What is Brugada syndrome?
Brugada syndrome is a set of genetic disorders that lead to pathological changes in the rhythm and conductivity of cardiomyocytes and increase the likelihood of sudden death from cardiac arrest. It was first diagnosed and described in 1922 by cardiologists the Brugada brothers.
It has been established that the pathology is a hereditary condition. Specific culprit genes have also been identified. The disease is more often diagnosed in men than in women. The disease develops at different ages, but typical symptoms clearly manifest themselves at 30–45 years of age.
Forecast
The prognosis for Brugada syndrome is unfavorable - 11% of patients die at a young age from sudden cardiac death.
Installation of a cardioverter-defibrillator has a positive effect on the quality of life of patients. They need to see a heart surgeon annually and have the device replaced every 4-6 years.
People with Buragada syndrome should lead a healthy lifestyle, eat a balanced diet, avoid stress and avoid extreme activities. These measures help reduce the likelihood of tachycardia attacks.
Symptoms of pathology
Depending on the current clinical symptoms, it is customary to distinguish two types of the syndrome:
- Syncopal. Characterized by loss of consciousness.
- Non-syncopal. It is almost asymptomatic, there are no typical complaints.
There is a relationship between clinical signs and the degree of sodium channel damage:
- if less than a quarter of the total number of channels is damaged, heart rate deviations are recorded only after the introduction of blocking substances;
- with a more extensive lesion, the attack may end in sudden death.
The typical clinical picture of a heart attack includes several characteristic symptoms:
- sudden deterioration of condition;
- dizziness;
- state of prostration;
- painful tremors in the heart area;
- black dots in the field of vision;
- increased sweating;
- short loss of consciousness (no longer than 30 seconds);
- convulsions (not excluded).
The development of an attack is preceded by any stress (both physical and emotional), increased body temperature, and alcohol intake. It occurs at night and in the evenings; it occurs extremely rarely during the day (no more than 13% of all diagnosed cases).
After the condition has stabilized, the person fully comes to his senses. A state of clinical death develops in 11% of patients. The outcome depends on the implementation of the necessary resuscitation actions.
There are certain ECG signs of Brugada syndrome. These are recognized as:
- Complete/partial blockade of the right bundle branch.
- Signs of depolarization disorder.
- Elevation of the ST interval by more than 1.5 mm. The formation of a line in the form of a vault indicates the syncopal form of Brugada syndrome; with the formation of a “saddle” we are talking about the non-syncopeal variety.
Important ! Characteristic changes are recorded only in the right chest leads.
In a child, diagnosing the syndrome is difficult, since typical changes are visible on the electrocardiogram only after reaching 5 years of age.
Regular ECG monitoring allows you to identify characteristic signs of the disease.
- The use of 24-hour monitoring makes it possible to monitor the transition of a healthy myocardial rhythm to ventricular tachycardia.
- Taking an electrocardiogram against the background of intravenous administration of sodium channel blockers. A sign of cardiopathology is the development of paroxysmal contractions of the ventricles. The test is carried out exclusively in a hospital setting.
Important ! If the cardiogram does not show abnormalities, despite regular fainting, then it needs to be redone. In this case, the right electrodes are installed above the normal zone by two ribs.
Consequences
After all of the above, it becomes clear that Brugada syndrome has an unfavorable prognosis. Death occurs due to VF. The risk of death is the same for periodic and permanent changes in the ECG.
It is difficult to say anything specific regarding preventive measures that can reduce the risk of sudden death, especially when it comes to a genetic predisposition to the occurrence of this disease. However, it is important to understand that a healthy lifestyle and a good mood will help you not to focus on your illnesses, and can sometimes save your life.
Reasons for development
The main factor in the development of pathology is the mutation of genes responsible for the production of proteins, the main task of which is the delivery of sodium ions to cells.
Brugada syndrome is a genetic disease transmitted in an autosomal dominant manner. This means that if a modified gene is received by an infant from one of the parents - it does not matter whether it is the father or the mother - then cardiac pathology will manifest itself in any case.
The probability of developing the syndrome is described by a 1:1 ratio, i.e., the disease will be present in 50% of all infants born, one of whose parents is a carrier of the damaged gene.
Potential signs of cardiac pathology include:
- development of syncope (short unconscious states accompanied by a decrease in muscle tone, disruption of breathing and functioning of the cardiovascular system) of unknown etymology;
- unexpected cardiac arrest in someone close to you;
- diagnosing cases of paroxysmal ventricular tachycardia.
Causes
The causes of the disorder lie in the pathological work of sodium and calcium cardiomyocytes. Modern medicine has been able to identify six genes that, when damaged, cause the disease. Based on this, the following types of Brugada syndrome are distinguished:
- BrS-1 is considered the most common form and has been well studied. It occurs due to a mutation in the SCN5A gene, which also leads to various hereditary cardiac pathologies;
- BrS-2 is triggered due to the GPD1L gene;
- BrS-3 develops as a result of a breakdown of the CACNA1C gene;
- The BrS-4 form appears due to a mutation in CACNB2;
- BrS-5 appears due to a mutation in SCN4B;
- BrS-6 causes a defect in the SCN1B gene.
The HEY2, KCNE3, and SCN10A genes are also blamed for the appearance of the syndrome. But scientists cannot reliably prove their involvement. It also remains unknown why Brugada syndrome affects men more often than women.
Diagnosis of the syndrome
Brugada syndrome is a frequently encountered cardiac pathology in world medical practice. In Russia, the disease is detected relatively rarely, which is explained by the insufficient focus of doctors on differential diagnosis.
The examination must be performed in the following cases:
- a history of syncope, the cause of which remains unknown;
- the appearance on the electrocardiogram of changes typical of the Brugada phenomenon;
- the formation of at least one episode of polymorphic ventricular tachycardia;
- episodes of unexpected death of relatives from a heart attack.
Diagnostic examination includes:
- ECG study with and without the administration of drugs;
- Holter monitoring (daily recording of an electrocardiogram);
- genetic research.
Important ! The use of antiarrhythmics can provoke the development of an attack of ventricular tachyarrhythmia (ventricular fibrillation is possible). Therefore, such tests are carried out exclusively in a hospital setting, where emergency medical care can be provided.
Diagnostics
At the moment, the main ways to diagnose Brugada syndrome are:
- ECG with and without drug tests;
- Holter ECG;
- molecular genetic research.
The administration of antiarrhythmic drugs during pharmacological tests in such patients can cause ventricular tachyarrhythmia (up to ventricular fibrillation), therefore, according to the protocol, drug tests with antiarrhythmic drugs are carried out only in specialized rooms for electrocardiography and with staff fully prepared to provide emergency care. The following antiarrhythmic drugs may be used to perform such tests:
- Novocainamide 10 mg/kg;
- Gilurythmal 1 mg/kg;
- Flecainide 2 mg/kg.
Treatment
Treatment of Brugada syndrome largely depends on the type of genetic mutations present and the current clinical symptoms.
If the condition is accompanied by the development of attacks of ventricular tachycardia and other conditions that worsen the patient’s quality of life, then the patient is recommended to install a cardioverter-defibrillator. This technique is the only possible way to eliminate the clinical symptoms of Brugada syndrome.
A drug therapy regimen for cardiac pathology is under development. Patients are prescribed antiarrhythmic drugs to eliminate attacks of cardiac arrhythmia. Patients may be recommended class IA antiarrhythmic drugs. This:
- "Quinidine"
- "Amiodarone"
- "Disopyramide".
Taking medications from the group of antiarrhythmics belonging to groups I and IC is completely prohibited. This:
- "Aymalin"
- "Novocainamide"
- "Flecainide"
- "Propaphenone".
Medicines can initiate blocking of sodium channels, which, with such a diagnosis, provokes ventricular fibrillation.
Brugada Syndrome: The Latest Information from the Brugada Brothers
At the very end of August, JACC published an excellent clinician-oriented review of Brugada syndrome, two of the authors of which were the Brugada brothers. That is, this is information from the original source. Below I give a brief but most informative summary of my own production from this article (Josep Brugada, Oscar Campuzano, Elena Arbelo, Georgia Sarquella-Brugada, Ramon Brugada,
Present Status of Brugada Syndrome: JACC State-of-the-Art Review, Journal of the American College of Cardiology, Volume 72, Issue 9, 2020, Pages 1046-1059, https://doi.org/10.1016/j.jacc .2018.06.037. (https://www.sciencedirect.com/science/article/pii/S0735109718353622)
Brugada syndrome is a genetically determined defect, manifested by a peculiar ECG graphic, with a high probability of leading to ventricular fibrillation and sudden death in a structurally unchanged heart.
In 1992, this syndrome was first described based on data from 8 resuscitated patients with ventricular fibrillation and a peculiar ECG pattern. The syndrome was initially called right bundle branch block, persistent ST segment elevation, and sudden death syndrome. Since 1996, this syndrome has been called Brugada syndrome. It is likely that what is now called Brugada syndrome was described earlier. For example, in 1917, unexplained nocturnal death syndrome was described in the Philippines. In 1998, a connection between the syndrome and a genetic anomaly was discovered.
Men get sick 10 times more often. Testosterone matters: the syndrome is rare in children, because testosterone levels in girls and boys are similar. After castration in men, the graphics of Brugada syndrome may disappear. The estimated prevalence of the syndrome is 1:2000-5000. Brugada syndrome is responsible for 4-12% of all sudden deaths and 20% of sudden deaths in structurally normal hearts. In children, the syndrome is rare, probably masked and disavowed at an older age.
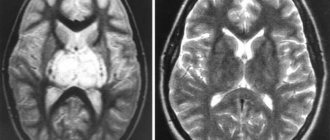
Diagnostic criteria: ST segment elevation in at least one of leads V1-V3 by 2 mm or more. Morphology type 1 (see picture). Type 2 is not a diagnostic criterion for Brugada syndrome, but increases the likelihood of having it. Characteristic graphics can be recorded at the 1st and 2nd intercostal spaces above V1-V3. In doubtful cases, it is recommended to record an ECG not only in standard leads, but also 1 and 2 intercostal spaces above. Characteristic graphics may appear or become more obvious after administration of ajmaline, procainamide or flecainide. The ECG graphics may not be completely typical.
Two types of ECG graphics for Brugada syndrome Type 1: the only diagnostic one for the syndrome. Straight or curved upward ST elevation of 2 mm or more, turning into a negative T. In at least one lead from V1-V3. Type 2. Not diagnostic for Brugada syndrome, but increases the likelihood of it and is an indication for a pharmacological test. Saddle-shaped downward curved ST elevation of 0.5 mm or more. In V1 T can be anything, in V2-V3 T is positive.
Additional criteria for Type 2:
A beta angle in the top figure equal to or greater than 58 degrees is the best predictor of transformation from Type 2 to Type 1 graphics in a pharmacological test. The length of the base of the triangle, the height of which is 5 mm from the point of maximum ST segment elevation. 4 or more mm at an ECG speed of 25 mm/s indicates Brugada syndrome, sensitivity 85%, specificity 96%.
Clinical manifestations: Syncope, seizures, agonal breathing during sleep. Polymorphic ventricular tachycardia and ventricular fibrillation. Sudden death. Most often during sleep or during fever. Fever may mask ECG signs. The average age of sudden death is 41+/- 15 years.
Pharmacological tests: Indications: any suspicion of a syndrome (for example, syncope or VF), Brugada syndrome type 2. The test is positive if type 1 graphics appear. Use intravenous administration of ajmaline, procainamide or flecainide. If unavailable, propafenone or oral flecainide can be used. Stop the test if frequent ventricular extrasystoles and more complex arrhythmias appear, as well as if the QRS expands more than 130% of the original duration. 25% of all tests are false negative. It is advisable to repeat the test with different drugs. Drug dosages are not described in the review. It is not clear how dangerous the tests are.
Who to treat? Risk stratification The obvious risk factor is syncope due to ventricular arrhythmia. In the absence of symptoms, there are no clear recommendations. Treatment is individualized. If EPS is positive, you can consider installing a cardioverter. A cardioverter is the most reliable method of treatment . Some patients undergo epicardial ablation, but long-term results are lacking and the effect is unclear.
Two types of ECG graphics for Brugada syndrome Type 1: the only diagnostic one for the syndrome. Straight or curved upward ST elevation of 2 mm or more, turning into a negative T. In at least one lead from V1-V3. Type 2. Not diagnostic for Brugada syndrome, but increases the likelihood of it and is an indication for a pharmacological test. Saddle-shaped downward curved ST elevation of 0.5 mm or more. In V1 T can be anything, in V2-V3 T is positive.
Defibrillator installation
Since taking drugs from the group of antiarrhythmic drugs practically does not bring the necessary therapeutic effect, the patient is recommended to install a special cardiac defibrillator. The operation is justified even in patients with asymptomatic cardiopathology. Surgical treatment reduces the risk of death from cardiac arrest by 89%.
A cardioverter-defibrillator is a miniature device placed in a medical metal box and installed subcutaneously in the left subclavian area. Its “filling” consists of an analyzer that evaluates the current rhythm of myocardial contraction, and a system that, if necessary, releases a discharge of electric current.
The device is equipped with electrodes that transmit and receive signals from the myocardium, passed through the coronary arteries, which are responsible for the blood supply to the organ.
The main functions of the device are:
- continuous assessment of the work of the heart muscle;
- interruption of the emerging rhythm disturbance using an electrical discharge;
- bringing the heart muscle contractions to a physiological norm;
- preventing complete cardiac arrest.
The service life of the device is no more than six years, then it must be replaced. The device is completely protected from external interference, i.e. does not react to radiation from household appliances.
Treatment of the disease
It is impossible to completely cure such a disease, but there are ways in which you can reduce attacks, and sometimes even prevent them altogether:
- Drug therapy. It will allow you to reduce and return to normal the work of the ST segment, improve heart function, and return the rhythm to normal (60% positive result).
- Installation of a defibrillator (provided that the medications did not give the desired effect). Features of the device are: assessment of heart function, prevention of disturbances and complete stop.
The study of SB continues, but no one knows how long it will take. That is why there are no specific methods of prevention, and treatment is symptomatic.
Complications caused by Brugada syndrome
The key problems that accompany this cardiopathology and worsen the prognosis of the outcome of the disease are severe complications:
- Ventricular tachycardia. Additional sources of excitation are located in the ventricles. Most often in the left cavity.
- Supraventricular tachycardia. Pathological foci are determined in the atria.
- Atrial fibrillation.
- Ventricular fibrillation.
Against the background of these pathological conditions, the patient may develop:
- Cardiac asthma. It is characterized by stagnation of blood in the pulmonary circulation, causing swelling of the lung tissue.
- Cardiogenic shock. A sharp impairment of the contractility of the left ventricle.
- Cerebral ischemia. Signs of the condition include blurred vision, dizziness, and shortness of breath.
- Sudden cardiac arrest. Most often it occurs at night, since attacks of tachycardia occur between 6 pm and 6 am.
Possible complications
The following complications occur with a disease such as Brugada syndrome:
- all types of tachycardia;
- cardiac asthma;
- cardiogenic shock;
- disorders in the brain;
- heart failure.
Installing a defibrillator will help avoid most complications and reduce the likelihood of death by 97%, provided that the patient is observed by a cardiologist and the device is changed in time, because its service life is six years.
Prevention as such does not exist. The patient remains under constant supervision of his attending physician, and as a preventative measure, the following recommendations must be followed:
- diet;
- avoid stressful conditions;
- avoid hypothermia and overheating;
- take arrhythmic drugs;
- do not consume stimulants (coffee, carbonated drinks);
- alcohol and smoking are prohibited;
- do not abuse physical activity.
All of the above will help reduce the number of attacks and reduce the risk of complications after them.
Diagnostic methods
Electrocardiography is one of the main and most effective studies of various heart diseases, including Brugada syndrome. This procedure can identify the disease, as a result of which timely measures will be taken to combat it. An electrocardiogram in Moscow can detect cases of RBBB and ST-segment elevation in the precordial leads. And this makes it possible to determine and accurately diagnose this syndrome.
Brugada syndrome is a hereditary pathology, so it behaves very insidiously. Signs of this disease appear on the ECG only from the age of five. However, there is a fact that the development of the disease cannot always be seen on electrocardiography.
It happens that signs of the disease appear on the ECG periodically, and this creates difficulties in determining an accurate diagnosis. However, in this case, the main determining factor will be the change in the ST segment, which rises in specific leads and has a completely different, dissimilar shape for a healthy cardiac organ. Thus, the doctor can see the form of SB in each specific case.
If, when undergoing an electrocardiogram, it is difficult for the doctor to determine the presence of the disease, then the patient is offered the same procedure, only with the use of a load. The patient is administered sympathomimetics, as a result of which all cases of SB previously detected will decrease. When novocainamide is administered, the manifestations, on the contrary, increase. In this case, the doctor has the opportunity to determine the correct diagnosis and prescribe effective treatment.
It is worth noting that the reason for the inability to detect Brugada syndrome on electrocardiography may be some medications that a person is taking at this moment. These can be psychotropic drugs, as well as blockers and various antiarrhythmic drugs. In this case, the specialist prescribes a repeat electrocardiogram after stopping taking these medications.