Decompression sickness is a complex of symptoms that forms when gas bubbles form in blood vessels and tissues against the background of a rapid decrease in atmospheric pressure. Pathology can be acute or chronic. It manifests itself as pain in the joints, muscles, Meniere's syndrome, dyspepsia, signs of central nervous system damage, acute pulmonary and cardiovascular failure. When making a diagnosis, anamnestic data and the results of an objective examination are used; radiography, ultrasound, MRI, and CT are used to assess the condition of various organs. Treatment is recompression followed by slow decompression, symptomatic drug therapy.
Caisson disease
Decompression sickness (decompression sickness, DCS) is a complex of changes that develop during the transition from high atmospheric pressure to normal, and less often - from normal to low. The pathology got its name from the word “caisson”, meaning a chamber created in the 40s of the 19th century and intended for work under water or in water-saturated soil conditions. DCS is considered an occupational disease of submariners and specialists working in caisson chambers; in some cases it is diagnosed in pilots. In recent years, due to the widespread prevalence of diving, it has been identified in other groups of the population. According to statistics, the incidence of the disease is 2-4 cases per 10,000 dives.
Causes
The immediate cause of decompression sickness is a rapid decrease in atmospheric pressure when the depth of immersion in water changes, and less often when the aircraft rises to a significant altitude. The faster the atmospheric pressure changes, the greater the risk of this pathology. Factors that increase the likelihood of developing the disease are:
- Aging of the body . As we age, the condition of all organs deteriorates. This causes a decrease in the compensatory capabilities of the lungs and heart during the period of pressure changes.
- Hypothermia . Accompanied by a slowdown in blood flow in peripheral vessels. Blood from distant parts of the body enters the pulmonary vessels more slowly, and gas is released from the blood physiologically to a lesser extent.
- Dehydration . In this condition, blood viscosity increases, which causes a slowdown in blood circulation. When external pressure changes, stasis occurs in the periphery, which is aggravated by the formation of bubbles blocking the lumen of blood vessels.
- Exercise stress . It potentiates a violation of the uniformity of blood flow, as a result of which conditions are created for the intensive dissolution of gases in the blood with the subsequent appearance of “quiet” bubbles. A characteristic feature is the deposition of microbubbles in the joints and an increased likelihood of pathology occurring during subsequent dives.
- Lipidemia, excess weight. Fats are highly hydrophobic, so when their content is high, bubbles form more actively. Cells of adipose tissue intensively dissolve inert gases that are part of respiratory mixtures.
- Hypercapnia . Develops when the quality of the respiratory mixture is low or attempts are made to “save” it by holding one’s breath. An increase in the amount of CO2 provokes a shift in the acid-base state to the acidic side. Because of this, more inert gases dissolve in the blood.
- Alcohol intoxication. When drinking alcohol, dehydration occurs. In addition, alcohol molecules cause small bubbles to join into larger ones and become centers around which large bubbles form, blocking blood vessels.
Prevention measures
Caisson disease develops when certain conditions are created. The main condition for its prevention is to prevent prolonged exposure to high blood pressure, that is, its normalization. It is also worth considering that flights after deep-sea diving are contraindicated, as they can aggravate the manifestations of the disease.
To prevent a diver from getting decompression sickness, he needs to make periodic decompression stops. Non-stop diving is only possible for a short period and at a shallow depth. When ascending, stops are made near the surface to prevent the development of decompression sickness and normalize the concentration of gases in the blood. Their duration and other features are determined using special tables or more modern computer methods.
Compliance with the rules allows you to at least alleviate the symptoms, even if, due to certain factors, decompression sickness still overtakes the person. Unfortunately, the variability of independent environmental factors is so great that even computer calculations are not always reliable.
To avoid becoming a victim of acute decompression, you must follow instructions when diving at depth, and also avoid pressure changes in other situations. Additionally, good health, lack of excess weight and overwork will help reduce risks.
Symptoms usually appear 1-2 hours after rising from depth. However, they may appear during the process or after 6-12 hours. Although this happens quite rarely.
Depending on the manifestations, there are three forms of decompression sickness - mild, moderate and severe.
Mild (cutaneous) form
Decompression sickness manifests itself as redness, rash and itching, sometimes swelling or red and white spots, the so-called marbling pattern. Slight pain in bones, muscles and joints is possible.
Medium form
Decompression sickness manifests itself as a disruption of the musculoskeletal system, with the legs and shoulder girdle most often affected, and less commonly the wrists, hands, elbows, and feet. First, unpleasant sensations arise in the affected organ, then it goes numb, then it begins to hurt. The pain is constant and aching. Disturbances in the functioning of the inner ear also occur - nausea, hearing loss. This condition is called Meniere's syndrome or ear decompression disease. Gastrointestinal manifestations of decompression sickness - abdominal pain and frequent bowel movements - are also characteristic of this stage. Visual acuity decreases, pupils are dilated.
In severe form
Decompression sickness affects vital organs. Paresis and paralysis of the muscles of the arms and legs, muscles of the rectum and bladder develop. The lungs and heart are affected, this is manifested by shortness of breath, cough, chest pain, and bluish skin. The functioning of the inner ear is disrupted - headaches, dizziness, nausea, and tinnitus develop. It usually develops at great depths. The pressure drops, hypoxia and loss of consciousness are possible.
These forms can be independent, or they can transform into one another. Moreover, a mild form can very quickly turn into a severe one.
Description
On land, you need to ensure the patient is calm and warm, check his pulse and breathing. If the patient is conscious, it is better to lay him horizontally on a flat surface so that his arms and legs do not become numb.
If he is unconscious, he is placed on his left side, with his right leg bent for stability. This is done so that if the patient vomits, vomit does not enter the respiratory tract. If necessary, you need to give him an indirect cardiac massage and artificial respiration, if there is a person around who knows how to do this.
Afterwards, you need to provide the patient with breathing pure oxygen. This creates conditions for the transport of nitrogen from tissues to the lungs. For this purpose, special cylinders with compressed oxygen are used.
Diagnostics
The diagnosis is made based on the clinical picture and medical history. The x-ray shows air bubbles in the blood vessels, joint cavities, and synovial tendon sheaths.
Treatment
The only treatment for decompression sickness is therapeutic recompression. It should be carried out immediately after the first signs of decompression sickness appear. At the same time, conditions are created in a special chamber under which the pressure increases, gas bubbles dissolve and blood circulation is restored.
Further treatment is aimed at eliminating paresis and paralysis resulting from decompression sickness, improving blood circulation and restoring the functions of the pelvic organs.
Death from decompression sickness is now quite rare. However, victims often remain paralyzed.
Prevention
To prevent decompression sickness, only people in very good health are accepted to work in compressed air conditions. They regularly undergo medical examinations, lead a healthy lifestyle and limit themselves to alcohol and cigarettes. Divers and those who work at depth must know and strictly follow safety rules when diving and ascending.
Those who have suffered decompression sickness are not allowed to go deep if they:
- have not fully recovered;
- the disease was severe, recovery from it was very long;
- decompression sickness occurred more than once;
- have symptoms of neurological disorders identified during examination.
Doctor Peter
Decompression sickness
is a complex of pathological changes that develop as a result of the formation of persistent gas bubbles in the human body.
The essence of the physical processes of formation of gas bubbles in the human body is as follows.
The human body consists of 80% water, so it has physical laws characteristic of water and gases. At normal atmospheric pressure, about 1 liter of nitrogen is dissolved in the blood and tissues of the body. When the excess water pressure increases by 1 kgf/cm2, another 1 liter of nitrogen dissolves in the body, i.e. there will be 2 liters of nitrogen in it, and so on. The amount of indifferent gas dissolving in the tissues of the body is directly proportional to the partial pressure of the gas in the inhaled gas mixture and depends on the time spent under elevated pressure. It is believed that almost complete saturation of body tissues with nitrogen occurs after 5-6 hours of exposure to pressure.
Nitrogen dissolves most in adipose tissue; saturation and desaturation in it occur slowly, because this tissue is poorly supplied with a circulatory network. The blood quickly becomes saturated and desaturated with nitrogen and is therefore its carrier.
With a slow decrease in external pressure, excess dissolved nitrogen is removed from the body through the blood and lungs by diffusion. With a sufficiently rapid decrease in external pressure, i.e., when the decompression regime is violated, excess dissolved nitrogen does not have time to be removed from the body and then gas bubbles form. They clog blood vessels and compress tissue, causing pathological changes in the body.
The body is able to retain an excess amount of physically dissolved nitrogen 1.2 liters and release it through the lungs without forming bubbles in the tissues. This value is called the coefficient of safe, permissible supersaturation of body tissues with nitrogen. This saturation of the body with nitrogen occurs at a depth of 12 m when breathing compressed air, and when breathing 25% oxygen mixtures - at a depth of 20 meters. Consequently, a safe ascent to the surface without decompression modes is possible when breathing compressed air from a depth of 12 m, and when breathing a 25% nitrogen-helium-oxygen mixture from a depth of 20 m.
So, the main cause of decompression sickness is the formation of gas bubbles in the blood and tissues of the body when the decompression regime is violated.
Causes of decompression sickness in ISP
1. Incorrectly developed decompression mode when leaving a sunken submarine.
2. Exceeding the maximum permissible time spent under high pressure.
3. Failure to comply with time delays at stops (the body does not have time to desaturate) when exiting on a break.
4. Lack or low supply of oxygen to the breathing bag (the submariner forgot to open the valve of the oxygen cylinder).
Decompression sickness can also occur with a rapid decrease in pressure in emergency compartments without taking into account the time spent under increased pressure.
The development of decompression sickness is promoted by low ambient temperature, physical activity, and the content of the respiratory mixture of carbon dioxide more than 1%.
SIGNS
There are three forms of decompression sickness: mild, moderate and severe.
1. The mild form is characterized by such symptoms as skin itching, rash, pain in bones, joints, muscles and along the nerve trunks, which do not cause much suffering to the patient.
2. The moderate form of the disease is characterized by severe pain in muscles, bones, joints, causing severe suffering to the patient; skin rash, “marbled” coloration of the skin. Severe abdominal pain may occur, accompanied by bloating, nausea and vomiting; general weakness, circulatory and respiratory disorders, rapid pulse, weak filling, shortness of breath.
3. Severe form. The previously described symptoms become more severe, and they are accompanied by damage to the central nervous system in the form of cuts and paralysis of the limbs and internal organs, hearing and vision disorders, and loss of consciousness.
Much less frequently, and, as a rule, when descending to great depths, dizziness, nausea, vomiting, nystagmus of the eyeballs and severe muscle weakness (Meniere's syndrome) may be observed.
The sooner signs of illness develop after leaving the water or high blood pressure, the more severe it is.
FIRST AID.
Each diver and submariner, if signs of decompression sickness appear or if health deteriorates during the ascent to the surface, or after leaving the water (chamber), is obliged to immediately report this, and the persons in charge (department commander, chief diver, diving specialist, doctor) are obliged to immediately begin providing assistance to the sick person and carrying out therapeutic recompression.
Treatment of decompression sickness is carried out in accordance with the instructions and the therapeutic recompression table. When the pressure increases again, the gas bubbles decrease in size, dissolve, and the painful symptoms disappear.
Carrying out therapeutic recompression is mandatory in all cases of decompression illnesses. The sooner recompression is started, the faster and more effective its results will be.
Preventing decompression sickness
1. Correct use of decompression tables.
2. Selecting the desired exit mode from the sunken submarine depending on the submersion depth of the submarine and the time spent under the highest pressure.
3. Strict adherence to the exit mode according to the buoy (shutter speed and speed of movement).
4. Proper activation of breathing in the IDA (open the oxygen cylinder after equalizing the pressure).
Caisson sickness (decompression sickness, DCS, caisson, divers' sickness) is a disease caused by a person's rapid transition from an environment with high pressure to an environment with normal pressure. This is accompanied by the release of nitrogen bubbles from physiological fluids, dissolved in it at high pressure. Most often, the disease is observed in divers who violate the rules for deep-sea work (ascending too quickly or staying at depth for a long time).
Source: likar.info
The first cases of caisson disease began to be recorded after 1841, when the caisson was invented - a special chamber for construction work under water (fastening bridge supports, building underwater tunnels). The workers entered this chamber through the airlock, where they carried out the necessary work. To prevent flooding of the caisson, compressed air was supplied to it. After the work shift ended, the pressure was reduced to atmospheric pressure. At the same time, many workers experienced severe joint pain, and some developed paralysis and even death.
Pathogenesis
At elevated pressure, the gases of the respiratory mixture, due to diffusion, dissolve in significant quantities in the blood of the capillaries of the lung tissue. When the pressure decreases, the opposite phenomenon is observed - gases “come out” of the liquid, forming bubbles. The faster the pressure changes, the more intense the process of reverse diffusion becomes. With a rapid rise, the patient’s blood “boils”, the released gases form many large bubbles, which can block vessels of various sizes and damage various organs.
Large bubbles connect with small ones, platelets “stick” to the resulting bubbles, and blood clots form, attaching to the walls of small vessels and blocking their lumen. Some of the blood clots break off with fragments of the vascular wall, migrate along the bloodstream and block other vessels. When a large number of such formations accumulate, a gas embolism develops. With significant damage to the walls, the integrity of the arterioles is disrupted and hemorrhages occur.
The appearance of bubbles and the formation of their complexes with platelets triggers a cascade of biochemical reactions, as a result of which various mediators are released into the blood, and intravascular coagulation occurs. Bubbles also form outside the vascular bed, in articular cavities and soft tissue structures. They increase in volume and compress the nerve endings, causing pain. Pressure on soft tissue formations causes their damage with the formation of foci of necrosis in muscles, tendons and internal organs.
Physics and physiology of DCS[ | ]
When you inhale, air enters the bronchi and reaches the alveoli, the smallest structural unit of the lungs. It is here that the process of gas exchange between the blood and the external environment occurs, when the hemoglobin contained in the blood takes on the role of a carrier of oxygen molecules throughout our body.
Nitrogen contained in the air is not absorbed by the body, but always exists in it, in a dissolved - “quiet” - form, without causing any harm. Nitrogen begins to behave completely differently when it comes to underwater diving.
The amount of gas dissolved in a liquid directly depends on the gas pressure at the surface of that liquid. If this pressure exceeds the gas pressure in the liquid itself, then a gradient of gas diffusion into the liquid is created - the process of saturation of the liquid with gas begins.
This process continues until the gas pressure in the liquid equals the gas pressure at the surface of the liquid. When the external pressure decreases, the reverse process occurs. The gas pressure in the liquid exceeds the external gas pressure on the surface of the liquid, and a process of “desaturation” occurs.
(30 m / 10 m/atm.) 1 atm. = 4 atm.
that is, four times greater than the pressure on land. In this case, the amount of nitrogen dissolved in the body increases over time and, ultimately, also exceeds the amount of dissolved nitrogen on the surface of the water by four times.
Upon ascent, with a decrease in external (hydrostatic) water pressure, the pressure of the gas mixture that the submariner breathes also begins to decrease. The amount of nitrogen consumed by the submariner, or rather its partial pressure, also decreases.
Because of this, a supersaturation of the blood with nitrogen begins to occur, as a result of which it begins to be slowly released in the form of microbubbles. There is a “desaturation” of the blood, which at the same time seems to “boil”. A reverse gradient of gas diffusion from the liquid is created.
When the ascent process is slow, the partial pressure of nitrogen in the breathing mixture also decreases slowly - relative to the diver’s breathing. Nitrogen microbubbles from the blood begin to be released and, together with the blood flow, move into the heart, and from there into the lungs, where they, again, exit through the walls of the alveoli when exhaling.
If the submariner begins to ascend too quickly, then the nitrogen bubbles simply do not have time to reach the lungs and leave the body. The submariner’s blood “boils.” Thus, more and more dissolved nitrogen is added to the bubbles, which creates a snowball effect.
Then platelets are attached to the bubbles, followed by other blood cells. This is how local blood clots (thrombi) are formed, making it unevenly viscous and can even clog small vessels.
Meanwhile, the bubbles attached to the inner walls of the vessels partially destroy them and tear off along with their pieces, complementing the “barricades” in the bloodstream. A breakthrough in the walls of blood vessels leads to hemorrhage into the surrounding tissues, blood flow slows down, and the blood supply to vital organs is disrupted.
The extravascular form of DCS occurs when microbubbles formed in tissues, joints and tendons attract nitrogen released from the tissues during ascent, but cannot enter the blood due to its blockage (the so-called.
DETAILS: What should be the pulse of a healthy 10-year-old child
"bottleneck effect"). Hydrophilic tissues of joints and ligaments are especially susceptible to the accumulation of extravascular nitrogen bubbles. It is this type of DCS that causes joint pain - a classic symptom of decompression sickness.
Mechanical blockage of blood flow by nitrogen bubbles is not the only effect of decompression sickness. The presence of bubbles and their connection with blood cells leads to biochemical reactions that stimulate blood clotting directly in the vessels, the release of histamines and specific proteins into the blood.
Selective removal of complementary proteins from the blood eliminates many of the devastating consequences of DCS. Recent research has shown that the binding of blisters to white blood cells causes severe vascular inflammation.
To prevent the occurrence of DCS, one should, first of all, control the ascent process, which, according to modern ideas, should not exceed 18 meters per minute. The slower the submariner ascends, the slower the surrounding pressure decreases, the fewer bubbles form in his blood.
Moreover, in the practice of scuba diving there are so-called decompression stops. Their essence lies in the fact that the submariner, rising from depth to the surface, stops at a certain depth, which is obviously less than the diving depth, for, again, a certain time, which is calculated either from tables or using a dive computer.
This stop (or even several gradual stops) can last for a fairly long period of time, depending directly on how much the submariner has exceeded the no-decompression limit of the dive, and, accordingly, on how much nitrogen his body is saturated with.
During such stops, the body “desaturates” and gas bubbles are removed from it. Excess nitrogen is removed from the body, and the blood does not boil, as if a swimmer had surfaced without any stop.
Often at such stops, the submariner breathes a gas mixture different from the “bottom” one. In such a mixture (stage, from English parking) the percentage of nitrogen is reduced, and therefore decompression occurs faster.
Of course, complete saturation of all body tissues with nitrogen does not occur immediately; this takes time. To calculate the maximum time spent at the “bottom” depth, without the risk of DCS, there are special decompression tables, which have recently begun to be replaced everywhere by dive computers.
Using these tables, you can approximately find out the time a submariner will spend at a given depth while breathing a given gas mixture, which will be safe from a health point of view. The word “approximately” is not accidental here.
Data on being at a certain depth for different people can vary within very wide limits. There are certain risk groups whose dive time may be significantly shorter than others.
For example, a severely dehydrated human body is much more susceptible to DCS, which is why all divers drink plenty of fluids before and immediately after diving. Decompression tables and dive computers initially contain a certain margin of “strength”, focusing on the minimum possible dive time, after which there is already a risk of DCS.
Cold and physical exertion during diving also contribute to the onset of DCS. Blood circulates more slowly in a frozen part of the body and is much less susceptible to removing excess nitrogen from it and adjacent tissues.
One option to reduce the risk of DCS is also to use breathing mixtures other than air. The most common version of this mixture is nitrox - oxygen-enriched air.
In nitrox, compared to simple air, the percentage of oxygen is increased and the nitrogen content is reduced. Since nitrox contains less nitrogen, the time spent at a given depth may be longer than the time spent at the same depth using air.
Or you can stay underwater for the same amount of time as using air, but at a greater depth. Due to the lower nitrogen content in nitrox, the body is less saturated with it. When diving with nitrox, you need to use decompression tables other than “air” ones or special computer modes.
Since nitrox contains more oxygen than air, another danger arises - oxygen poisoning. The maximum depth to which you can dive without the risk of oxygen poisoning depends on the grade of nitrox (the percentage of oxygen in it).
Classification
Due to the possibility of damage to various organs, significant differences in severity and prognosis, the most rational, from a practical point of view, is considered to be the most rational, from a practical point of view, to systematize the types of decompression sickness based on the predominant manifestations. The clinical classification of M. I. Yakobson is a detailed version of distinguishing the degrees of the disease, taking into account symptoms. There are four forms of pathology:
- Easy . Arthralgia, myalgia, and neuralgia, caused by compression of nerve endings by gas bubbles, predominate. A number of patients experience livedo, itching, and greasiness of the skin caused by blockage of small superficial veins, ducts of the sebaceous and sweat glands.
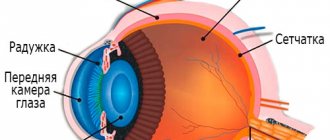
- Moderate weight . Disorders of the vestibular apparatus, eyes and gastrointestinal tract predominate, resulting from embolism of the capillaries and arterioles of the labyrinth, accumulation of gas bubbles in the vessels of the mesentery and intestines, transient spasm of the retinal arteries.
- Heavy . It manifests itself as rapidly increasing symptoms of damage to the spinal cord, as a rule, at the level of the mid-thoracic segments, which is due to the tendency of myelin to absorb nitrogen and weak vascularization of the mid-thoracic region, due to which actively forming bubbles do not migrate with the blood, but compress the nervous tissue. Signs of brain involvement are much less common. Cardiac and respiratory disorders are possible.
- Lethal. Occurs when there is a total cessation of blood circulation in the lungs or medulla oblongata, and the development of acute heart failure. It is provoked by the formation of a large number of large bubbles, simultaneously blocking many vessels.
To assess the threat to the patient’s life and determine the optimal treatment tactics in traumatology and orthopedics, a simplified classification is also used, including two types of acute DCS. The first type is characterized by damage to peripheral structures (skin, muscular-articular system). The second is accompanied by changes in the nervous, respiratory, cardiovascular, and digestive systems; if left untreated, death is possible. In addition, there is a chronic variant of decompression sickness, which can develop in the presence of a history of acute pathology or without previous acute phenomena; diagnosed in people who worked for a long time in caisson conditions.
Symptoms of decompression sickness
In the case of severe damage, manifestations may occur already in the first minutes after ascent, but more often the clinical picture of decompression sickness develops gradually. In half of the patients, symptoms are detected within an hour. After 6 hours, signs of pathology are detected in 90% of patients. Rarely there is a delayed onset of symptoms (within 1-2 days). In mild forms, there is pain in the joints, bone structures, muscle tissue, and back area. The pain syndrome is usually more pronounced in the area of the shoulder and elbow joints. Patients describe the sensation as “boring”, “deep”, and intensifying with movement. A rash, itchy skin, increased greasiness, and marbling of the skin color are often noted. Possible enlarged lymph nodes.
In moderate decompression sickness, Meniere's syndrome is observed, which is caused by damage to the balance organ and includes dizziness, headache, pallor, sweating, nausea, and vomiting. Disorders of the gastrointestinal tract are manifested by pain, vomiting and diarrhea. Retinal vascular spasm is accompanied by the appearance of photomorphopsia, “floaters” and “fog” before the eyes. The severe form is characterized by lower spastic paraplegia, pelvic disorders, and sensory disturbances in the lower half of the body according to the conduction type. Sometimes hemiparesis or hemiplegia, headaches, speech disorders, and psychotic disorders of a transient nature are observed.
Cardiovascular and respiratory symptoms are detected in severe forms and reach their greatest severity in the lethal variant of the disease. Weakness, pallor, shortness of breath, intense chest pain, cough, and a drop in blood pressure are detected. As symptoms progress, pulmonary edema develops, breathing becomes frequent and shallow, the pulse slows down, and the skin becomes bluish or pale gray. Pulmonary and myocardial infarctions are possible. The lethal form is accompanied by acute heart failure, asphyxia due to blockade of pulmonary circulation or impaired regulation of breathing by the medulla oblongata.
The most common manifestation of chronic decompression sickness is deforming arthrosis, caused by repeated exposure of small bubbles to osteoarticular structures. Scientists' opinions regarding cardiac myodegeneration, early atherosclerosis and frequent middle ear diseases in people engaged in caisson work differ. Some experts consider the listed pathologies to be a consequence of repeated subclinical DCS, others - the result of the influence of other factors that arise when staying at great depths.
Symptoms
- Pressure in the ears, dizziness.
- Joint pain.
- Skin rashes, itching.
- Fatigue, shortness of breath.
- Weakness and/or lack of sensation in the limbs,
- Bleeding from the ears and nose.
- Drowsiness to the point of loss of consciousness.
- Paralysis.
Symptoms of decompression sickness vary from joint pain in the first 24 hours after getting up to loss of consciousness immediately after getting up. What ailments will appear depends on the depth of the dive and the speed of ascent.
Diagnostics
The acute form of decompression sickness is diagnosed based on the patient’s complaints, anamnestic data and the results of an external examination. X-rays may reveal gas bubbles in joints, muscle tissue, fascia, and tendon sheaths. To determine the state of the central nervous system, tomographic studies of the spinal cord and brain are prescribed. The diagnosis is confirmed by improvement of the patient's condition during recompression. The examination program for the development of complications is determined by the nature of the suspected pathology and may include ECG, echocardiography, radiography, ultrasound, MRI and CT of various organs.
Treatment
Once the disease is confirmed, therapy should be started as soon as possible. Any delay may result in dangerous consequences or death. In the initial stages, the disorder is eliminated by inhaling oxygen through a mask. For more severe cases, treatment in a pressure chamber is necessary. In this device, the pressure first gradually increases and then decreases. This action causes gas bubbles in the blood to dissolve.
Treatment in a pressure chamber
Drug therapy is aimed at reducing pain and stimulating the cardiovascular system. It is also used as a preventive measure and to eliminate complications. For this purpose, painkillers, substances that strengthen the immune system, and anti-inflammatory medications are prescribed. Physiotherapy methods can be used, in particular water or dry air baths. With timely treatment, in almost all cases it is possible to completely eliminate decompression sickness.
Treatment of decompression sickness
Treatment of the disease, depending on the form and severity of symptoms of complications, is carried out by resuscitators, traumatologists, occupational pathologists and other specialists. For mildly expressed skin, muscle and joint manifestations, dynamic observation is acceptable. In other cases, urgent recompression in a pressure chamber is indicated. First, the pressure is increased to levels corresponding to the depth of the patient’s immersion. In case of a serious condition of the victim, pressure higher than the initial one is used. The minimum duration of recompression is 30 minutes; if symptoms persist, the procedure is continued until the patient’s condition normalizes. Then slow decompression is carried out, reducing the pressure by 0.1 atmosphere every 10 minutes. After reducing the pressure to 2 atmospheres, inhalation of oxygen is used to accelerate the process of nitrogen removal. If signs of DCS appear after normalization of pressure, repeat recompression is performed.
According to indications, symptomatic therapy is prescribed. Carry out infusions of glucose solution, plasma, saline solutions. Pharmaceuticals are used to normalize and stimulate the activity of the cardiovascular system. If necessary, vasodilators are included in the treatment plan. For intense pain, non-narcotic analgesics are used. Narcotic pharmaceuticals are not indicated due to a possible inhibitory effect on the respiratory center. For myalgia and arthralgia, local warming and painkillers are recommended. After leaving the pressure chamber, physiotherapy is performed: solux, diathermy, medicinal baths.
Decompression sickness
Decompression sickness (or decompression sickness) is an occupational disease, mainly of submariners and divers, associated with the release of inhaled gas (oxygen, nitrogen and hydrogen) into the blood in the form of bubbles due to a sharp decrease in pressure. This is an extremely dangerous condition and often leads to paralysis and death.
Other Therapy: Hernia Dyspareunia
Causes
As is known from physics, the higher the pressure, the better the gas dissolves in the liquid and, conversely, as the pressure decreases, the gas dissolves less well. This process is the main cause of decompression sickness. When a person is under conditions of sharply decreasing pressure (for example, a diver rises to the surface from a great depth), undissolved gas from his lungs is released into the blood and other body fluids in the form of bubbles, which injure blood vessels, and sometimes cause rupture of the vessel wall or gas embolism. In addition, these bubbles can penetrate tissues and joints, causing serious damage to nerve endings, internal organs and joints.
Additional factors that increase the risk of developing decompression sickness are: hypothermia, dehydration, physical activity under conditions of high blood pressure, alcohol consumption and excess weight.
Symptoms of decompression sickness
Symptoms of decompression sickness vary depending on the severity of the condition. Mild severity is characterized by mild pain in joints and bones, aching muscle pain, general weakness and skin rash (accompanied by itching). It is also possible to experience paresthesia and mild numbness, increased heart rate and increased breathing. In the more severe stage of decompression illness, immediately after the end of the decompression period, clumsiness of movements, loss of coordination, severe nausea and cold sweat occur. The pain in the joints and bones is much worse. In some cases, loss of consciousness is possible. At the most severe stage of decompression sickness, there is a high risk of developing paralysis and other serious disorders of the central nervous system. Choking, cyanosis, collapse and chest pain may also occur.
Diagnostics
Diagnosis of decompression sickness is usually made on the basis of the clinical picture of the disease and a carefully collected medical history. It is important to establish the fact that the patient is in conditions of pressure drop - whether diving under water or flying on an airplane. Using an X-ray examination, you can identify gas bubbles in blood vessels, tissues and joints, as well as assess the degree of damage to internal organs and the body as a whole. Computed tomography and magnetic resonance imaging are used to detect changes in the spinal cord and brain.
Classification
Depending on the location of damage and changes in the body, there are two main types of decompression sickness:
• Type I decompression sickness is generally characterized by mild symptoms and involvement of the joints, muscles and bones. The main symptoms of this type of decompression sickness are joint pain, lymphadenopathy and skin manifestations.
• Type II decompression sickness is much more severe and dangerous. It affects the circulatory system, the brain and spinal cord, as well as the respiratory system. It is characterized by severe symptoms and serious disorders in the body, including paralysis and death.
Patient Actions
If you suspect decompression sickness, it is recommended to immediately call an ambulance and wait for its arrival with minimal movements, being in a horizontal position if possible.
Treatment of decompression sickness
Treatment of decompression sickness is aimed, first of all, at removing gas bubbles from tissues and vessels. For this, the patient is subjected to recompression by being placed in a pressure chamber. Under high pressure, the bubbles dissolve on their own, normalizing the patient’s condition. Next, doctors analyze and diagnose the damage caused to the body and, if necessary, prescribe symptomatic therapy.
Complications
Lack of timely treatment for decompression sickness can lead to serious consequences for the body and some diseases. Depending on the location of gas bubbles, the development of osteoarthritis, aeropathic myelosis, acute heart failure, acute respiratory failure, and optic neuritis is possible.
Prevention of decompression sickness
To prevent decompression sickness when ascending from depth, it is recommended to ascend to the surface according to the rules, observing the decompression time, no less than the prescribed period. It is also recommended to use special breathing mixtures (with a high oxygen content) for breathing underwater at great depths.
Prognosis and prevention
The outcome of DCS is determined by the severity of the lesion and the time of onset of recompression. 80% of patients experience complete recovery. Fatal outcomes are observed quite rarely, usually due to emergency ascent or lack of specialized care. Prevention of decompression sickness includes the use of high-quality diving equipment and professional work at depth, strict adherence to lifting rules taking into account data from specially developed tables, regular medical examinations, and the elimination of factors that increase the risk of DCS. Preventive measures also involve establishing a sufficient time interval between the first and subsequent dives or flights by air, limiting the time spent in high-pressure conditions for divers and caisson workers.
| Literature1. Occupational diseases: Diagnosis, treatment, prevention / Skepyan N.A. – 20132. Occupational diseases/ Artamonova V.G., Shatalov N.N. – 19883. Decompression sickness / Shitov A. – 2011 | ICD-10T70.3 code |
VKontakte
LiveJournal