What is a bicornuate uterus
A bicornuate uterus is an anomaly in the structure of the female reproductive organs that occurs rarely; the most common defect (0.1 - 0.5%) is a bicornuate uterus, characterized by doubling, in which the two cavities of the body of the organ are not completely separated. The body of the uterus is divided into two horns, which are connected at the bottom.
- Causes
- Classification
- Symptoms
- Diagnostics
- Treatment
- Forecasts
- Prevention
The defect is classified as an anomaly in the development of the paired Müllerian canal, which forms in the fetus at the beginning of pregnancy (10–14 weeks). The duct is the basis for the further intrauterine development of the uterus, vagina, and fallopian tubes in a female fetus.
The paramesonephric (Müllerian) duct consists of two parts fused in the distal (far) section. If intrauterine development is disrupted (underdevelopment of one part of the duct, the impossibility of merging its lower parts), uterine defects develop.
It is possible to develop a bicornuate saddle uterus, partial bifurcation, or a bicornuate uterus with a septum. In some cases, the pathology is combined with other abnormal forms of the vagina, cervix, urinary tract, and kidneys.
The first signs of a bicornuate uterus
During normal organogenesis, a woman's uterus forms a triangular shape. Any septations or structural abnormalities are an abnormality.
Clinical signs of pathology are nonspecific. A defect can be reliably detected only by the results of instrumental studies.
A woman can suspect problems in the field of gynecology on her own. Prerequisites for this may include disruptions in the menstrual cycle, difficulties with conception, and changes in the amount of discharge. However, these signs may also indicate other diseases, so an ultrasound scan and consultation with a specialist are extremely necessary.
Causes of a bicornuate uterus
The exact causes of a bicornuate uterus have not been established. An anomaly is formed in the embryo during intrauterine development under the influence of unfavorable factors:
- intoxication (poisoning with alcohol, medications, drugs, chemicals, toxic emissions into the environment);
- constant psycho-emotional stress of a woman during gestation;
- injuries;
- diseases of the endocrine system;
- exposure to pathogenic microflora (viruses, bacteria, fungi, parasites), infection at the beginning of pregnancy;
- severe toxicosis of a pregnant woman;
- hypoxia (oxygen deficiency) of the fetus;
- severe deficiency of vitamins and microelements.
A hereditary factor and chromosomal abnormalities in the mother cannot be excluded.
Classification
The bicornuate uterus is classified according to the type of cleavage:
- Complete separation - the septum extends from the fundus of the uterus to the internal os, forming two isolated horns. Sometimes the cleavage is so pronounced that two separate niches are formed, like two closely spaced queens. Is it possible to get pregnant with this type of anomaly? Yes, in this case, pregnancy can develop and proceed without problems in one of the niches.
- Incomplete separation - a shallow opening is formed between the horns in the upper third of the organ. The horns are the same in size and shape. The cavity is divided by a partition, which can be of different lengths.
- With the saddle-shaped (arched) version, the shape of the uterus resembles a saddle - this is a depression at the bottom of the organ. Pregnancy is possible, but miscarriage occurs, since the saddle shape of the uterus leads to malpresentation of the fetus.
These are the three main types of bicornuate uterus. There is also a double body of an organ with a common neck or with a double neck, with atresia (fusion) of the internal cavity, atresia or atrophy of one horn.
Types of bicornuate uterus photo.
Bicornuate uterus and pregnancy
- Ionizing radiation that affects the body of a pregnant woman and fetus - radiation, x-rays. As a result of this effect, the processes of transfer of genetic material (chromosomal DNA) between dividing cells are disrupted.
- Infectious pathology of a pregnant woman, in which pathogenic microorganisms can enter the developing fetus and lead to various malformations - the most dangerous in this regard are toxoplasma, Epstein-Barr virus, and chlamydia.
- The impact of various chemical compounds on the body of the developing fetus, which have aggressive properties and have a damaging effect on its cells - such substances include some aromatic hydrocarbons (benzene), salts of heavy metals. During pregnancy, taking certain medications (antibiotics, chemotherapy), alcohol, smoking and drug use can also lead to fetal malformations.
These reasons can become a causative factor in malformations of other fetal organs (heart defects, nervous system defects).
A pregnant woman needs to remember that Toxoplasma is transmitted from cats, therefore, during pregnancy, in order to prevent the development of a bicornuate uterus in the future girl (or other malformations), it is necessary to limit contact with pets as much as possible.
After identifying the defect, determining the type, severity and size of the septum in its cavity, the gynecologist determines further therapeutic tactics. In the case of incomplete bicornuate uterus and saddle uterus, active surveillance is carried out, especially during pregnancy. In case of complete bicornuity, metroplasty is recommended - a surgical intervention in which the septum is excised to form one cavity.
- Miscarriage at various stages of pregnancy.
- Isthmic-cervical insufficiency, which is characterized by miscarriage and premature birth.
- The formation of a breech presentation of the fetus, which significantly complicates the process of physiological labor.
- Complicated course of childbirth.
If a bicornuate uterus was diagnosed during pregnancy, childbirth in most cases is not carried out physiologically, but a cesarean section is performed.
To prevent the development of a bicornuate uterus in a daughter, an expectant mother, it is necessary to make maximum efforts aimed at preventing the effects of various negative environmental factors on her body. This will also contribute to the birth of a healthy child and prevent the development of defects in other organs and systems.
In most cases, with this anatomical defect, gynecological observation is carried out; during pregnancy, various measures are taken to prevent its interruption, and a caesarean section is used to give birth to a child.
A bicornuate uterus is a structural anomaly in which the body of the organ is incompletely divided into two cavities. The bicornuate uterus resembles a slingshot in appearance. Along with disturbances in the formation of the uterus, a woman may be diagnosed with concomitant pathologies of the kidneys, vagina, cervix or urinary tract.
A bicornuate uterus can function normally as a single organ, but in some cases both horns work independently - the uterine cycle is formed in each of them and pregnancy is possible. In any case, changes in the normal structure of the uterus make it difficult for the egg to attach, carry the fetus and reduce the likelihood of pregnancy.
The abnormal organ is shaped like a jester's cap, which is often depicted in children's fairy tales. The internal cavities of the two horns have a common place where they meet.
In the presence of such pronounced external changes, the structure of the uterus and its layers is usually not disturbed. The walls of the organ and all its layers are able to fully function and fulfill their purpose. Cases where one of the horns atrophies or does not reach sufficient development are rare.
This congenital anomaly affects the anatomical structure due to which a horn-shaped uterus is formed (two horns or two niches), a single cavity splits, and a septum forms inside the organ. A woman with a heart-shaped uterus will suffer from abnormal uterine bleeding (menstruation), dysmenorrhea, infertility or miscarriage.
- probing, MRI;
- laparoscopy;
- hysteroscopy;
- hysterosonography;
Causes
Bicornuate uterus in the fetus can be caused by various factors in the first months of gestation. During this period, the child’s organs are formed and formed, so any negative effects on the body can cause the development of abnormalities. Teratogenic factors that can cause dissection of the uterine fundus include:
- any type of intoxication: drugs, alcohol, nicotine, chemical agents, medications;
- psychological trauma during pregnancy;
- avitaminosis;
- endocrine pathologies: thyrotoxicosis, diabetes mellitus;
- mother's heart defect.
Infectious agents, for example, pathogens of influenza, measles, toxoplasmosis, rubella, syphilis, etc., can damage the embryo. Separation of the uterus can occur due to chronic fetal hypoxia, during pregnancy with toxicosis. The bicornuate structure in some cases is sometimes combined with other anomalies, usually defects of the urinary system.
Symptoms
The bicornuate anomaly does not have pronounced clinical signs. Uterine bifurcation may be accompanied in some cases by uterine bleeding and algomenorrhea. Cases of spontaneous abortion (miscarriage) or infertility have been recorded. This does not mean that there is no chance of giving birth and surviving pregnancy without complications.
Miscarriages occur, as a rule, in the first trimester; at this stage, embryo growth is hampered due to lack of blood supply and the small volume of the uterine horn cavity. With bicornuate anomaly, other symptoms also appear:
- pathology of the location of the placenta (low or previa);
- placental abruption, bleeding;
- isthmic-cervical insufficiency;
- premature birth;
- postpartum hemorrhage;
- breech presentation of the fetus;
- disturbances in the contractile activity of the uterine muscles.
A uterus with a bicornuate anomaly has pronounced physical signs; the organ cavity is divided into two parts. This rudimentary process can fuse at different levels of the lower section. In gynecology, the size of the cleft is used in the following classification of bicornuate anomaly:
- full;
- incomplete;
- saddle-shaped
Full
A bicornuate anomaly of this type is characterized by the separation of the cavities in different directions, starting with the uterosacral ligaments. The angle between the horn “pockets” may differ from case to case. The separation is pronounced; two separate niches are formed, which are located in close proximity to each other. Pregnancy can proceed normally in one part of the uterus.
Incomplete
The separation may be partial. Incomplete duplication of the uterus is externally distinguished by the splitting of the internal space by only a third with a shallow opening between the two horns. The horny anomaly on both sides is the same size. Pregnancy can proceed normally in one of the “pockets”; there have been cases of conceiving twins. Both fetuses are located in a separate uterine horn.
Saddle
A bicornuate uterus of this type has a slight depression in the bottom (upper part) that visually resembles a saddle. If there are accompanying defects, there is a possibility of miscarriage, but conception with this type of anomaly is possible. If a girl has a narrow pelvis with this pathology, the possibility of abnormal fetal position cannot be ruled out. In such cases, it is necessary to perform surgery during childbirth (caesarean section).
To answer the question of what a bicornuate uterus is in women, you need to be aware of its structure and shape. Normally, the uterus is a muscular organ with a single cavity inside. In this cavity, the fetus is borne during conception. However, with bicornus, a bifurcation of the intrauterine space into two parts is observed. The degree of complexity of the anomaly and the level of its impact on conception and gestation depend on the characteristics of such bifurcation.
There are three degrees of splitting of this organ into cavities:
- Complete - pronounced division into two independent uteruses. They may have a common neck that passes into the vagina, or they may have separate necks and are supplemented by a partial vaginal septum.
- Incomplete - division occurs only in the upper third of the organ, and its lower part forms a single cavity.
- Saddle-shaped - with this anomaly, the uterus has one cavity, but its upper part is distinguished by a strong depression directed inside the organ.
The listed degrees of complexity determine what a woman’s bicornuate uterus looks like and how severe the consequences of this deviation can be.
- lack of blood supply to the embryo due to the failure of the placenta to perform all its functions;
- pathological placement of the placenta leading to its detachment;
- cervical insufficiency;
- impaired contractility of the organ muscles;
- breech presentation of the child, requiring surgical intervention during childbirth.
In addition to the above points, the available cavity size should also be considered. After all, dividing the uterus into two parts significantly reduces the volume of each of them, so the growth of the embryo will be hampered by the limited free space.
The problem of placental insufficiency is solved in a clinical setting by prescribing drugs that accelerate metabolism. Such medications improve blood flow and accelerate the absorption of beneficial microelements through the placenta. If a woman has problems with muscle contractility (increased uterine tone, threatening miscarriage), doctors recommend regular use of antispasmodics under the supervision of a specialist. But the best way to solve the problem is to eliminate the anomaly in a timely manner to ensure a normal pregnancy.
Symptoms of a bicornuate uterus
Normally, the uterus resembles a triangle with a base and a cavity inside. With an anatomical anomaly, the organ looks like a cap with two halves diverging to the sides. These cavities can communicate with each other and open into the cervical canal separately or have a common exit into the cervical canal. The angle of divergence of the cavities is different in each case, which depends on the development of the external walls and the length of the septum. The layers of the horn walls are fully developed in most cases, but asymmetry also occurs when one horn is underdeveloped or overgrown.
A bicornuate uterus may not give any clinical manifestations, and even often gestation and childbirth with a bicornuate uterus proceed without complications. In some women, pregnancy ends in spontaneous abortion with a bicornuate uterus, which is due to the small amount of space for fetal development in one horn and insufficient blood supply.
A characteristic symptom of a bicornuate uterus is menstrual disorder. Most often, bleeding, prolonged and painful periods are observed with a deterioration in general well-being, excitability of the nervous system, dyspeptic disorders, headaches, decreased performance, and the addition of infections.
The pain of menstruation with a bicornuate uterus is caused by an enlargement of the organ, in which the uterus presses on neighboring tissues and nerve plexuses. Bleeding and an increase in the duration of menstruation are due to the fact that the volume of a bicornuate uterus is larger than that of a normal one, so more endometrium is rejected, but its evacuation is difficult. In horizontally located niches, blood can stagnate, which causes severe discomfort.
If a woman does not have vaginal abnormalities, the bicornuate uterus does not affect her sex life and libido. A woman experiences during intimate intimacy all the same sensations as with a normally developed organ.
How to get pregnant with a bicornuate uterus?
If pregnancy does not occur or is not delayed, then the above-described operation helps to experience the joy of motherhood, which, however, cannot fully guarantee that the organ restored in this way will perform the functions of a healthy one, because during pregnancy it may not cope with the load and simply rupture. In addition, there remains a risk of infertility (now secondary), due to the development of postoperative adhesions, so even an operated bicornuate uterus during pregnancy remains the subject of close attention by gynecologists. But it should be noted that the anomaly is not always the cause of infertility and miscarriage.
Quite often, pregnancy occurs without problems, and even goes “without a hitch” if the cavity size is sufficient for the full development of the fetus. And a woman accidentally finds out about bicornuity after an ultrasound scan was performed to determine the gestational age during registration. It happens that childbirth proceeds without complications and the postpartum period without “expected” bleeding, therefore, as they say, “one at a time is not necessary” and there is no need to despair in advance, however, you should be aware of possible troubles in order to help the doctor prevent them. Thus, this pathology during pregnancy can pose a threat:
- the development of isthmic-cervical insufficiency, in which the isthmus and cervix lose the ability to withstand the load caused by the increase in the size of the pregnant uterus and open. The result of this process is a spontaneous miscarriage, which is painless and has no warning signs, so the woman may not be aware of the changes occurring the day before;
- improper placement of the placenta with possible premature detachment or abnormal presentation of the fetus (pelvic, transverse or oblique), which complicates childbirth with a bicornuate uterus, posing a threat to the baby’s life;
- premature birth, especially with complete bicornus, therefore, in order to avoid unwanted complications, in order to save the life of the child, at a period of 28 weeks, if there is a threat of spontaneous abortion, a caesarean section is performed routinely;
- violations of the contractility of the muscular layer of the organ;
- bleeding in the postpartum period.
Of course, during pregnancy no one will treat bicornuate pathology, and all the doctor’s efforts, as a rule, will be aimed at preventing complications of this congenital defect.
Knowing about her anomaly, a woman in such a crucial period should be especially vigilant and regularly attend an antenatal clinic, because, as mentioned above, she may not even suspect that a spontaneous miscarriage is beginning, since the uterus is in a calm state (not in good shape), painful does not reveal its feelings.
Obviously, a bicornuate uterus is more frightening by its name and is not such a hopeless option that prevents a normal pregnancy, however, it is also obvious that a lot depends on the woman. Ultrasound diagnostics, which has already become commonplace and familiar, in most cases can promptly identify this congenital pathology and thus prevent its complications, so visits to the doctor should not be avoided, because a woman may know almost nothing about herself. And if he knows, he will always find a way to prepare for the vicissitudes of fate. But it’s better to do this with the help of a gynecologist.
Video: “What does a bicornuate uterus with a septum look like?”
Diagnostics
The defect is discovered accidentally during examination of a pregnant woman or during a preventive gynecological examination. Bimanual examination can detect fundal deformation (if the defect is significant), the presence of a septum, and a double neck.
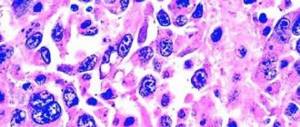
Clinical signs of the pathology are absent or similar to other diseases of the female reproductive system, therefore reliable methods are used to confirm the diagnosis:
- Transabdominal or transvaginal ultrasound examination - evaluates the anatomical structure of the organs of the urinary and reproductive systems. 3D scanning is used more often, but with minor deformations the pathology may not be noticed, it all depends on the experience of the diagnostician.
- X-rays can determine the outer boundaries of the uterus, but cannot determine the type of abnormality.
- Hysterosalpingography is an x-ray of the genital organs with contrast, which allows you to evaluate the uterine cavity and tubal patency. It is more often used to identify the causes of infertility, which is possible with a bicornuate uterus.
- Hysteroscopy refers to therapeutic and diagnostic minimally invasive surgical techniques. With the help of endoscopic examination, abnormalities in the structure of the organ, the cause of uterine bleeding, polyps and submucosal fibroids are identified. The procedure allows you to assess the condition of the endometrium.
- Laparoscopy is a therapeutic and diagnostic gentle surgical technique that can be used to detect and remove polyposis and cystic formations, and identify structural defects of the reproductive organs, kidneys, and urinary tract.
- MRI or CT - determine the shape of the organ, the structure of the walls, and identify anatomical anomalies.
In diagnostics, it is important not only to make the correct diagnosis, but also to assess the functionality of the reproductive system, the likelihood of pregnancy, and the prospects for surgical treatment.
Hysterosalpingography photo.
Diagnosis of a bicornuate uterus
1. Routine gynecological examination - as a rule, an anomaly in the structure of the uterus can be determined by palpation. However, it is difficult to determine exactly the nature of the change. 2. Ultrasound is the most informative method, in which most often the nature of the change can be determined quite accurately. 3. Hysteroscopy and hysterosalpingography - you can not only visually examine the uterine cavity and assess its condition, but also introduce an X-ray contrast agent, and use an X-ray to determine the doubling and its shape.
Metrosalpingogram for a bicornuate uterus
4. MRI is a rather expensive method. Its use is permissible in extreme cases, when there are other goals in addition to identifying developmental anomalies.
Treatment of bicornuate uterus
In the treatment of malformations of the uterus and appendages, it is important to both eliminate the anomaly and preserve reproductive function. Indications for surgery for bicornuate uterus:
- repeated early miscarriages;
- infertility;
- history of stillbirths;
- hematometra (collection of blood in the uterus).
Treatment tactics are selected individually. Today they use minimally invasive technologies. The most commonly used reconstructive method is metroplasty, which is performed:
- with removal of one horn;
- in removing a complete septum;
- with excision of an incomplete septum;
- in partial excision of the uterine wall and subsequent formation of the fundus.
Correction of the septum is carried out using a gentle, simple operation - hysteroscopic metroplasty. The procedure is as follows: during hysteroscopy, the walls of the uterus are stretched using an isotonic solution, then the necessary manipulations are carried out with optical scissors.
To evacuate pathological fluid or blood clots, hysteroresectoscopy is used, which allows electrodes to cut tissue of different thicknesses. With this option, the operation time is significantly reduced and the risk of complications is minimized.
Metroplasty is performed laparoscopically (surgical access through small holes in the abdomen) or laparotomy (surgical access through an incision in the peritoneum). After a successful operation, an intrauterine contraceptive device is installed for a period of 6–8 months. You can plan a pregnancy after 8–9 months.
Successful metroplasty can reduce the risk of complications during gestation from 85% to 30%. In many cases, surgery eliminates the cause of infertility. IVF increases the chances of pregnancy with a bicornuate uterus, especially if the deformation is mild. If bicornus is combined with other anomalies of the genitourinary organs, IVF becomes the only chance to get pregnant.
Are there any peculiarities with a septum in a bicornuate uterus?
The possibility of conception, the course of pregnancy and the risk of complications depend on how exactly the anomaly formed. The main role here is played by the degree of separation of the cavities by the partition; on this basis they differ:
- with a partition, when both cavities are completely separated from each other;
- incomplete bicornuate uterus, in which the septum leaves a gap between the cavities;
- saddle-shaped, when the cavities are practically not separated, and there is a small depression in the organ.
The maximum risk for pregnancy is a bicornuate uterus with a septum, since the embryo can attach itself to it.
If an ultrasound examination reveals an incomplete septum, then gynecologists use non-intervention tactics until complications arise. Many women with this pathology successfully give birth without any complications.
If there is a complete septum in the uterus, there is a high risk of pregnancy fading, especially if the embryo is attached to it. This is explained by the fact that the septum is devoid of blood vessels, so the fetus is not able to receive normal nutrition.
Watch the video about the features of the septum in the uterus:
Forecasts
The most favorable prognosis is the saddle-shaped form of the anomaly. The structural defect is usually weakly expressed, the uterine cavity is deformed insignificantly or not deformed at all. The likelihood of conception with this type of defect is higher than with others.
With atresia or atrophy of one horn, medical abortions are dangerous, which lead to scar tissue changes, which can cause infertility.
During gestation, with a bicornuate uterus, the following complications are possible:
- low placement of the placenta;
- abnormal placenta previa;
- premature placental abruption;
- breech or transverse presentation of the fetus;
- isthmic-cervical insufficiency (impaired opening of the cervix);
- premature birth;
- postpartum bleeding.
If the fertilized egg is attached to the atrophic horn, the horn will most likely rupture with intra-abdominal bleeding. The clinic resembles the course of an ectopic pregnancy. If the horns are full and the volume of the cavity is sufficient, usually the course of pregnancy is normal and ends with childbirth.
Defects of the Müllerian canal do not affect the development of the ovaries, therefore, in teenage girls, menarche (first menstruation) occurs on time, and there are no gross hormonal abnormalities.
Features of a bicornuate uterus
This developmental anomaly occurs in no more than half a percent of women, but nevertheless, among all congenital abnormalities in the structure of the main female organ, it is the most common.
Bicornus is formed in the embryo at 10–14 weeks of development; as a result of this process, its cavity is divided into two niches. In most cases, when the uterus is divided into two horns, one vagina and one cervix are preserved. Sometimes they can also be separated by a partition. One of the cavities may remain in its infancy, and if the fertilized egg attaches in this section, as it grows, the horn may rupture and bleeding may begin.
If both cavities develop normally, then a normal pregnancy can occur in each horn, and childbirth will take place without complications.
The reasons for the formation of a bicornuate uterus in the embryo may be the following negative factors:
- intoxication of the expectant mother’s body with alcohol, drugs, nicotine, and potent drugs;
- poor nutrition, lack of vitamins;
- problems with the endocrine system, for example, diabetes or thyroid disease;
- inflammatory processes of infectious etiology;
- diseases of the cardiovascular system and others.
Also, the cause of the development of the anomaly can be severe toxicosis in the first weeks of pregnancy and fetal hypoxia.
Depending on the nature of the division of the cavity, complete, incomplete and saddle-shaped bicornus are distinguished.
We recommend reading the article about the saddle uterus. From it you will learn about the structural features of the organ, symptoms and diagnosis, ways to solve the problem, as well as pregnancy and childbirth with an anomaly. And here is more information about how the uterus changes during pregnancy.
Prevention
To minimize the risks of developing anatomical abnormalities in the fetus, the expectant mother should eliminate bad habits, eat rationally, be moderately active, not be overloaded physically and psychologically, take more frequent walks in the fresh air and go to nature.
Management of pregnancy with a bicornuate uterus in a patient requires prevention of potential complications. In the early stages, bed rest, therapy with antispasmodics, hemostatics, sedatives, and gestagens are indicated. If there is a threat of failure in the later stages, a cesarean section is performed at 26–28 weeks.
What to do?
If you think you have a bicornuate uterus
and symptoms characteristic of this disease, then a gynecologist can help you.
We wish everyone good health!
Diseases with similar symptoms
Transversoptosis (matching symptoms: 5 out of 9)
Transversoptosis is a change in the anatomically prescribed position of the large intestine. As the pathology progresses, the transverse colon prolapses: on x-rays it will have the shape of the letter “V”.
Did you like the article? Share with friends on social networks: