Breast abscess
- a limited inflammatory focus in the thickness of the soft tissue of the mammary gland, which is an encapsulated purulent cavity. The disease develops and occurs acutely, with a significant increase in temperature and symptoms of intoxication, intense pain, redness and swelling of the breast, purulent discharge from the nipple. In diagnosis, anamnesis and complaints, objective examination and additional research methods (ultrasound of the breast, radiography, bacteriological culture of breast discharge) are important. Treatment of a breast abscess is only surgical (opening the abscess) with the parallel prescription of antibiotics.
Breast abscess
Breast abscess is always a secondary pathology, which is a complication of a previously occurring disease of the mammary gland (hematoma, mastitis and other purulent-inflammatory processes). The disease is more common in women, developing in 2% of cases in nursing mothers, but can also affect men, adolescents and newborns. Breast abscess associated with lactation occurs during the first six weeks after birth. In newborns, purulent formations of the mammary glands develop at the age of 1-1.5 months. The abscess, as a rule, forms on one side; bilateral abscesses are diagnosed extremely rarely, usually in infants.
Symptoms
Basically, the disease begins with an increase in body temperature. The girl/woman develops a fever. The affected gland becomes extremely painful, the mother can no longer feed the baby with a sore breast. The lobes of the gland closest to the source of infection become denser and enlarged.
Inflammation begins to spread to other areas of the chest. The skin over them becomes red and swollen, and then a visible abscess forms, which is called an abscess.
Pathological forms of breast abscess:
- superficial (accumulation of pus occurs in the subcutaneous tissue of the parapapillary region)
- intramammary (an abscess forms against the background of congestive mastitis; isolated areas of necrosis (death) can form, and in severe cases, the abscess breaks through and its contents flow out)
- retromammary (the back of the mammary gland suppurates; pus is able to break through the fiber between the organ and the outer pectoral fascia and flow out)
Inflammation at any stage causes an increase in body temperature in the patient, and only after the abscess breaks out, a decrease in temperature closer to normal values is sometimes observed.
Causes of breast abscess
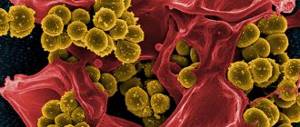
The disease is caused by the penetration of pathogenic bacteria (staphylococci, streptococci, Proteus, Escherichia coli or their associations) into the breast tissue. Melting of gland tissue with the formation of an encysted abscess occurs due to the following diseases:
- Mastitis
. Occurs as a result of stagnation of milk in the breast. Inflammation of the mammary gland leads to the active proliferation of bacteria in its tissues, which in 6–11% results in abscess formation. - Chest injury
. A bruise of the mammary gland is often accompanied by the formation of a hematoma. If left untreated, the hematoma festeres and encapsulates. - Galactophorite
. This is an inflammation of the milk ducts, the most common cause of which is trauma to the mammary gland. The disease belongs to non-lactation mastitis. - Cyst or benign tumor
. The growths put pressure on the milk ducts, causing them to become blocked. As a result of the addition of a secondary infection, an encysted purulent formation occurs. - Hormonal disbalance
. Hormonal disorders provoke stagnation of lymph and blood in the mammary glands, which activates the proliferation of pathogenic microflora. Hormone imbalance is observed in mastopathy, during the neonatal period and in various endocrine pathologies. - Purulent-inflammatory diseases
. The cause of a breast abscess can be the following diseases: furunculosis, axillary lymphadenitis, pyoderma, carbuncle. Pathogenic microbes penetrate the tissues of the mammary glands by hematogenous route, causing an inflammatory process in them, followed by the formation of an abscess.
There are a number of predisposing factors, the presence of which increases the risk of developing the disease. These include weakened immunity, lactostasis, cracked nipples, smoking, endocrine diseases. Carrying out invasive medical procedures (ductography, minor surgical interventions on the chest), nipple piercing with non-compliance with aseptic conditions can contribute to the penetration of infection.
Causes
Breast abscess (ICD 10 code - No. 60-64) develops mainly in women. In rare cases, suppuration of breast tissue occurs in men and children. In newborns, the pathology occurs in the first month of life.
The development of the disease is facilitated by infection of the mammary gland by pathogenic microorganisms. Most often this happens after infection:
- staphylococci;
- Proteus;
- streptococci;
- coli.
The possibility of developing an abscess after infection cannot be ruled out:
- tuberculosis;
- Pseudomonas aeruginosa;
- pneumococci;
- syphilis;
- pathogenic fungi (actinomycetes);
- Brucella and other microorganisms.
Infection does not always cause suppuration of the mammary glands. Concomitant pathologies lead to the development of an abscess:
- Mastitis. The disease occurs against the background of stagnation of milk during breastfeeding, which causes inflammation of local tissues and a decrease in local immunity. This contributes to the addition of a secondary infection.
- Injuries. Due to mechanical damage, hematomas form in the problem area, which fester over time.
- Galactophorite. The disease is characterized by inflammation of the milk ducts. Galactophoritis mainly occurs after chest injuries.
- Benign neoplasms (including cysts). Tumors compress the milk ducts, causing stagnation of fluid in the chest.
- Hormonal imbalance. Because of this disorder, lymphatic fluid and blood stagnate in the breast, resulting in the activation of pathogenic microorganisms. Hormonal imbalance occurs due to pregnancy, endocrine and a number of other pathologies.
Other diseases and neoplasms, the development of which is accompanied by tissue suppuration, also lead to breast abscess:
- carbuncle;
- furunculosis;
- lymphadenitis localized in the armpits;
- pyoderma.
In these pathologies, pathogenic agents spread throughout the body along with the bloodstream and are localized in the mammary glands, causing inflammation and suppuration.
Breast infections are caused by cracked nipples, a weakened immune system, and smoking. Infection also occurs due to the lack of antiseptic treatment of the mammary glands during minimally invasive procedures.
Pathogenesis
The entry point for infection is often the nipple or its damaged areola. In some cases, infectious agents enter the mammary gland through the bloodstream from other purulent formations. Bacteria spread through the milk ducts into the tissues of the gland and begin to actively multiply, releasing toxins and decay products, which leads to the development of intoxication syndrome. Inflammatory edema that occurs in the walls of the mammary ducts is the result of an immune response to the action of bacterial antigens and causes microcirculation disorders. The permeability of the vascular wall increases, intercellular fluid enters the lumen of the milk ducts, and their blockage occurs. Lactostasis aggravates the inflammatory process in the milk ducts, which spreads to surrounding tissues. Subsequently, the inflamed tissues melt, they are separated from healthy ones by a dense capsule and the formation of a cavity containing pus.
Risk factors
Such factors do not in themselves lead to the appearance of an abscess, but indirectly increase the risk of its development in the event of infection. These include:
- Weakening of local and/or systemic immunity;
- Poor breast emptying (refusal of breastfeeding due to mastitis, insufficient expression of excess milk, etc.);
- Closure of the lumen of the milk ducts by polyps or tumors, desquamated epithelium, scar tissue;
- Diabetes. When it occurs, microcirculation of blood in the tissues of the gland is disrupted, which makes it difficult for the immune system to eliminate the pathogen. In addition, in diabetes, the composition of milk deviates from normal, which normally prevents the development of bacteria.
- Smoking;
- Piercing. The presence of foreign bodies in the mammary gland creates additional entry points for infection.
Classification
In mammology, the generally accepted classification of breast abscesses is used. Systematization of purulent formations of the mammary gland is carried out according to their location, the number of ulcers, damage to one or both glands. Depending on the location, there are:
- Subcutaneous abscess
. It is located superficially and is easily diagnosed due to the translucency of the pus. - Subareolar abscess
. Located under the nipple and its areola. More common in lactating women. - Intramammary abscess
. Located in the thickness of the glandular tissue of the chest. - Retromammary abscess
. Located between the retromammary fatty tissue and the pectoral muscles. The most dangerous form of the disease, which poses a high risk of purulent melting of the muscles and an abscess breaking into the chest cavity.
Depending on the involvement of one or both mammary glands in the pathological process, unilateral and bilateral abscesses are distinguished. Based on the number of abscesses in one gland, abscesses are divided into single and multiple.
Symptoms of a breast abscess
The disease begins acutely, with a rise in temperature to 38–39°C. In the case of a previous chest injury, signs of a formed purulent formation appear on days 3–5. Patients are concerned about sharp, throbbing pain in the mammary gland, redness of the skin over the purulent focus, and its pain on palpation. The pain in the gland intensifies when shaking in a car, walking and jumping. By palpating the gland, you can accurately identify the epicenter of pain. The mammary gland swells, purulent discharge may appear from the nipple, often with blood clots. The axillary lymph nodes on the affected side are enlarged and painful on palpation. To local symptoms are added general signs of intoxication: nausea and vomiting, weakness, adynamia, lack of appetite, increased heart rate.
The leading symptoms depend on the location of the abscess. With a subareolar location of the purulent formation, an enlargement of the nipple and its areola occurs due to edema. A dense and painful formation is palpated under the isola. When an intramammary abscess is located at a shallow depth, there is a dense and hyperemic area at the site of its localization. In the case of a deep abscess, there are no external changes in the mammary gland. If a retromammary abscess has formed, the gland rises and takes on the appearance of a hemisphere directed forward and upward.
Complications
Lack of timely treatment leads to abscess breakthrough and the development of complications. If the purulent formation is superficial, there is a high probability of fistula formation. It is also possible to develop phlegmon of the mammary gland, a breakthrough of the abscess into the milk ducts, followed by the release of milk mixed with pus and blood clots. Long-term purulent inflammation in the milk ducts destroys their walls and causes metaplasia (degeneration) of epithelial cells, which is fraught with the formation of malignant processes. The most dangerous complication of a breast abscess is the development of sepsis, in which bacteria are spread throughout the body through the bloodstream, which leads to the formation of new multiple purulent foci in different organs and tissues.
Why does a breast abscess occur?
The disease occurs when bacteria gets inside the breast tissue. Basically, this is staphylococcus, streptococcus or a combination of them, but there may also be a complex of Staphylococcus aureus and Proteus or Escherichia coli.
The pathogen enters the organ usually through the nipple. Thus, an abscess during breastfeeding occurs when the baby is incorrectly applied to the breast; with an irregularly shaped nipple, when the baby is forced to injure the nipple with his gums, which leads to the formation of cracks; with excessive rubbing of the area around the nipple with a washcloth or removal of hair near the areola.
The last two reasons can serve as a convenient place for infection to enter outside the period of lactation, when dirt from hands and underwear gets into open wounds on the skin of the chest.
In the postpartum period, it is “convenient” for an abscess to develop in the area where milk stagnation has occurred, or due to blockage of the milk ducts, cysts have formed in their deeper parts.
The reasons for this include refusal to breastfeed, situations where a woman does not empty the milk sinuses and ducts (does not express milk from there), as well as underdevelopment of the nipples and diseases of the child himself, which is why the baby sucks very little milk. A large volume of the mammary gland will contribute to the formation of a purulent cavity, when its lower parts descend strongly downward, and milk is poorly excreted from them.
The rest of the time, including during pregnancy, an excellent substrate is a hematoma (even of minimal size), formed deep in the gland tissue as a result of injury. Mastitis, followed by a breast abscess, develops if bacteria penetrate the soft tissue of the breast from internal organs affected by a bacterial infection - aggressive and not receiving adequate treatment.
An abscess develops more often if an infection has entered the mammary gland due to conditions such as:
- decreased general immunity: after childbirth, due to a viral infection or taking drugs that suppress the immune system;
- hypothermia of the soft tissues of the chest;
- severe stress;
- exacerbation of osteochondrosis or acute disease of the spine in the thoracic region, due to which the mammary gland does not receive sufficient nervous regulation;
- breast tumors of benign and malignant course;
- hormonal disorders.
In men, mammary gland abscesses occur as a result of injury, the entry of bacteria from infected organs into the gland, as well as hormonal imbalance, due to which there is more estrogen in a man’s body than male hormones.
The latter situation may arise due to diseases of the adrenal glands, testicles, pituitary gland or hypothalamus. But it can be caused by the accumulation of adipose tissue - a source of estrogen - due to drinking large amounts of alcoholic beverages, taking drugs such as Ranitidine, Famotidine, Captopril, drinking anabolic steroids without sufficient physical training. False gynecomastia, that is, breast enlargement in a man due to adipose tissue, can occur due to obesity or diabetes.
Diagnostics
A breast abscess is diagnosed by a mammologist or surgeon. The doctor ascertains the medical history, clarifies the connection of the disease with lactation, decreased immunity or injury, examines the mammary gland and identifies characteristic signs of purulent formation: skin hyperemia, soreness and fluctuation of a certain area of the gland, enlarged axillary lymph nodes. Laboratory and instrumental research methods are also used in the diagnosis of breast abscesses:
- Clinical tests
. In the peripheral blood, leukocytosis with a shift to the left, accelerated ESR (signs of inflammation) are detected; proteinuria and leukocyturia are possible in the urine. - Bacteriological culture of breast secretions
. The discharge from the nipple or the contents of the abscess obtained by puncture are examined, the pathogen and its sensitivity to antibiotics are determined. - Ultrasound of the breast
. The location, size, depth of location and number of ulcers, their communication with the milk ducts and with each other are specified. - Mammography
. Helps determine the shape and size of a purulent formation, its approximate location and carry out a differential diagnosis with non-inflammatory breast diseases. - CT scan of the breast
. Indispensable in case of unsatisfactory results of mammography and ultrasound, in the presence of a retromammary abscess and in the differential diagnosis of purulent formation with other pathologies of the mammary gland.
Differential diagnosis of breast abscess is carried out with phlegmon, hematoma, fibroadenoma, breast carcinoma, fat necrosis and a number of other diseases. For this purpose, a cytogram of discharge from the nipple, puncture of the formation and analysis of the punctate, biopsy of the suspicious area followed by histological examination are performed.
Treatment of the disease
The main treatment for a breast abscess is emergency surgery. It must be carried out in a surgical hospital, after hospitalization. The operation consists of opening the purulent cavity under general anesthesia, clearing it of its contents, and rinsing it with antiseptics.
Surgeons make an incision going from the nipple to the periphery of the gland, along its radius. They examine the affected gland, looking for possible messages for pus. Next, you need to connect the natural and pathological passages into one cavity, destroying the bridges between them with a blunt instrument. Carefully cauterize and bandage all bleeding vessels to avoid the formation of a hematoma in the postoperative period.
The operation ends with drainage of the cavity and the application of loose sutures that will not tighten the swollen tissue of the gland, thereby increasing inflammation. The woman is left under observation for 1-3 days, during which the surgeon examines the gland and rinses the cavity cleared of pus with antiseptics to avoid recurrence of the infection.
Only when the swelling subsides and any contents cease to be released through the drainage, the surgical wound is sutured “tightly” and the patient can be discharged home. Dressings will need to be performed daily, then recovery will occur within 3-4 weeks. During this period, you cannot warm your breasts, perform physical activity, or feed the baby.
After the abscess has been removed, antibiotic therapy is prescribed. It includes broad spectrum antibiotics: Ceftazidime, Ceftriaxone, Gentamicin, Cefuroxime.
Local treatment
A breast abscess takes many days to form, but it needs to be opened only when it is fully “ripe.” Then it will be possible to cleanse the tissues of pus, which will be visible visually. If you do not open an unformed breast abscess (when pyogenic microbes have already colonized the fatty tissue of the gland, but have not yet caused its melting), and start using a complex of rational antibacterial and local therapy, you can avoid surgery.
For local treatment, heparin ointment is recommended. It thins the blood at the site of application, which will improve the nutrition of the affected area of the gland and cleanse it of pyogenic flora (necessarily during long-term antibacterial therapy). In addition, the ointment has antimicrobial and anti-inflammatory activity, promoting additional effects on pyogenic microorganisms. One disadvantage: it cannot be used during pregnancy.
While waiting for the child, in addition to antibacterial therapy and surgery, treatment with folk remedies can be carried out (its possibility is agreed with the attending surgeon).
The following recipes can be used:
- Onion compress. There are 2 main ways to use this plant. In the first one, grate a fresh juicy onion on a fine grater, apply the pulp to the sore spot, keeping it there for 5 hours and replacing it with a new one. The second recipe is to use a baked onion. To do this, the onions are baked, ground into a paste, and then mixed with an equal amount of grated laundry soap. This compress is applied for 3 hours, twice a day.
- Honey ointment. It is prepared from equal parts of honey, 70% alcohol and Vishnevsky ointment. Immediately after mixing, the ointment is ready to be applied to the skin for 12 hours. After this, the breasts are washed and a new portion of honey ointment is applied to the painful area.
- Aloe juice compress. Take one of the lower leaves of the plant, wash it with soap, and grind it into a paste. It must be applied to the abscess, secured with a gauze bandage. Change the compress every 12 hours.
After acute inflammation subsides (at the healing stage), proper massage of the gland and a course of physiotherapy procedures are required, which will accelerate tissue regeneration.
If you consult a doctor in time, when the first symptoms appear, and then carefully follow all his recommendations, it is possible to completely cure the abscess and preserve the appearance and functionality of the mammary gland.
Treatment of breast abscess
The basis of treatment for a formed abscess is emergency surgery - opening the abscess and draining it. Incisions are made from the center (nipple areola) to the periphery (base of the gland). In some situations, it is more appropriate to make an incision in the fold under the mammary gland. The wound is examined, all detected ulcers are opened and combined into one cavity, the pus is removed and the wound is washed with an antiseptic solution. Then drainage is installed and the wound is partially sutured. The drainage is left in the wound for 3–4 days, until the discharge stops, after which the wound is sutured tightly. It is possible to puncture aspiration of pus from the abscess and introduce an antibiotic solution into its cavity. Such an intervention is low-traumatic and does not leave a scar after healing, but is not effective enough. The puncture is performed only if there is a small single abscess.
In parallel with surgical intervention, antibiotics are prescribed according to the sensitivity of the isolated pathogens (penicillins, cephalosporins, fluoroquinolones), and infusion therapy is carried out for the purpose of detoxification. Also indicated is the use of NSAIDs, which eliminate pain, reduce temperature and reduce signs of inflammation. In order to stimulate the immune system, it is recommended to take immunomodulators.
Treatment
Elimination of a breast abscess can only be achieved surgically. To do this, the patient is prepared for opening and draining the purulent cavity.
The location of the incision during surgery to remove an abscess is determined by the clinical case. Sometimes it is carried out from the center of the nipple to the base of the breast, and in other cases it is carried out under the fold at the base of the breast.
After gaining access to the abscess cavity, the surgeon examines the wound and opens the identified cavities. If there are several of them, then to improve drainage of the abscess, the cavities are combined into one. The tissues formed and cleared of pus are washed with antiseptic solutions. Next, a drainage tube is installed into the cavity for washing and administering medications in the postoperative period. This device remains in the wound for 3-4 days, and after the release of exudate stops, it is removed. After installing the drainage tube, the surgeon sutured the tissue layer-by-layer in the surgical field and applied a sterile dressing.
In some cases, a minimally invasive technique can be used to remove an abscess, which involves aspiration to remove purulent contents. This method can only be performed if there is a single small purulent cavity. In other cases, the effectiveness of the final result of this operation is not enough to completely eliminate the purulent-inflammatory process, and the abscess may recur.
After the operation, antibiotics or antibacterial drugs, non-steroidal anti-inflammatory drugs and the administration of infusion detoxifying solutions are prescribed. At the same time, dressings and care of the drainage tube are performed.
In order to eliminate the causative agent of the purulent-inflammatory process, penicillins, cephalosporins and fluoroquinolones can be prescribed. Pain relief and reduction of inflammation is achieved by taking non-steroidal anti-inflammatory drugs. To stabilize the immune system, immunomodulators are prescribed.
After the stitches are removed and in the absence of complications, the woman is discharged from the hospital. She is advised to follow a gentle regimen until the suture is completely healed and a date is set for a follow-up examination with a mammologist.
Prognosis and prevention
With timely consultation with a doctor and adequate treatment, the prognosis is favorable. The function of the mammary gland is completely restored, there are no consequences other than a scar. Prevention of breast abscess during lactation consists of following the rules of breastfeeding: full pumping of the mammary glands, taking air baths for the breasts, washing the glands before and after feeding, preventing and promptly treating cracked nipples, changing your bra daily. General preventive measures include a healthy diet, adherence to a daily routine and rest, identification and correction of endocrine disorders, giving up bad habits and nipple piercing, strengthening the immune system.