cannot be carried out if there is a pacemaker or other metallic inclusions in the body.
Features of stenosing coronary sclerosis
When using various methods, atherosclerosis of the coronary artery with stenosis can be determined by the following signs:
- a pronounced decrease in blood flow speed in the affected area;
- the presence of a plaque that covers the lumen by 50% or more of normal;
- changes in the myocardium in the area of the narrowed coronary artery.
Prevention
The first rule of prevention: stop smoking! It is smoking that most often leads to such undesirable consequences as coronary heart disease.
- A proper daily routine will help not only self-discipline, but also good health of all organs;
- Strong physical activity, for example, long walks in the fresh air, morning exercises, etc.
- A rational, balanced diet based on reducing the consumption of cholesterol-containing products and increased consumption of vegetables and fruits is also necessary;
- And don’t forget to take vitamins, as well as such important “heart minerals” as: Potassium, which not only regulates the water balance in our body, but also normalizes the heart rhythm, helps eliminate toxins and lowers blood pressure;
- Magnesium, which is responsible for the proper functioning of most organs.
The right psychological attitude is no less important: avoid stress, spend more time with loved ones.
Circumflex artery
The circumflex branch of the left coronary artery is located in the left part of the coronary sulcus and in 38% of cases gives the first branch to the artery of the sinoatrial node, and then the obtuse marginal artery (obtuse marginal branch, OMB), usually from one to three. These fundamentally important arteries supply the free wall of the left ventricle. In the case when there is a right type of blood supply, the circumflex branch gradually becomes thinner, giving off branches to the left ventricle. In the relatively rare left type (10% of cases), it reaches the level of the posterior interventricular groove and forms the posterior interventricular branch. In an even rarer case, the so-called mixed type, there are two posterior ventricular branches of the right coronary and circumflex arteries. The left circumflex artery forms important atrial branches, which include the left atrial circumflex artery (LAC) and the large anastomosing artery of the appendage. The branches of the left coronary artery vascularize the left atrium, the entire anterior and most of the posterior wall of the left ventricle, part of the anterior wall of the right ventricle, the anterior 2/3 of the interventricular septum and the anterior papillary muscle of the left ventricle.
Complications
- Atherosclerosis of the cerebral arteries can cause vascular dementia and stroke.
- When a plaque ruptures, a blood clot forms, interfering with the normal movement of blood through the artery, and this can lead to a heart attack and, accordingly, death of the heart muscle.
- Sudden coronary death can also occur as a result of this disease.
- Rhythm disturbances are also possible
- There is a high risk of heart muscle weakness.
Development of the disease
With careful attention to one's own health, a person can detect the first symptoms of atherosclerosis of the coronary arteries long before old age. This, according to experts, is the norm, especially considering the lifestyle of modern people. It predisposes to the earlier appearance of massive cholesterol plaques in the vessels supplying the heart muscle.
In its development, the disease goes through several stages, each of which can last decades:
- The initial to clinical stage is accompanied by a slight deposition of cholesterol in the form of a fatty spot on the walls of blood vessels. This usually occurs where the intima of the artery is damaged. Over time, the lipoprotein spot transforms into longitudinal or transverse stripes, the thickness of which does not exceed several microns. There are no clinical signs of atherosclerosis of the coronary vessels at this stage.
- The second clinical stage of atherosclerosis of the heart vessels is accompanied by the proliferation of lipid deposits. Due to an increase in their thickness, a decrease in blood supply to the heart is noticeable, especially if the patient is in a state of activity. At this stage, fibrin fibers and red blood cells join the cholesterol plaques, and a fairly large blood clot can form. Experts call this process multifocal atherosclerosis of the coronary arteries, which is often complicated by blood clot rupture and death. The symptoms at this stage are already quite pronounced: palpitations and shortness of breath during physical exertion appear, and arrhythmia is observed.
- The third and final stage of atherosclerosis of the coronary and coronary vessels is accompanied by thickening of the plaque due to the addition of calcium to it. At the same time, the lumen of the arteries narrows significantly, the walls of the arteries are deformed, becoming less elastic and dense. The condition is accompanied by sharp pain under the sternum during exercise of any intensity, arrhythmia, periodic heart attacks, and general weakness.
Despite the fact that modern medicine has extensive capabilities to eliminate atherosclerosis, treatment is more effective when the disease is detected in the initial stages.
Forecast
If you follow your doctor’s advice and take preventive measures in time, there is a high probability of preventing CHD. If it leads to a heart attack or sudden coronary death, then the probability of death is too high.
Even if a heart attack does not become a fatal diagnosis for coronary artery disease, after it, coronary heart disease will begin to progress faster. Also, patients with CAD are more likely than others to end up in the hospital with a stroke and ailments that arise from blockage of the arteries.
Even more useful information on the issue of coronary artery disease is contained in this video:
Coronary arteries
From an anatomical point of view, the coronary artery system is divided into two parts - right and left. From a surgical perspective, the coronary bed is divided into four parts: the left main coronary artery (trunk), the left anterior descending artery or anterior interventricular branch (LAD) and its branches, the left circumflex coronary artery (OC) and its branches, the right coronary artery (RCA). ) and its branches. The large coronary arteries form an arterial ring and loop around the heart. The left circumflex and right coronary arteries participate in the formation of the arterial ring, passing along the atrioventricular groove. The formation of the arterial loop of the heart involves the anterior descending artery from the left coronary artery system and the posterior descending artery from the right coronary artery system, or from the left coronary artery system - from the left circumflex artery with a left dominant type of blood supply. The arterial ring and loop are a functional device for the development of collateral circulation of the heart.