In our country, epidermolysis bullosa is a rare disease. About one in 200 thousand people suffers from it in different stages and types. The disease is genetic in nature, so both men and women are susceptible to it. But the disease is more common in children and adolescents.
- Classification
- Causes
- Symptoms of epidermolysis bullosa
- Diagnostics
- Treatment Options
- Complications
- Forecast
Video: Epidermolysis bullosa in children: current state of the problem
Characteristics of the disease
Children and adolescents are most vulnerable to epidermolysis bullosa
The disease epidermolysis bullosa involves pathologies and mutations of more than 10 human genes. Failures at the gene level cause the formation of erosions and blisters on the skin and mucous membranes. Any, even weak, mechanical contact with the skin causes erosions on sensitive, vulnerable skin. The affected area can be completely different - from a small area to damage to the entire skin.
Doctors compared the increased vulnerability of the skin with this disease to the fragility of the wings of a butterfly, and therefore even called it butterfly disease.
The disease occurs due to the destruction of the adhesive layer in the skin, which gives the skin layers elasticity and protects them from damage . When gluing does not occur, the layers of skin seem to shift and separate from each other, which makes the skin layers vulnerable to any irritation.
The main goal of treatment is to prolong remission as much as possible by providing proper care for the patient and using different treatment methods.
Important! In most cases, epidermolysis bullosa is congenital. The disease cannot be prevented, since all processes occur at the genetic level.
Treatment
Currently, there are no radical treatments for any form of EB. Despite this, there are effective preventive and symptomatic treatments. In general, treatment should be comprehensive and carried out by a multidisciplinary team of doctors, since EB is a systemic disease[46][47].
Treatment of BE is symptomatic. The main thing in the treatment of BE is wound care for the purpose of their rapid healing and epithelization of the skin. The main task is to prevent the bladder from growing in size and to preserve the bladder cover to prevent erosion and better wound healing. Most wounds of patients with BE are covered with atraumatic non-adhesive materials and multiple layers of bandages[48].
Treatment of any complications is also symptomatic and aimed at maintaining the functioning of all organs and systems. Patients with severe subtypes of EB often require gastrointestinal surgery and finger separation surgeries[49][50][51].
On November 10, 2020, the University Hospital of Bochum announced the successful completion of treatment with skin transplantation, which lasted two years. A child with EB managed to replace almost all of his skin with healthy transgenic skin grown from his own cells, into which a working version of the LAMB3 gene was inserted.
Classification
Epidermolysis bullosa has a huge number of types and subtypes. Only the simple type of this disease has 12 subtypes, such as Koebner, Weber-Cockayne, Dowling-Meara syndromes . Pathology can affect the outer layers of the epidermis, and blisters and erosions can also occur in the inner layers of the skin when the protein of the epidermis is damaged.
In addition to the simple type of disease, there are:
- Borderline - located on the border of simple and dystrophic epidermolysis bullosa. In this form, pathologies are associated with damage to the skin enamel, and large areas of the body can be affected;
- Dystrophic - associated with dominant and recessive types of gene mutation formation. Erosions affect the deep layers of the skin and often develop in the papillary layer of the dermis, causing scars to form and erosions to heal with great difficulty;
- The mixed form is the rarest form of the disease. The name is due to the fact that lesions can affect any layer of the skin: epidermis, dermis, light plate.
In addition to the congenital disease, there is acquired epidermolysis bullosa, which is associated with chronic diseases of various systems and organs, hormonal disorders and endocrine problems. It rarely appears in the adult population with diseases of the skin of the feet and palms, on which blisters appear, which subsequently form scars and cicatrices. Acquired disease is divided into:
- Classic appearance - lesions appear on the bends of the limbs, mucous membranes of the nose, mouth, anus, etc.;
- Inflammatory - skin damage occurs in any open area.
Forms of the disease
The term epidermolysis bullosa includes several forms of the disease, differing in symptoms, course and prognosis.
Simple congenital
The location of the disease is the hands, knees, and elbows.
Epidermolysis bullosa simplex occurs in 1 in 50,000 newborns. This disease was described back in 1886. The type of inheritance is autosomal dominant; to date, families have been known in which epidermolysis bullosa simplex was diagnosed already in the eighth generation.
The main symptoms of a simple form of epidermolysis bullosa:
- The disease begins immediately after birth and a short time after it. Boys get sick more often than girls.
- Blisters appear on areas of the skin that have been subjected to even slight pressure, friction or other mechanical stress. The blisters are filled with serous fluid and can range in size from a pinhead to a walnut. The skin around the blisters does not become inflamed.
- The main locations of rashes are hands, knees and elbows, legs and feet.
- For most newborns with a simple form of epidermolysis bullosa, the first traumatic factor is the birth process itself. As a result, rashes occur on the skin that is in close contact with the birth canal.
- Bubbles are opened naturally or artificially. After their resolution, superficial skin defects (scarring, tissue degeneration) are not observed. Temporary pigmentation may remain in place of the opened blisters.
- In the simple form of epidermolysis bullosa, the mucous membranes are affected extremely rarely, in approximately 2% of cases. Nails are not destroyed. Increased sweating of the feet and palms may occur (in about a quarter of patients).
- The child’s general well-being is not impaired, mental, mental and physical development occurs in accordance with age.
- Some deterioration of the condition is noted by the age of 8 - 12 months, when the child begins to crawl and walk due to an increase in the degree of exposure to the skin.
- As a rule, the symptoms of the disease appear more pronounced in summer than in winter.
- By adolescence, as a rule, manifestations of epidermolysis bullosa weaken or completely disappear.
The simple form of epidermolysis bullosa may include a localized form, which is also called the summer form or Weber-Cockayne syndrome. This form of the disease may not appear immediately after birth, but in the first or second year of life. Rashes in the summer form of epidermolysis bullosa are located only on the feet and hands. The blisters often have bloody-serous contents. A deterioration in the condition of patients is observed in the summer, after taking hot baths or when wearing warm shoes.
Dystrophic
Dystrophic epidermolysis bullosa has two forms - hyperplastic and polydysplastic.
This type of disease weakens by adolescence.
Symptoms of the hyperplastic form of epidermolysis bullosa:
- the disease begins to appear either immediately from the moment of birth, or 1 - 2 days later;
- rashes appear after any mechanical impact on the skin;
- after the bubbles resolve, scarring skin changes may appear in their place;
- Nikolsky syndrome (tendency to peel off layers of the epidermis after mechanical impact on the skin) is negative for this form of epidermolysis bullosa;
- Not only the skin can be affected, but also the mucous membranes, on which degenerative changes are noticeable after the rash resolves;
- hair, nails and teeth do not undergo pathological changes;
- the child’s physical and mental development does not suffer;
- By adolescence, the manifestations of the disease weaken.
Symptoms of the polydysplastic form of dystrophic epidermolysis bullosa:
- the disease manifests itself from the moment of birth;
- rashes are observed on the skin and mucous membranes, and their formation is not always associated with mechanical action; blisters can also appear spontaneously;
- often the blisters have bloody contents. After opening them, ulcers form, which gradually heal;
- rashes can cover large areas of skin surfaces;
- Nikolsky's symptom in this form of epidermolysis bullosa is positive;
- Often patients are bothered by severe itching;
- nails quickly become smaller and disappear completely;
- after the ulcers heal, scar tissue forms, which can limit joint mobility;
- with this form of epidermolysis bullosa, tissue necrosis and spontaneous rejection of body parts, most often the phalanges of the fingers, are often observed;
- Patients often experience dysplasia (underdevelopment of organs or tissues), hypotrichosis (underdevelopment of hair), dental anomalies;
- The polydysplastic form of epidermolysis bullosa is characterized by severe damage to the mucous membranes of internal organs:
- the general condition of the patients is severe, there is a severe delay in physical and sometimes mental development. Decreased ability to resist infections. The prognosis for this form of epidermolysis bullosa is unfavorable.
Malignant
This form of epidermolysis bullosa is fatal. It manifests itself immediately after birth with the appearance of a generalized rash in the form of bleeding blisters. The rash covers the skin and mucous membranes, including the mucous membranes of the esophagus, stomach, and intestines.
After opening the blisters, painful, poorly healing ulcers form. Congenital dystrophies of nails and bone tissue are observed. The disease, as a rule, is complicated by the addition of pyococcal infection, sepsis and ends in the death of the infant.
Causes
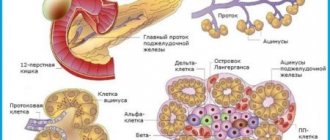
The disease appears due to mutations of 10 genes
The main cause of the disease is a mutation of 10 types of genes, as a result of which the protein is destroyed under the influence of a pathogenic secretion secreted by the body's enzymes . For example, a simple form of the disease appears with pathologies of the KRT5 and KRT14 genes. Proteins become susceptible to pathogenic secretions, and the integral structure of the skin is disrupted. The borderline type of disease is caused by malfunctions in the genes LAMB3, LAMA3, etc. With this pathology, the protein structure that supports the structure of the lower layers of the epidermis is destroyed. The dystrophic appearance is provoked by altered genes such as COL7A1. In this variety, type 7 collagen protein, which is responsible for the connective tissue of the skin, suffers and is destroyed.
It turns out that malfunctions in the gene composition lead to the activation of harmful enzymes that kill the protein that is necessary for the normal functioning of the skin. The skin becomes brittle, vulnerable and susceptible to any external influence, which entails the formation of intractable ulcers, erosions, and blisters.
Symptoms of epidermolysis bullosa
The main symptom of epidermolysis bullosa is increased skin sensitivity
With epidermolysis bullosa, symptoms can be very diverse - from characteristic blisters on the skin to vomiting and diarrhea, as well as weight loss.
But the main symptoms of the disease include:
- Increased skin sensitivity;
- Bubbles;
- Ulcers;
- Erosion;
- Milia are white round formations;
- Thickening of the nail plate or its absence;
- Thickening of the skin on the feet or palms;
- Lack of hair or noticeable thinning;
- Blistering formations in the mouth.
With different types of disease, these symptoms may manifest themselves differently, and the following will also be different:
- Localization of foci;
- Degree of expression;
- Area of affected areas;
- Time of exacerbation and healing, etc.
So, for example, with a localized form of epidermolysis bullosa simplex (Weber-Cockayne subtype), only the feet and hands are affected. And with the generalized subtype - most of the skin in any area.
There are also specific manifestations of a certain type of disease. Thus, with the borderline form, symmetrically located blisters often appear on large areas of the skin. Fever and severe physical condition are also a sign of this type of disease. In dystrophic epidermolysis bullosa, scars and scars are often recorded along with erosions and blisters.
Important! An experienced doctor will be able to make a preliminary diagnosis even during an external examination.
Epidemolysis bullosa: causes and treatment of congenital butterfly skin disease
Epidermolysis bullosa is also called butterfly disease. Pathology received this comparison due to the fragility of the outer integument, like that of an insect.
The disease occurs due to gene mutation and, as a result, the synthesis of protein structures is disrupted.
Moreover, ordinary epidermolysis bullosa is inherited in an autosomal dominant manner, borderline epidermolysis is inherited in an autosomal recessive manner, and dystrophic epidermolysis is inherited in both ways.
As a result of such genetic disorders, the activity of tissue enzymes in the skin decreases. This leads to the destruction of proteins in the basement membrane, dermis or epidermis and disruption of connections between the layers of the skin. As a result, even a small mechanical impact leads to the formation of bubbles and erosions.
Classification
Butterfly skin disease is classified depending on the genotype, phenotype and mode of inheritance. The following forms of epidermolysis are distinguished:
- epidermolysis bullosa simplex - occurs in a ratio of 1:100,000. Blisters occur in the upper layers of the skin. They are found on the hands and feet, sometimes throughout the body. With a mild degree, scars do not form, but repeated manifestations of the disease are possible. There are localized and generalized subtypes;
- borderline epidermolysis bullosa - incidence 1:500,000. Skin lesions appear in the area of the light plate. There are 2 subtypes. The Herlitz subtype is the most severe, with frequent deaths;
- dystrophic epidermolysis bullosa - there are also 2 subtypes. They are divided according to the type of inheritance (dominant and recessive). The frequency of occurrence of the dominant is 3:1000000, and that of the recessive is 1:5000000. Bubbles appear in the area of the papillary dermis, below the lamina densa. The formations are located on the arms, legs or throughout the body. Characterized by a severe course with frequent relapses;
- Kindler syndrome (mixed epidermolysis bullosa) - characterized by the appearance of blisters in all layers of the skin: epidermis, dermis, lamina lucidum. This subtype is poorly studied and currently only one protein target for enzymes is known. It is called kindlin-1.
Symptoms
All types of congenital epidermolysis bullosa have one symptom in common: the formation of blisters when exposed to the skin. Their location, severity and healing process vary. With the localized subtype, blisters appear in the summer and are located on the hands and feet.
As the patient gets older, their number decreases. The generalized Dowling-Meara subtype is severe, affects the entire body, and appears immediately after birth. The generalized type often ends in death.
At the site of the opened vesicles, hyperkeratosis or pigmentation disorders may form.
The borderline type of the disease has a severe course, especially the Herlitz subtype. The latter is characterized by high fragility of the skin, a large number of blisters and eroded lesions, which often form on the back and face. The lesions affect both the mucous membranes and the enamel of the teeth, and caries forms early.
This type of disease leads to nail dystrophy and alopecia.
Epidermolysis, which occurs according to the dystrophic type, spreads throughout the body. With a dominant type of inheritance, the course is more favorable. Bubbles form and resolve slowly, and scars form in their place. Often patients lose the nail plates on their hands.
With a recessive type of inheritance, especially the generalized form, the course is severe. In addition to blisters, scars form on the body of patients, which can develop into squamous cell carcinoma. Such patients have missing nails and bones may be affected.
The recessive subtype is difficult to treat.
Diagnostics
Diagnosis of epidermolysis bullosa consists of several stages. Hereditary history, examination, immunohistological and genetic tests help make a diagnosis.
During the examination, the doctor can perform a mechanical effect on the skin and after some time record the presence or absence of blisters.
Immunofluorescence analysis is carried out using antibodies. They may be polyclonal or monoclonal. Antibodies are aimed at identifying proteins of the epidermis, dermis and lamina lucidum. Their number indicates tissue enzymatic activity.
If the amount of protein is reduced, this indicates either its slow release or increased destruction.
A low concentration of proteins makes it possible to diagnose the level of blistering at the initial stages, which will help determine the type of epidermolysis bullosa.
Genetic analysis allows you to accurately determine what type of epidermolysis the patient suffers from.
You can quickly make a diagnosis if relatives have a similar problem. Studying the hereditary history will help with this. In addition, if either parent suffers from epidermolysis bullosa, prenatal diagnosis is necessary to rule out the disease in the fetus.
Treatment
Treatment for epidermolysis bullosa has not yet been developed. The therapeutic methods used are aimed at reducing the number of blisters, their severity and preventing complications.
In severe cases of the disease, treatment is carried out with prednisolone. For any type of epidermolysis bullosa, the blisters are opened under aseptic conditions, antiseptics are applied to their lid, and heliomycin ointment is applied on top.
Bandages are applied with caution, as injury to the skin may result in the appearance of new blisters. If sepsis or shock develops, treatment with antishock or antibacterial drugs is prescribed.
Currently, research is being conducted in the field of genetics to find new treatment methods. Animal trials using stem cells, protein and gene therapy are already underway. But there is no cure for epidermolysis bullosa.
Complications
Complications of epidermolysis bullosa can include shock, sepsis and dehydration. A state of shock develops with extensive skin lesions.
Sepsis and dehydration occur when a secondary infection occurs. The more blisters, erosions and ulcers, the greater the likelihood of complications.
Treatment includes measures to eliminate factors that can lead to the listed conditions.
Lifespan
How long do people live with epidermolysis bullosa? Life expectancy depends on how much the gene structure is changed and how deeply the tissue and body are damaged. Severe forms may be accompanied by extensive tissue damage, infection, and damage to internal organs. Often in this case the patient dies in infancy.
How long the patient will live depends on the care he receives. With maximum effort, one can achieve relief of suffering and improve the patient’s quality of life. In general, life expectancy with this diagnosis is low.
Several cases have been described in which patients were completely cured. It has become known that certain body systems can restore the genetic structure through new mutations (reverse mosacism). Such self-healing is extremely rare.
Prevention
Prevention comes down to prenatal diagnosis if there are cases of epidermolysis bullosa in the family. If necessary, a fetal biopsy is performed under ultrasound guidance in the second trimester of pregnancy.
Despite the fact that epidermolysis bullosa is an incurable pathology, the severity of which depends on the type of genetic disorder, its course can be influenced. With timely diagnosis, proper treatment and proper care for the patient, the outcome can be favorable. In other cases, treatment will help alleviate the patient's condition.
Source: https://dermatologiya.pro/nasledstvennye-bolezni/bulleznyj-ehpidermoliz.html
Diagnostics
Genetic tests are required for an accurate diagnosis and treatment plan for the disease.
External signs of the disease already make it possible to make a preliminary diagnosis. But to determine the type and subtype of the disease, doctors use other diagnostic methods - in particular, laboratory tests: blood tests (hormones), general blood test, skin scrapings, immunohistological studies, etc.
To make an accurate diagnosis, understand the cause of the disease and develop an effective treatment regimen for the disease, genetic tests are needed.
Diseases that are inherited from generation to generation need to be given increased attention. And only research at the molecular level allows us to give an accurate assessment of the presence of a predisposition to this disease. Our genes contain information about the tendency to develop skin pathologies. In addition to blood tests, geneticists conduct a histological analysis of the affected areas of the skin, which confirms the presence of a subepidermal cavity.
Geneticists determine:
- genetic predisposition to the disease;
- what specific genes triggered the disease;
- which medications are indicated and which are contraindicated for the patient;
- blood clotting rate is monitored.
Thanks to the result of the genetic analysis, the geneticist:
- when a disease is detected, prescribes optimally effective medications that will not harm the patient’s other organs;
- determines other therapy that will bring maximum benefit to a particular patient.
When this data is not enough to determine the exact type of epidermolysis bullosa, an instrumental clinical diagnostic method is used - in particular, electron microscopy is performed, which will help to see the level and synthesis of protein, as well as structural changes in the skin and the state of cellular formations.
If necessary, doctors of other specializations are involved: oncologists, hematologists, dentists, cardiologists, surgeons, gastroenterologists, otolaryngologists.
Laboratory diagnostics
The most reliable and reliable method of diagnosis is the examination of skin samples taken during biopsy using transmission electron microscopy, but now indirect immunofluorescence has become the main method for diagnosing BE, when monoclonal and polyclonal antibodies against the most important proteins of the epidermis and the epidermal-dermal interface involved in the pathogenesis of BE[39].
In BE, immunohistological (immunohistochemistry and immunofluorescence) methods are used to determine the presence, absence or reduced expression of structural proteins of keratinocytes or the basement membrane, as well as the distribution of certain proteins in naturally formed or artificially caused blisters [40] [41]. This way you can determine the level of blistering: inside the epidermis, at the border of the epidermis and dermis. Immunohistological methods, along with DNA diagnostic methods, serve as the main methods for diagnosing EB. With their help, it became possible to quickly classify EB and determine the main type of EB, determine the structural protein most likely to undergo mutation and determine the clinical prognosis [42][43].
The results of immunohistological examination provide a basis for further search for mutations, indicating which genes encoding structural proteins of keratinocytes or the basement membrane should be examined.
Transmission electron microscopy allows for visualization and semi-quantitative assessment of certain skin structures (keratin filaments, desmosomes, hemidesmosomes, anchor filaments, anchor fibers) that are known to be altered in number and/or appearance in certain subtypes of EB[44].
After determining the type or subtype of EB using immunohistological methods, genetic analysis can be performed. Genetic diagnostics makes it possible to identify mutations, determine the type and location of the mutation, and, ultimately, the type of inheritance of the disease. Currently, genetic analysis is a method that reliably confirms the diagnosis. For EB, genetic analysis is usually carried out using direct sequencing. Genetic analysis allows for prenatal diagnosis of subsequent offspring in a family where there is a patient with EB[45].
Treatment Options
Antibiotic ointments are common for external treatment of epidermolysis bullosa.
Today, there are many treatment methods that can achieve long-term remission.
The main modern treatment methods for this complex disease include:
- Gene therapy - by transplanting healthy skin to the diseased area;
- Protein treatment - intradermal injection of collagen, which will normalize the amount of protein;
- Cellular method - introduction of cells with a normal gene or fibroblasts - connective tissue cells that will help connect the layers of the skin;
- Stem cells - a method using bone marrow cells (both donor and own);
- Combination therapy - the use of cell, stem, gene methods of treatment.
- Drug therapy relieves symptoms, maintains protein levels, normalizes the number of enzymes that stimulate immune and metabolic processes to compensate for hormonal deficiency and immunodeficiency.
These drugs include anabolic steroids, Pentoxyl, Levamisole, Methyluracil. Vitamin E helps restore skin elasticity; vitamins A and C are also indicated. Non-hormonal preparations based on sulfur, potassium, zinc, iron and calcium can also normalize the level of collagen in tissues.
In external therapy, ointments of both hormonal and non-hormonal action are used. In addition, ointments with antibiotics are used, which relieve inflammation and have an antibacterial anti-inflammatory effect. Such drugs include “Iruksol”, “Butadione”, “Solcoseryl”. Among hormonal ointments, “Corticomycetin”, “Lorinden S”, “Oxycyclosol”, “Oxycort”, “Gioxy-zon” are often used.
As a supplement to the main therapy, the doctor may recommend traditional medicine. Thus, compresses and lotions based on decoctions of plantain, oak bark or string are suitable for relieving inflammation.
For some types of disease, medication and physical treatment have a good effect. For example, electrophoresis, phonophoresis with hydrocortisone and zinc sulfate, UHF, and ultraviolet radiation are often used.
Important! Unfortunately, a panacea for this disease has not yet been invented. Therefore, the goal of effective treatment is to relieve inflammation and exacerbation, as well as prevent the appearance of new lesions.
Treatment of epidermolysis bullosa
There is no specific treatment for epidermolysis bullosa. All measures are aimed at eliminating itching and burning during the opening of the vesicles. It is also necessary to ensure sterility to prevent infection from entering the eroded skin.
In order to resolve colloidal scars of connective tissue, physiotherapy methods and drugs containing biostimulants are used. They can be presented in the form of ointment and gel (solcoseryl, methyluracil).
In severe cases, hormonal therapy is indicated, which, although it has some side effects, can still save the child from painful suffering.
During periods of exacerbations, lotions with soothing herbal decoctions, zinc ointment, D-panthenol spray, Actovegin ointment, napkins soaked in silver solutions and many other modern pharmacological agents can be used. Celestoderm ointment or Lorinden S helps relieve itching.
Complications
The danger of incorrect diagnosis and illiterate treatment of epidermolysis bullosa is that under these circumstances the disease continues to progress, which entails tissue necrosis . Purulent discharge, abscess, peritonitis and other secondary infections may also occur, which can be fatal.
With proper treatment and the patient's compliance with all doctor's prescriptions, remission is inevitable.
There are subtypes of the disease that are life-threatening. Thus, the Herlitz subtype, according to its statistics, in most cases ends in the death of the patient. Also, with late-stage dystrophic epidermolysis, pathologies of the joints and mucous membranes of the respiratory and digestive systems occur. Scars left behind by blisters are often the basis for the appearance of malignant tumors.
Malignant tumors often appear on scars that remain after erosions have healed.
Borderline epidermolysis of the Görlitz and Non-Gerlitz subtypes provokes complications that do not affect the skin. Thus, anemia, blockage of the respiratory tract, growth of the tongue to the lower part of the mouth, and narrowing of the mouth often occur. These types of illness are often fatal.
Some types of epidermolysis cause damage to internal organs: the digestive system, circulatory system, cardiovascular system, and so on. Some emerging pathologies of organs and systems are also incompatible with life.
Important! Treatment of epidermolysis is aimed at preventing complications - damage to other organs and systems, the addition of a secondary infection, the development of shock, etc.
Treatment methods
To date, there are no specific treatments for epidermolysis bullosa. When choosing therapy, special attention is needed:
- Prevention of traumatic skin injuries;
- Prevention of secondary infections.
Breastfeeding is the main treatment for epidermolysis bullosa.
At an early age, when the child’s immune mechanisms have not yet been formed, it is important to prevent the risk of developing sepsis. It is highly advisable to provide breastfeeding to the child.
In severe forms of epidermolysis bullosa, treatment with glucosteroid hormones is indicated. As a rule, Prednisolone is prescribed up to 60 mg per day; as the condition improves, the dose is reduced until complete withdrawal.
In addition, anabolic agents, broad-spectrum antibiotics, and plasma infusions are prescribed.
External therapy for epidermolysis bullosa is as follows:
- the resulting bubbles are opened on both sides using sterile needles;
- the tires of the bubbles are lubricated with antiseptic solutions - brilliant green, methylene blue, eosin, fuchsin;
- Applications are made to the erosion using iruxol or heliomycin ointment;
- ointments containing glucocosteroids and antibiotics are used;
- bandages and the use of plaster should be avoided to avoid putting additional pressure on the skin;
- Physiotherapy - general ultraviolet irradiation - gives a good effect.
Forecast
The outcome of treatment for the disease will depend entirely on:
- Stages of the disease;
- Type (subtype) of disease;
- The presence of other chronic diseases;
- Features of the patient’s physiology;
- Age;
- The degree of damage to skin areas;
- Presence of concomitant diseases.
If you consult a doctor in time with a small lesion of the skin, then if you correctly follow all his recommendations, the prognosis will be comforting. You will be able to enter a long, lasting remission.
For information about the state of knowledge of the problem and statistics of the disease, watch the video.
Video: Epidermolysis bullosa in children: current state of the problem
Life expectancy with epidermolysis bullosa
How long you live with this disease will depend on:
- Depth of skin damage;
- Damage area;
- Stages of the disease;
- Type and subtype of the disease.
Unfortunately, it is difficult for children to reach school age; it requires a lot of effort and courage. There are a number of types of pathologies that do not allow children to live beyond 3 years of age. In dystrophic forms, the prognosis is unfavorable - death occurs in adolescence, in the malignant form - from sepsis at an early age.
But if the form is mild, then with proper treatment you will be provided with stable remission for many years. You will be able to lead a full life, and epidermolysis bullosa will not affect its quality.
How is BE recognized and treated?
The main symptom of epidermolysis bullosa is the appearance of a rash on the skin - blisters filled with fluid. In addition, nails may become deformed, problems may arise with breathing and swallowing (if EB affects the internal integument of the body), with teeth (fragile teeth, caries, gum disease) and hair (if blisters form on the head). The first symptoms of the disease usually appear in early childhood.
It will not be possible to cure the “butterfly child”, because the disease was caused at the genetic level. Patients will need special care throughout their lives. Treatment by doctors is symptomatic, depending on the type and course of the disease. Vitamin preparations, antibiotics and other medications are prescribed, the blisters are opened and smeared with special agents.
At the same time, “butterfly children” need special care: soft household items, clothing fabrics, shoes. You need to follow a diet and respond in time to exacerbations of the disease.