What is hypogonadism
Hypogonadism in women is a disease characterized by insufficient functioning of the gonads and problems with the production of sex hormones. As a rule, this pathology is accompanied by insufficient development of the organs of the reproductive system and secondary sexual characteristics.
This disease occurs in men and women, but in each situation it has characteristic features. In the female body, hypofunction of the ovaries is usually observed, which negatively affects the condition of the reproductive and reproductive systems.
With a disease such as female hypogonadism, the patient’s ovarian function decreases. In some cases, the ovaries stop working completely. Hypogonadism is divided into primary and secondary.
Primary hypogonadism
Primary hypogonadism in women is a violation of ovarian function due to their damage in the newborn age, as well as due to congenital underdevelopment. There is an insufficient amount of estrogen and progesterone in the body, and this leads to the fact that the pituitary gland begins to produce gonadotropins in large doses, which stimulate the ovaries.
The blood contains large quantities of follicle-stimulating and luteinizing hormones, and the amount of estrogen, on the contrary, is very small. Because of this, there is underdevelopment of female hormones and mammary glands. Menstruation may be absent for six months. If ovarian disorders occur before puberty, weak development of secondary female sexual characteristics can be observed.
Secondary hypogonadism in women
In this case, ovarian function is reduced due to the fact that the pituitary gland does not produce sufficient amounts of follicle-stimulating and luteinizing hormones. There is no damage to the ovaries.
Manifestations of female hypogonadism
- Narrow pelvis;
- Amenorrhea (a phenomenon in which there is no menstruation for six months or more);
- If the disease began to develop in childhood, secondary sexual characteristics are practically not represented; if they are present, they are underdeveloped (little pubic hair, lack of distribution of fatty tissue according to the female type);
- Disrupted menstrual cycle (periods are either irregular or completely absent);
- There is poor development of the internal genital organs (hypoplasia of the ovaries, uterus and fallopian tubes).
Hypogonadism in women, etiology of the disease
The causes of primary hypogonadism are considered to be:
- Polycystic ovaries;
- Ovarian hypoplasia (their underdevelopment of a congenital nature);
- Postponed oophorectomy;
- Effect of ionizing radiation;
- Autoimmune oophoritis;
- Congenital pathology of a genetic nature (Shereshevsky-Turner syndrome);
- The influence of past infection (syphilis, mumps, tuberculosis).
If we consider the causes of secondary hypogonadism, we can highlight:
- Infectious processes occurring in the brain (meningitis, arachnoiditis, encephalitis);
- Development of tumors in the brain;
- Congenital and acquired hypopituitarism;
- Age-related hypogonadism in women.
Methods for detecting this disease
- First of all, a general examination of the patient is carried out, during which the doctor examines the mammary glands, studies the distribution of subcutaneous fat throughout the body, and determines the presence or absence of hair growth.
- Examination and observation by a gynecologist.
- Consultation with an endocrinologist.
- Study of hormone levels in the blood (mainly estrogen, prolactin, FSH, LH, progesterone).
- Ultrasound of the pelvic organs.
- X-ray of the skeleton in order to determine the delay in its development.
- Test for the presence of osteoporosis.
Diagnostics
Diagnosis of primary amenorrhea
- Anamnesis collection. To make a diagnosis of amenorrhea, it is necessary to carefully analyze the girl’s medical history, including family history. Perhaps late menarche is an inheritance from mother, grandmother, and other relatives. It is necessary to collect information about the girl’s sexual development, the operations she has undergone, find out when secondary sexual characteristics appeared, whether the girl adheres to any diet, or whether she is involved in “non-female” sports.
- General inspection. The doctor pays attention to physique, height, the presence of hypertrichosis (excessive body hair growth), and the development of the mammary glands.
- Examination in a gynecological chair. It is carried out to exclude defects of the genital organs - androgenital syndrome and gonadal dysgenesis.
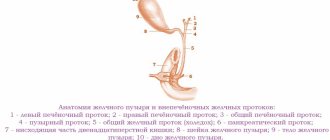
- Ultrasound of the pelvic organs. Check for polycystic ovary syndrome.
- MRI of the brain and pituitary-hypothalamic study. To identify or exclude pathologies of pituitary gland development.
- Karyotyping. A method that allows you to detect or exclude a number of genetic pathologies.
Diagnosis of secondary amenorrhea
The condition is detected in several ways:
- Examination in a gynecological chair. When diagnosing amenorrhea, pregnancy should be excluded. By asking, it is determined whether the cause of amenorrhea is diet, physical overload or stress. Exclude genetic predisposition.
- Tests for amenorrhea: plasma prolactin levels. It should not exceed 20 ng/ml. If there is too much prolactin, the pituitary gland should be examined;
- on the level of FSH (follicle-stimulating hormone). It is increased when the gonads are underdeveloped, decreased when the pituitary gland is insufficient;
- on the level of LH - luteinizing hormone. If the indicator is too high and FSH is below average, this is evidence of polycystic ovaries.
- measurement of the density of thyroid hormone accumulation: T4 and TSH (thyroxine and thyroid-stimulating hormone);
- Glucose tolerance tests, glucose level measurement.
- progesterone test. If the test is negative, the cause of amenorrhea is the effect of hormones on the endometrium or its changes for another reason. If positive, bleeding occurs during anovulation with preserved estrogen secretion.
Read also…. How to properly harden with cold water: methods and methods of hardening
You can avoid the appearance of amenorrhea by adhering to the principles of a healthy diet, the correct way out of stressful situations, maintaining a normal weight, regular sex life, and systematic visits to the gynecologist.
Symptoms of hypogonadism in women
In women, hypogonadism leads to the following disorders:
- uterine hypoplasia;
- development of amenorrhea;
- infertility;
- hypoestrogenism.
One type of secondary hypogonadism in women is hyperprolactinemic hypogonadism. This is a neuroendocrine syndrome associated with excessive secretion of the hormone prolactin by the anterior pituitary gland and is accompanied by a number of endocrine and somatogenic disorders. Hyperprolactinemic hypogonadism is characterized by pathological galactorrhea, menstrual dysfunction, hirsutism, and infertility in women.
Also, this disease can provoke other abnormal conditions caused by acute estrogen deficiency. Otherwise, the symptoms directly depend on the stage of the pathology and the individual characteristics of the female body.
For example, the congenital form of the disease is accompanied by the absence of menstruation. A woman has insufficient development of secondary sexual characteristics against the background of a predominance of moderate hair growth in the pubic area.
However, the most dangerous condition that accompanies hypogonadism is amenorrhea. This disorder often worsens during puberty. In this case, amenorrhea can be primary or secondary. In the first case, the absence of menstruation is observed throughout life.
Menopause and hypogonadism. The connection with secondary amenorrhea has certain characteristics. Such women initially have a stable menstrual cycle, but under the influence of certain factors they develop specific symptoms. These include hot flashes, excessive sweating, and mood swings.
How does hypogonadism manifest in women (symptoms)?
- Irregular menstrual cycle and amenorrhea;
- The genitals do not fully develop during puberty;
- Hair growth is insufficient for a particular age;
- Fat deposits are distributed according to the male pattern;
- Underdevelopment of the mammary glands;
- Large buttocks;
- If the disorder is congenital, no secondary sexual characteristics are visible;
- Narrow pelvis;
- The secondary genital organs are not developed according to the patient’s age;
- Inverted nipples.
Sometimes bone abnormalities are noticeable in the form of short stature, curvature of the cervical spine, and curved ulnar articulation of the bones.
Symptoms
The main symptom of amenorrhea is the complete absence of the menstrual cycle. Girls often complain about excess weight, which is associated with hormonal imbalance in the body. Pain during amenorrhea may occur due to ovarian dysfunction.
In addition, representatives of the fair sex are diagnosed with increased testosterone levels. They complain of the following symptoms:
- increased sweating;
- rapid weight gain;
- intensive hair growth;
- the voice becomes rougher.
With secondary amenorrhea, doctors note the appearance of galactorrhea. Girls who are not pregnant begin to secrete milk. If the level of prolactin in the body increases, then doctors diagnose “secondary amenorrhea”.
Women who have not yet entered menopause experience unpleasant symptoms of menopause. They experience frequent and regular hot flashes, heart pain, and excessive sweating.
Symptoms of amenorrhea are accompanied by headaches, general weakness, fatigue, drowsiness and irritability. The absence of menstruation during amenorrhea is a signal to consult a doctor. If menstruation is not observed for three months, then it is necessary to perform a thorough diagnosis and eliminate the main cause of the failure.
Symptoms of hypothalamic amenorrhea
The causes of amenorrhea are very diverse, so after the first symptoms appear, you need to consult a doctor to eliminate the causative agent of the disease. The most common reason is the presence of various hormonal imbalances. When normal functioning of the hypothalamus is observed in a woman’s body, it secretes all the necessary substances to stimulate the pituitary gland. This organ affects the functioning of the ovaries, stimulating the normal cycle of egg maturation.
If the fair sex has problems with the endocrine system, then they may encounter the following problems:
- The influence and regulation of the normal functioning of the hypothalamus is reduced.
- The amount of hormones in the body changes.
- There is an imbalance of thyroid hormone. Its insufficient or excessive amount leads to various disorders in the menstrual cycle. Girls may notice the following symptoms: decreased frequency and irregularity of menstruation.
- The functioning of the adrenal glands is disrupted, because in the fair sex the content of the male hormone in the body increases.
Symptoms of hypothalamic amenorrhea are associated with the origin and duration of the disease. In most cases, the disease develops with regular intense exercise, frequent stressful situations, poor diet and rapid weight loss.
The main symptoms are absence of menstruation, weight gain, lack of pubic and armpit hair, increased blood pressure and osteoporosis.
Types of hypogonadism in women
Hypogonadism in women can be represented by three types: hypergonadotropic, hypogonadotropic and normogonadotropic.
Hypogonadotropic hypogonadism in women
In this condition, ovarian function is reduced due to the presence of disturbances in the functioning of the pituitary gland or hypothalamus. In this case, the ovaries produce insufficient amounts of hormones or do not produce them at all. If the functioning of the hypothalamus is disrupted, the production of gonadotropin-releasing hormone decreases, which, in turn, leads to the appearance of clinical symptoms of hypogonadotropic hypogonadism. This hormone is necessary for the normal functioning of the reproductive system and the production of the required amount of sex hormones.
Hypergonadotropic hypogonadism in women
In patients with this diagnosis, the amount of follicle-stimulating and luteinizing hormones in the blood is noticeably increased, premature ovarian failure, and pathologies of gonad development are noted. Ovarian function is reduced, as a result of which the body tries to compensate for the lack of hormones produced by producing pituitary hormones (gonadotropins), which stimulate the activity of the ovaries. The amount of estrogen in the blood is reduced compared to normal.
Normogonadotropic hypogonadism in women
This pathological syndrome is otherwise called hyperprolactinemia. The level of other hormones is generally normal, but Rokitansky syndrome manifests itself, which is amenorrhea due to uterine underdevelopment.
All of the listed types of hypogonadism should be treated only in conjunction with a doctor. It is not recommended to take any action on your own. Treatment tactics will be different, depending, for example, on whether hypogonadism is congenital or not.
Treatment
The essence of drug treatment for pathology is to artificially stimulate ovulation. For this purpose, a woman can be prescribed 2 groups of drugs. The first includes menopausal gonadotropins, the second includes gonadotropin-releasing hormone (GnRH) agonists. The effectiveness of such therapy can be assessed in advance based on the results of the luliberin test.
Note that all medications are prescribed to a woman by a gynecologist after a full examination.
If drug therapy is successful, the patient's ovulation is restored, allowing her to become pregnant again. Unfortunately, treatment of hypogonadotropic amenorrhea does not always achieve good results. Share:
Treatment of hypogonadism in women
If the patient is young, the doctor prescribes hormone replacement therapy, which involves treatment with drugs containing natural estrogens. If she experiences menstrual-like bleeding, the doctor recommends taking biphasic hormonal contraceptives (they must contain estrogens and gestagen). Women of late reproductive age, that is, those who have reached forty years, should also undergo treatment with hormones, but in this case monophasic agents are prescribed.
Hypogonadotropic hypogonadism in women: treatment
At the beginning of treatment for this pathology, doctors recommend eliminating the causes of the disease such as:
- Eliminate stress from a woman's everyday life;
- Normalize body weight by getting rid of excess weight;
- Avoid heavy physical activity for the body;
- Treat pituitary tumors.
The above measures can have a beneficial effect on a woman’s menstruation and fertility. Next, doctors usually prescribe estrogen-progestogen treatment in a cyclic mode. Estradiol and dydrogesterone are often used in combination.
Hypergonadotropic hypogonadism in women: treatment
To treat this pathology, doctors prescribe replacement therapy using female sex hormones, in particular ethinyl estradiol. Once menstrual bleeding occurs, oral contraception will need to be used to continue treatment. The drugs must contain estrogens and gestagen. The most famous are represented by Triquilar, Silest, Triziston, Diane-35.
How can women prevent the development of hypogonadism?
Maintaining a correct, healthy lifestyle, in which a woman regularly exercises, eats healthy food and gives up bad habits;
- Consultations with an obstetrician-gynecologist throughout pregnancy and registration at the antenatal clinic at the required period (before the twelfth week of pregnancy);
- Medical examination of the population;
- High-quality and timely elimination of infectious processes in the pelvic organs, as well as STDs.
It should be remembered that self-treatment of the disease can only cause damage to women’s health, therefore, if you suspect this disease, consultation with a specialist is necessary.
What consequences can hypogonadism lead to?
- Delayed sexual development of a teenage girl;
- Inability to get pregnant;
- Ovarian dysfunction;
- Poor development or hypoplasia of the internal genital organs.
What is amonerea?
So, amenorrhea in medical terminology is the absence of menstrual bleeding for several cycles. This is not a disease, but a conditional symptom, which in some cases is the norm, in others it is a sign of a woman’s reproductive function disorder.
It is customary to distinguish several types:
- true (when there are no cyclic changes in the ovaries, and the synthesis of female sex hormones is reduced);
- false (when the ovaries function normally, the hormone levels are also normal, but bleeding does not occur);
- postpartum (is the norm, associated with the restoration of reproductive function after pregnancy);
- pathological
In this case, amenorrhea is usually indicated in the absence of menstruation for more than 3 months. And pathological, in turn, is divided into:
- primary;
- secondary;
- etiotropic.
Primary is when there is no menstrual bleeding before the age of 14 years, or up to 16 years in the presence of other secondary signs of puberty in the female body. Secondary is when there is no menstruation, but in previous cycles they occurred normally and on time. Etiotropic occurs against the background of hormonal imbalance (after all, the course of the entire menstrual cycle is regulated by sex hormones).
Amenorrhea is further divided into degrees:
- Grade 1 – no bleeding for up to a year;
- Grade 2 – no bleeding for 1 to 3 years;
- Grade 3 – no bleeding for over 3 years.
Hypogonadism and pregnancy
Hypogonadism and pregnancy: how are these two concepts related?
If a woman is diagnosed with gonadotropic insufficiency of the pituitary gland, represented by hypogonadism, in order to become pregnant she will need to use replacement therapy, which will allow her to achieve follicular growth in the ovaries and the ovulatory process.
Hypogonadotropic hypogonadism in women and pregnancy (as well as hypergonadotropic) and pregnancy are compatible concepts if proper treatment is carried out in time, which is divided into two stages: preparation and induction of ovulation.
The preparatory stage involves the use of hormone replacement therapy. This treatment lasts from three months to a year. Ovulation induction is carried out using gonadotropins. How successful the treatment was is assessed using ultrasound. Within normal limits, follicles with this treatment should grow by 2 mm per day. During further diagnosis, ultrasound is used to observe whether the dominant follicle is absent. If so, ovulation has occurred (once confirmed, the luteal phase is maintained) and pregnancy will be possible. Doctors prescribe an ultrasound at 2 weeks of pregnancy to confirm pregnancy. The photo taken during the ultrasound does not yet show what the embryo looks like and what its vital signs are. But if you wait until the sixth week of pregnancy, the doctor can already hear the baby’s heartbeat.
Should amenorrhea be treated?
Treatment of amenorrhea is carried out only when it is classified as a pathology and a disorder in the functioning of the reproductive system of the female body. For example, in the case of postpartum amenorrhea, no therapy will be required. This is a feature of the female reproductive system - after the birth of a child, their body “restores” its usual functionality within 3-24 months. This is also due to lactation (breastfeeding), in which the level of hormones differs from those characteristic of the normal menstrual cycle.
Article on the topic:
Symptoms and treatment of hormonal imbalance in women
There is also the concept of physiological amenorrhea. This is the absence of menstruation before puberty or after menopause (after 45 years). Naturally, such amenorrhea cannot be treated, since it is not a violation of the reproductive system. It should be borne in mind that puberty and menopause are purely individual physiological parameters. For each woman, these periods occur at different ages, and 14 and 45 years are the average value.
But if menstruation does not occur after puberty, and previously it proceeded normally, then this is a malfunction of the reproductive function. In this case, medical consultation is required. Girls under 16 years of age may also not have menstruation due to false amenorrhea. This is when the ovaries function normally, the hormonal levels are also stable, but bleeding does not occur due to pathology in the structure of the reproductive system itself.
Most often, this is a violation of the physiology of the structure of the organs of the reproductive system, due to which menstrual blood accumulates, but does not come out. In most cases, such a “defect” is eliminated surgically.
It is worth mentioning separately about amenorrhea, which occurs after menarche - the first menstrual bleeding in girls aged 12 - 14 years (when puberty occurs). A delay in the subsequent menstrual cycle in this case can take from 2 to 12 months and this is the norm. Why is this happening? Up to the age of 16-18, puberty is still in the active stage, and at the same time the usual hormonal background of the female body is established. Disruptions in the menstrual cycle are the norm for this period.
So how to treat amenorrhea? If it occurs, you should consult a gynecologist as soon as possible and, if necessary, undergo an ultrasound (ultrasound examination, in this case, of the pelvic organs). You will also need to donate blood for tests (to determine the level of sex hormones).
Causes
Etiology • Primary amenorrhea •• Gonadal damage: Turner syndrome, testicular feminization syndrome, resistant ovarian syndrome, developmental anomalies of the uterus and ovaries •• Extragonadal pathology: hypopituitarism, hypogonadotropic hypogonadism, delayed menarche, congenital adrenal hyperplasia •• Impaired patency of the vaginal opening, vagina , cervical canal and uterine cavity • Secondary amenorrhea •• Psychogenic amenorrhea (stress) •• Hypothalamic form - amenorrhea due to weight loss •• Hypothalamus - pituitary form ••• Hyperprolactinemia - functional and organic forms ••• Hypogonadotropic ••• Postpartum hypopituitarism ( Scheen's syndrome) ••• Discontinuation of oral contraceptives ••• Medicines: oral GCs, danazol, gonadotropin-releasing hormone analogues, chemotherapy drugs ••• Decompensated endocrinopathies: diabetes, hypo- and hyperthyroidism •• Adrenal form ••• Post-pubertal adrenogenital syndrome ••• Virilizing adrenal tumor ••• Ovarian form ••• Ovarian wasting syndrome ••• Refractory ovarian syndrome ••• Virilizing ovarian tumors •• Uterine form ••• Asherman's syndrome (intrauterine synechiae) ••• Endometritis of specific etiology.
Risk factors • Physical overload • Eating disorders (including overeating and starvation) • Psycho-emotional stress.
Genetic aspects. There are many inherited diseases accompanied by amenorrhea.