Tooth extraction is one of the most unpleasant medical procedures a person has to face. Even if no pain is felt during the removal itself due to the anesthetic, then after the freezing stops working, the pain may not subside for several days in a row. Sometimes the reason for this is an inflammatory process that develops in the wound left after tooth extraction (alveolitis).
After tooth extraction, alveolitis begins due to bacteria and other pathogenic microorganisms entering the socket. Sometimes this leads to infection of the tissues located next to the tooth socket. The disease develops in almost 90% of cases after the removal of wisdom teeth or molars.
Features of hole healing
The risk of dangerous complications arises when, after tooth extraction, the hole was not properly treated or the patient did not follow the recommendations of the attending physician. Osteomyelitis can develop from inflammation - this is a complication that leads to jaw abscesses and phlegmon. For sepsis to occur, which often ends in death, it is enough for infection to enter the blood during the spread of osteomyelitis.
When the tooth extraction procedure is carried out correctly, blood immediately begins to flow from the socket. After a blood clot forms within 30 minutes, the fluid flow stops. At the same time, the clot protects the wound from environmental influences and various infections.
The clot can change its color from red to yellow within 2-3 days and this will not be a sign of pathology. The change in shade occurs against the background of normal physiological processes, the essence of which is the replacement of red blood cells with a fibrin framework - the basis of the structure of the blood clot, which prevents bleeding.
This wound healing occurs almost painlessly. In this case, the principle of secondary intention operates, the meaning of which is to bring the edges of the wound closer together. Fibroblasts are the main factor ensuring tissue healing. Over time, they are replaced by young osteoblasts.
Normally, the healing process lasts 7 days. During this period, granulocytes are completely replaced by young bone tissue. The duration of complete restoration of the gums will depend on the type and location of the surgical intervention. If the wound size is larger than usual or the intervention in the oral tissues was too rough, the duration of the wound healing process will increase. In most cases, these types of wounds should heal within the first 2-3 weeks. Complete replacement of alveolar granulocytes with young bone tissue occurs within 2–3 months.
Appearance of a normal socket after a few weeks
Who is to blame is not a simple question
The development of this complication does not necessarily occur if the doctor ignores the prescribed rules for tooth extraction.
The tooth to be removed can be technically complex: located in a hard-to-reach place, having an anomaly in the roots or additional, excess roots. And, despite the high level of development of modern surgical dentistry, the occurrence of extraordinary situations that require the highest skill from the doctor when extracting a tooth from the gum is still possible.
An equally important role is played by the need for emergency removal when purulent-destructive changes develop in the tooth, gum or jaw. Changes leading to fragility of the walls of the socket are already pathological.
It may also be caused by a process common to the entire organism, leading to increased fragility of the alveolar walls:
- cancer or other debilitating disease (AIDS, tuberculosis, systemic damage to connective tissue, blood disease, diabetes mellitus);
- exacerbation of a chronic disease, either an acute disease , or the presence of foci of dormant chronic infection in nearby areas, which leads to a weakening of the protective capabilities of oral tissues.
Dentist's responsibility
The dentist is responsible if a broken-off fragment of a tooth root or a fragment of the socket wall is left in the socket without noticing - the presence of a foreign body in the socket after tooth extraction leads to non-healing of the wound and its inflammation and alveolitis. Leaving a successfully removed tooth in the socket of a dental cyst or granuloma also leads to the same result.
Another mistake is not maintaining the time required for the formation of a blood clot in the socket - the doctor must make sure that it is filled with blood, the clot has formed, and only after that perform tamponing; a dry socket will certainly cause an inflammatory process.
In the case of a purulent process that has caused the need for tooth extraction, the doctor must prescribe a program of antiseptic treatment of the oral cavity after the operation and monitor its implementation.
Patient's guilt
The patient undergoing the procedure bears no less responsibility for the development of dental alveolitis.
Excessive nervousness due to a “defect” that has arisen in the mouth with endless looking in the mirror at the “affected” area of the gums with restless unconscious touching of the wound with fingers and tongue. Or the use of various available home remedies out of a desire to heal the wound as quickly as possible.
Excessive zeal when rinsing the mouth, leading to rinsing out the blood clot, which serves as the basis for the formation of scar tissue here in the future. All this, as well as ignoring the doctor’s recommendations for caring for the oral cavity, can lead to additional damage to the gum mucosa and cause inflammation and infection of deeper tissues. Down to bone tissue.
A serious complication, even after a successfully performed extraction, is the lack of formation of a blood clot in the alveolus, blocking access to the tissues of the pathogenic flora. A patient who has not informed the dentist that he suffers from a blood clotting disorder or that he is taking anticoagulants unknowingly creates an additional risk of developing alveolitis in the postoperative period.
Symptoms and causes of inflammation
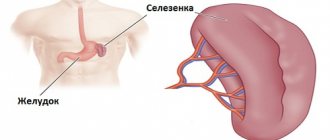
If inflammation is present on the roots of the teeth, it becomes isolated and a cyst may form. These membranes contain pus and infection.
During and after tooth extraction, bacteria accumulate. If bacteria accumulate near or inside the postoperative hole, primary wound infection occurs.
It is impossible to completely kill bacteria. Therefore, the infection can and should be controlled. Particular attention is paid to the patient’s immunity.
Bacteria can enter the body from the external environment. This will be called secondary wound infection.
Alveolitis after wisdom tooth removal can occur under the following conditions:
- A dry socket after extraction can allow bacteria from the mouth to enter the wound. This pathology develops if the correct blood clot has not formed.
- When aseptic objects penetrate into the tooth socket.
- If the patient evades the direct instructions of the attending physician.
Dentists distinguish the following types of pathology:
- Alveolitis of a serous nature is manifested by increased pain during eating. With this pathology, the general condition of the body is normal, no increase in body temperature is observed. When examining the oral cavity, the doctor notices that there is no blood clot in the socket or it is not sufficiently formed. There may be food debris at the site of damage. This form of pathology develops in the first days after the procedure. If it is not noticed within a week, it can develop into more serious diseases.
- Alveolitis of a purulent nature is manifested by a putrid odor from the oral cavity, a significant increase in body temperature, general increasing weakness, and intense pain in the gum area. The patient cannot eat, his face is swollen, and his lymph nodes are enlarged. During examination, a pink-gray coating is noted in the oral cavity.
- Chronic purulent alveolitis of a tooth is manifested by a decrease in the intensity of the clinical picture, characteristic of a purulent form. The patient returns to a “conditional norm.” A growth of soft tissue forms around the damaged socket, which can be seen when examining the oral cavity. Slit-like wounds may occur. At the same time, pus is released from the hole. The mucous membrane takes on a blue tint.
In patients who have had a tooth removed, suppuration may occur within 2 days after surgery. Gradually increasing pain and persistent swelling of the gums are alarming symptoms that can provoke a further deterioration in the patient’s general condition.
The video explains the reasons for the appearance of alveolitis after tooth extraction:
Types of alveolitis
Alveolitis is divided into several main types:
- Serous. The pain is constant and intensifies during chewing; Dry socket syndrome may occur. There may be no other symptoms besides pain at all, the lymph nodes remain in a healthy state, and the body temperature is not elevated. This form of the disease can last up to a week without changing symptoms, and then passes into the next stage.
- Purulent. The infection develops, and in addition to the pain in the area of the extracted tooth, a general state of malaise is added - fever, chills, weakness, headache. The affected area of the jaw swells, causing the face to become asymmetrical. You can see pus in the wound, and a putrid smell comes from your mouth. On palpation, the pain in the walls of the socket intensifies, thickening and inflammation of the processes of the alveoli on both sides is observed.
- Hypertrophic. At this stage, most symptoms subside and the disease enters the chronic stage. Lymph nodes and body temperature return to normal. Particles of dead flesh appear between the soft tissue and the jaw bone, the soft tissue becomes bluish, and pus oozes from the wound.
Separately, it is worth highlighting a deadly disease - toxic fibrosing alveolitis. Despite the similarity of names, it develops in the alveoli of the lungs and occurs due to exposure to toxic substances, such as certain medications, on the body.
First aid at home
If the symptoms described above occur, but it is not possible to consult a dentist, you can alleviate the patient’s condition at home. With the help of special compresses and solutions for rinsing the mouth, the intensity of pain is reduced, but the disease itself is not treated.
You cannot use hydrogen peroxide with baking soda. Rinsing the mouth with this product can provoke general inflammation of the mucous membrane. Effective natural antiseptics include tinctures and decoctions of chamomile and sage. There are certain rules for using such tools:
- To avoid washing out the blood clot, frequent and vigorous rinsing of the mouth is prohibited. To ensure a therapeutic effect, it is enough to keep the decoction in the mouth for 2 minutes.
- If there is an unpleasant odor from the mouth, sucking or picking out the clot using improvised means is prohibited.
- Until the condition improves, it is recommended to do oral baths 10–12 times a day. This schedule should be followed until the affected area is disinfected.
Before consulting a doctor, a strong analgesic may be used. Such medications only relieve pain, but do not eliminate inflammation. Some drugs in this group are recommended to be taken as prescribed by a doctor (Corsodil, Eludril). You can apply Metrogyl Denta gel or a special Solcoseryl paste to the gums.
Read also: Extracted tooth hurts
After providing first aid, it is recommended to make an appointment with a dentist. Before treatment, the doctor makes sure that the purulent process has not become chronic. Physiotherapeutic procedures are used for therapy:
- microwave treatment;
- gel and neon laser therapy;
- Ural Federal District;
- fluctuarization.
Physiotherapy is widely used in dentistry, including in the treatment of alveolitis
In advanced cases, surgical treatment is prescribed. If necessary, the jaw is examined before surgery to determine the extent of inflammation and the location of pus. If there is no need for surgical treatment, the dentist recommends other treatment methods to the patient.
You may also be interested in:
Patient reviews. Works of doctors Video about the clinic
Sign up for a consultation
three ROOTT specialists + diagnostics as a gift
All specialists Our specialists
Doctors from the ROOTT Center have extensive experience in recognizing absolutely any dental disease. Among other things, alveolitis is successfully diagnosed here, from which the patient gets rid of it in our clinic in literally 3-4 visits to a specialist.
Bogatyrev Adam Albertovich
Orthopedic dentist
Borovkova Ella Viktorovna
orthodontist
Professional treatment
To establish the correct diagnosis, dental surgeons check two factors that indicate the occurrence of alveolitis:
- the presence of pus in the socket and its release upon palpation;
- the presence of residues after the disintegration of a blood clot.
Professional treatment of alveolitis after tooth extraction consists of several stages:
- administration of anesthesia;
- thorough cleaning of the extracted tooth socket;
- re-opening the hole with a scalpel;
- it is possible to apply a gauze bandage with active drugs and apply sutures;
- At the end of the appointment, the patient receives recommendations on how to properly treat the wound using antiseptic drugs, ointments and gels.
In the video, a dentist talks about how various complications are treated after tooth extraction:
An outdated method of treating alveolitis is the placement of medications into the cavity of the socket. This therapy is widely used in public institutions.
Alveolitis is a serious complication with a clear manifestation of unpleasant symptoms. But it can be avoided if you follow your doctor's recommendations. For quick treatment and healing of a wound, it is necessary to protect it from the influence of the external environment. Mechanical interventions cannot be performed without the help of a specialist.
The video simulates the process of alveolitis occurrence and its treatment:
During the first 24 hours after the procedure, it is not recommended to chew food on the side where the tooth was removed. Such measures are taken to preserve the integrity of the blood clot. If there are seams on the hole, it is prohibited to act on them in any way. A dry socket after wisdom tooth removal needs more careful care, since purulent processes in this area are more dangerous.
Prevention
Preventive measures that will help prevent the development of alveolitis during successful tooth extraction should be carried out by the patient himself. That is, he must carefully follow the doctor’s recommendations.
In order for the healing process of the hole to proceed normally, you should not pick at the wound, scrape the gum without permission, squeeze out a blood clot, suck it out or damage it in any way. It is especially important not to chew food on the side of the jaw where the tooth was removed for at least a few days, so that the blood clot is preserved.
The dentist, for his part, can prevent the development of complications by observing the rules of asepsis and antisepsis, as well as performing the operation in accordance with the rules of removal technique. The formation of a blood clot by squeezing the edges of the socket is also a prerequisite for successful wound healing.
(Visited 6,568 times, 1 visits today)
Alveolitis after tooth extraction: symptoms, photos, treatment in the clinic and at home
Like other types of surgery, tooth extraction may well lead to complications that need to be treated. Among all the possible consequences after tooth extraction, the most common is alveolitis - inflammation of the socket , which cannot be treated at home due to the risk of developing more dangerous complications, for example, osteomyelitis.
Alveolitis photo of the hole
Often the hole may look normal, that is, without pronounced deviations, but this can be seen in the photo. But here you can consider the presence of a narrow inlet. It is also not very clear whether a clot is present in this case. Of course, making a diagnosis under such circumstances is very difficult. To do this, the doctor will have to conduct a full examination, which is performed using modern technology. And only because of the constant, very often in the form of increasing pain, smell from the open socket, tumor of the gingival tissue, can alveolitis be suspected.
Causes of alveolitis after tooth extraction
The extraction of teeth in itself is not a direct cause of the development of alveolitis. Factors that provoke inflammation of the tooth socket are complications that arose during surgery:
- Injury to the wall of the alveolus, in which the root was fixed before the tooth was removed.
- Penetration of infection into damaged jaw tissue.
- A dry socket after tooth extraction is the absence of a blood clot, which serves as a natural isolation of the resulting wound from pathogenic microorganisms.
- Tooth destruction during extraction.
- The presence of curved roots of the tooth being removed or growths on their surface.
- Root stuck in the gum after crown removal.
- Using additional removal methods: sawing, cutting.
Molars are large teeth with a large number of roots, so alveolitis appears more often after the removal of a wisdom tooth or adjacent molars than when pulling out incisors.
Alveolitis can develop due to an infectious disease of the tooth to be extracted or nearby gum tissue:
- Chronic inflammation in the gums.
- Presence of caries, periodontitis.
- An abundance of dental plaque with actively multiplying microbes.
Inflammation can be caused by improper actions of the dentist or patient: insufficient treatment of the instrument and wound, eating rough food after surgery, and poor hygiene. The patient's weak immunity increases the risk of developing inflammation.
What are the stages in the rehabilitation process?
To be able to identify the problem in time, you should know how and how long the hole heals, how long it can bleed and hurt after removal. And for this it is worth familiarizing yourself with the main stages of healing. Let's look at each of them in a little more detail.
Gradual restoration of soft tissues
A few hours are enough for a protective blood clot to form. You should not touch it or try to remove it, because it acts as a kind of barrier that prevents harmful microorganisms from entering an open wound. During the soft tissue healing stage, you should conscientiously brush your teeth at least twice a day, but without affecting the causative area. You should also rinse your mouth every time after a snack, but again without excessive intensity. Around day 2-3, epithelization begins, which is accompanied by the formation of granulation tissue. The patient loses severe pain, swelling and redness disappear. Next, the wound is covered with a white coating. To understand what a properly healing hole looks like, take a look at the photo below.
The photo shows a properly healing hole after removal
If plaque of a different color has formed in the hole, there is cause for concern. A yellowish or even black color of the hole, coupled with bad breath, indicates the onset of inflammatory processes. It should also be taken into account that after wisdom tooth extraction, the recovery process takes longer. Typically, figure eights initially grow in the wrong position, which is why, to remove them, the doctor has to cut the gum and then suture it. This involves more extensive intervention and, accordingly, longer rehabilitation.
Bone tissue regeneration
Bone tissue begins to form only 7-8 days after surgery. The blood clot should still remain in the socket, but the depression where the tooth used to be is no longer as clearly visible. The patient almost completely loses the feeling of discomfort; there is no more pain or discomfort. The bone regeneration process is usually completed by the end of the second week.
Consolidation of new bone tissue
New hard tissues become denser and stronger. After a certain period of time, they turn into full-fledged bone. This is a fairly long period, which, however, does not cause any discomfort to the person. However, the entire process takes about 4 months.
Fusion of bone with gum
The final stage of rehabilitation involves the fusion of new bone tissue with the jawbone. This stage also takes about 4 months, but only if the operation was successful and there were no complications. If inflammatory processes have occurred, fusion can take up to 6-10 months.
The photo shows the healing pattern after removal
Symptoms of alveolitis after tooth extraction
Alveolitis is an inflammation of the walls of the alveolar socket. Therefore, the disease is accompanied by all the local symptoms characteristic of the inflammatory process:
- Pain.
- Swelling.
- Redness.
- An increase in local or general temperature.
There are other signs of the disease:
- No blood clot after surgery.
- Covering the wound with a gray coating.
- Spread of swelling to the facial area.
- Swelling of nearby lymph nodes.
- Fetid odor from the wound.
- Weakness.
As pus accumulates in the wound formed after tooth extraction, the symptoms of alveolitis intensify. A person begins to experience weakness due to intoxication and elevated temperature; toothache radiates to the ear and temporal region.
What types of alveolitis are there?
Experts in the field of dentistry identify several forms of the pathology in question. The types of alveolitis and their characteristic symptoms are briefly described below.
Serous form
The pain is constant and aching in nature, becoming more intense while chewing food. The temperature usually does not rise, and there is no enlargement of the lymph nodes. This form may gradually develop within a week from the date of surgery. Further, the inflammation becomes more severe.
Purulent form
Severe pain appears, body temperature rises, and weakness appears. Infected tissues swell, which can cause the face to become asymmetrical. A yellowish coating and pus appear in the hole. The patient complains of pain when trying to open his mouth, and an unpleasant odor appears.
In the purulent form, pus is released from the hole
Chronic alveolitis
The purulent process in chronic form is characterized by subsidence of symptoms. The lymph nodes shrink, and the main acute signs of infection disappear. The temperature returns to normal. However, during the examination, the doctor discovers the proliferation of granulation tissue, in which necrotic areas can be recognized. The gums acquire a bluish tint, become swollen, and pus is released from the wound.
Diagnostics
It is impossible to determine the diagnosis on your own; you can only assume the development of inflammation in the socket. In order to diagnose the disease as soon as possible and begin its treatment, you should immediately consult a doctor.
The dentist asks the patient how much time has passed since the gum became inflamed and how much it hurts. Examines the wound, checks for the presence of a blood clot, plaque, or purulent odor. Based on external signs, a qualified specialist can make a rough diagnosis, but to determine the exact type of disease, he may need additional examinations, for example, X-rays and CT scans.
Clinical manifestations of alveolitis
After tooth extraction, pain is normal. As the hole heals, the pain subsides and goes away after a few days. With alveolitis, discomfort and pain first subside, but 3-5 days after tooth extraction, severe, sometimes throbbing pain in the socket appears. As the infection progresses, the pain intensifies. The severity of alveolitis is characterized by pain: the pain can be moderate or throbbing and unbearable. Pain is observed only in the area of the extracted tooth, but sometimes with alveolitis the pain radiates to the entire half of the face.
In addition, the following main symptoms are distinguished:
- Spread of pain beyond the affected area, for example, to the ear or temporal region;
- Deterioration of general condition;
- Body hyperthermia;
- The appearance of a fetid and putrid odor from the oral cavity;
- Swelling of the mucous membrane of the socket;
- The appearance of a gray coating on the walls and hole;
- No blood clot;
- Difficulty eating;
- Enlargement and pain in the lymph nodes;
- Discharge of pus from an empty socket.
The appearance of one or more of the above symptoms in the oral cavity is an absolute reason to consult a doctor for help, since they all indicate the presence of alveolitis. With alveolitis, the temperature can rise to low-grade levels, and tooth sensitivity to cold/hot food increases. Sometimes regional lymph nodes become enlarged, causing a bitter taste in the mouth and bad breath. Due to painful sensations, appetite decreases and salivation increases.
If the tooth socket was quite large, then alveolitis is accompanied by swelling of the face. Sometimes the general condition suffers, weakness, increased fatigue appear, and sometimes secondary infectious foci appear on the oral mucosa. Often alveolitis “evolves” and causes several serious complications, for example, leading to the development of osteomyelitis or periostitis.
Treatment of alveolitis after tooth extraction
Treatment of inflammation of the socket after tooth extraction is carried out only after an accurate diagnosis and as prescribed by the dentist. Self-medication at home can lead to serious negative consequences, including the loss of adjacent teeth and infection of internal organs by an infection that spreads through the bloodstream. At home, you can only perform those procedures that are prescribed by your doctor.
Doctors can treat alveolitis that appears after tooth extraction using different methods. The tactics of therapy depend on how quickly the patient sought help, at what stage the pathological process is, and what the individual characteristics of the patient’s body are.
Read also: Is it possible to eat before tooth extraction?
If active necrotic phenomena with tissue death are not observed in the wound, treatment will be limited to cleansing and disinfecting the hole. When alveolitis is advanced, it is necessary to remove all soft and hard tissues affected by the infection in order to stop the infection of healthy ones.
Treatment of early stages of alveolitis
If the patient sought help immediately as soon as his gums became inflamed, then treatment of alveolitis of the tooth socket will consist of the following steps:
- Local anesthesia.
- Rinsing the hole with an antiseptic solution.
- Cleansing the hole from pus, destroyed tissue elements and granulation particles.
- Repeated rinsing of the socket cavity with an antiseptic.
- Dry the surface of the hole with sterile gauze.
- Cover the wound with gauze soaked in antiseptic.
Advanced forms of alveolitis
Advanced alveolitis after tooth extraction requires intensive treatment using various medications:
- As in the early stages of the disease, the tooth socket is cleaned and washed with an antiseptic. A tampon with medicinal drugs that can relieve inflammation and normalize the microflora is placed in the hole. After this procedure, the wound hurts less.
- If the infection penetrates deeply, you need to block it with lidocaine. How many injections are needed depends on the progression of the disease: if the condition does not improve the first time, the manipulation is repeated.
- If there are dead areas of tissue in the hole, the dentist removes them using proteolytic drugs. Such medications are applied using a gauze bandage.
- Based on the decision of the dentist, who assesses the extent of the infection in the oral cavity, antibiotics may be prescribed in the form of drugs for local treatment or for oral administration. Rinsing with antiseptic agents is mandatory and must be done at home.
In case of severe inflammation, the hole hurts greatly, in this case you can take painkillers, but the doctor must select an effective drug. Independent choice of medications and long-term use of analgesics can lead to serious complications.
Complementary therapy
To speed up the healing of the inflamed hole, especially with the development of necrosis, additional treatment methods are indicated. The dentist may recommend:
- Take a course of microwave therapy or fluctuarization.
- Treat the hole with infrared laser or UV radiation.
- Resort to the balneotherapy procedure.
- If bone tissue is exposed, perform a smoothing procedure.
- Take vitamins.
Treatment of alveolitis after tooth extraction at home
Usually, inflammation of the socket is treated using traditional methods and medications, but the disease at an early stage of development can be treated at home using folk remedies. The most effective method of relieving inflammation in the socket is oral baths (holding liquid in the mouth) with a solution of potassium permanganate: 5 crystals per 1 liter of water.
In addition to the manganese solution, you can make baths with herbal infusions. Decoctions of chamomile, St. John's wort, calendula, and oak bark are suitable. It is recommended to take vitamin complexes that strengthen dental tissue and immunity.
If the inflammation of the hole does not subside or intensifies after several days of home therapy, you should urgently consult a doctor. Self-medication should be completely abandoned if there are severe symptoms of the inflammatory process, general malaise, or elevated temperature. Alveolitis can develop into osteomyelitis - inflammation of the bone tissue of the jaw, which can lead to its removal. Therefore, this disease cannot be ignored under any circumstances.
Forecast
With early diagnosis and timely initiation of treatment for this pathology, the prognosis in most cases is favorable . If the development of osteomyelitis is suspected, hospitalization in a specialized hospital may be indicated. If there is a decrease in immunity and the presence of concomitant pathologies, the use of broad-spectrum antibiotics is indicated. If you consult a dentist in time, treatment of alveolitis will take only a few days. Residual pain may persist for 2 weeks or more.
Plisov Vladimir, dentist, medical columnist
11 total today
( 39 votes, average: 4.38 out of 5)
Covering denture: design, advantages and disadvantages
Why do fillings fall out of teeth?
Related Posts
Alveolitis after wisdom tooth removal
Most often, alveolitis develops during extraction of third molars , which is associated with an increased traumatic operation: the gums are often cut and peeled off, and the tooth is sawed into pieces for easier extraction in the presence of curved roots.
Alveolitis in dentistry is a rather rare disease. However, if when removing ordinary teeth, pathology occurs in only 2% of cases, then when removing extreme molars, the incidence of this disease increases to 20%. Symptoms and treatment methods for inflammation of a wisdom tooth socket are standard.
Complications
If after treatment of alveolitis the patient’s socket begins to hurt, it means that it has become inflamed again. You will have to visit the dental clinic again; attempts to cure the inflammation at home may worsen it. For example, rinsing with hydrogen peroxide disinfects the wound, but this procedure removes the remaining blood clot, which makes the wound even more vulnerable to further penetration of pathogens. That is why rinses are replaced by oral baths.
Complications in the form of spread of infection deep into the dentofacial apparatus include osteomyelitis, phlegmonous tissue melting and abscess. If pathogens and their toxins have entered the blood en masse, a person faces sepsis, which, in the absence of surgical treatment, can lead to death.
A disease such as alveolitis should not be underestimated, since it can cause great harm to the body. Only a timely visit to the dentist to eliminate the infection will help prevent further tissue destruction. Therefore, after removing an incisor, canine or molar, you need to monitor the condition of the gums so as not to miss the first signs of inflammation.
Alveolitis after tooth extraction - symptoms and treatment
Alveolitis of the socket is an inflammatory process that, under a number of circumstances, can develop in the socket (alveolus) of an extracted tooth (for this reason it is sometimes also called post-extraction alveolitis).
In this case, both the tooth socket itself and the surrounding gum tissue are affected. Alveolitis of the socket most often acts as a complication after incorrect tooth extraction, accounting for 25 to 40% of all complications after tooth extraction.
If this procedure went well, then the healing process of the alveoli is almost asymptomatic, causing a minimum of discomfort in the first 2-3 days.
What is alveolitis
Alveolitis is an inflammation of the hole in the jawbone that formed after tooth extraction. Inflammation occurs as a result of infection entering the hole. In some cases, with alveolitis, damage to the socket or surrounding gum tissue may be noticeable.
After a tooth is removed, a blood clot forms in the socket. Its function is to protect the socket from infection and promote the healing of injured tissue. If there is no such clot or its integrity is somehow compromised, then tissue healing stops, the infection enters the socket and spreads, resulting in alveolitis after tooth extraction. Photos taken by dentists show that the alveolitis looks like an empty hole containing food debris and particles of dead tissue. While in a hole that heals without complications, you can see a dark red blood clot.
Causes of dental alveolitis
Infection of a tooth socket after extraction can be the result of the following main factors:
- In most cases, alveolitis appears due to injury to the walls of the socket. They are quite thin, so if handled carelessly, they can be damaged or completely broken. In addition, when bone tissue is destroyed, debris can get into the wound, which can cause infection. The risk of alveolitis increases significantly when wisdom teeth are removed.
- Another most common cause of alveolitis is infection. Pathogenic bacteria that provoke inflammation can be introduced into an open wound after tooth extraction from the outside - with dental instruments. The risk of infection entering the alveoli increases in people with oral problems (the presence of carious teeth, periodontitis, gingivitis, a large amount of plaque on the teeth). This is why dentists do not recommend removing teeth if you have ARVI, flu, sore throat, etc.
Alveolitis of the socket can also develop with:
- decreased immunity;
- insufficient oral hygiene and plaque getting into the hole;
- if part of the tooth root remains in the socket (for example, the root broke off during surgery);
- non-compliance with the doctor’s recommendations - removing a blood clot with particles of solid food, liquid with frequent rinsing, eating hot or spicy food immediately after tooth extraction;
- if there was a cyst in the area of the apex of the tooth root, which remained in the socket after tooth extraction;
- increased bleeding associated with impaired blood clotting or severe postoperative bleeding after traumatic surgery.
Alveolitis usually occurs when a tooth is removed due to advanced forms of caries, pulpitis, and gumboil. Age also plays a big role in its development. More often, this complication after tooth extraction occurs in older people.
The risk group for developing the disease includes people with a weakened protective function of the body, those with a positive HIV status, pathologies of the endocrine system and diseases associated with blood clotting disorders.
As a rule, at the initial stage, alveolitis is practically invisible, but it gradually progresses, that is, it spreads in width and depth. The first symptoms of alveolitis are observed 2-3 days after tooth extraction.
Therefore, the main symptoms in the initial stage will be:
- aching pain that may subside over time, but intensifies while eating;
- swelling, redness;
- soreness of the gums in the socket area;
- Swelling may occur, especially after wisdom tooth removal.
Left to chance, alveolitis can cause more serious symptoms, such as weakness, fever up to 37.5 - 38 degrees, and increased fatigue. The lymph nodes may become inflamed, tooth sensitivity may appear, an unpleasant odor may occur, a bitter taste may be felt, and the pain may radiate to the ear or, for example, to the temporal region.
Alveolitis is a rather complex disease that is very painful for humans. The more neglected it is, the more unpleasant the symptoms of the disease and the more difficult it is to cure. Therefore, it is necessary to consult a doctor at the slightest suspicion of alveolitis. The sooner medical assistance is provided, the faster the recovery will occur and the lower the likelihood of developing severe complications.
Signs of alveolitis
The inflammatory process with alveolitis begins with the outer layers lining the tooth socket. Later, the infection penetrates into the deeper layers of the bone. In addition to inflammation, suppuration and tissue death are possible, which can lead to even more serious complications, such as osteomyelitis of the jaw (bone destruction), periostitis (inflammation of the periosteum tissue), abscess, and phlegmon.
How do you know if you have alveolitis after tooth extraction? The symptoms of this complication in the first stage are subtle, and the patient may not realize that something is wrong. Therefore, in no case should you neglect routine dental examinations after tooth extraction. As the disease progresses, symptoms become more pronounced.
Initial stage of alveolitis:
- Aching pain in the tooth socket, which can sometimes go away completely, but always intensifies while eating.
- The patient's general condition and body temperature are normal.
- When examining the tooth socket, you can notice the absence of a blood clot in it. Sometimes only part of it is available. The hole is filled with saliva and food debris.
- The gum adjacent to the socket is bright red and painful to the touch.
Alveolitis in a progressive stage:
- Severe pain in the socket and throughout the gum. The pain can radiate to the ear, temple and half of the head corresponding to the extracted tooth.
- The patient feels general malaise and chills.
- Low-grade fever persists constantly.
- Pain in the jaw interferes with chewing food.
- When examining the hole, the remains of a decomposed clot and a gray coating are found.
- You may notice pus discharge from the socket.
- A pungent smell of rotting emanates from the hole.
- Swelling appears around the hole, the mucous membrane is unnaturally red and very painful when touched.
- The submandibular lymph nodes become enlarged and pain appears on palpation.
- Swelling of the cheek on the corresponding side may occur.
How to treat alveolitis
Treatment of alveolitis after tooth extraction should begin during the period when the disease has just made itself known. Otherwise, the duration and cost of therapy will be significantly higher. Only a dentist can determine that you have alveolitis and not some other disease. He will prescribe the appropriate treatment for you.
Doing this yourself at home using rinses or antiseptic drugs is unacceptable. You can relieve some symptoms and at the same time drive the disease inside, where it will further develop, involving more and more tissues in the process and posing an increasing threat to your health.
However, until you have an appointment with the dentist, you can reduce pain with the help of painkillers:
Before starting treatment, the patient is given an x-ray. The image will indicate the presence of foreign elements or tooth fragments in the gum cavity. Next, anesthesia is performed, and the following manipulations:
- Cleaning the hole of an extracted tooth and washing out purulent discharge with special solutions.
- Local applications with analgesics and antimicrobial agents.
- Rinsing the mouth with antiseptic solutions.
- Physiotherapeutic procedures for speedy healing of the wound (after relieving inflammation).
If treatment is started on time, then within a week the inflammatory process is stopped, the wound is covered with protective epithelium, which indicates a positive dynamics of treatment. After this, the patient must follow treatment recommendations and regularly visit a specialist for examination.